Abstract
Pediatric clinicians are on the front line for prevention of language and speech disorders. This review uses prevailing theories and recent data to justify strategies for prevention, screening and detection, diagnosis, and treatment of language and speech disorders. Primary prevention efforts rest on theories that language learning is the product of the interaction of the child’s learning capacities with the language environment. Language learning occurs in a social context with active child engagement. These theories support parent education and public programs that increase children’s exposure to child-directed speech. Early detection of delays requires clinician knowledge of language milestones and recognition of high-risk indicators for disorders. Male sex, bilingual environments, birth order, and chronic otitis media with effusion are not adequate explanations for clinically significant delays in language or speech. Current guidelines recommend both general and autism-specific screening. Sex, and environmental and genetic factors explain primary language and speech disorders. Secondary and tertiary prevention requires early identification of children with language and speech disorders in association with chromosomal, genetic, neurological, and other health conditions. Systematic reviews find that speech-language therapy, alone or in conjunction with other developmental services, is effective for many disorders. Speech-language interventions alter the environment and encourage children’s targeted responding to improve language and speech skills.
Introduction
Learning language seems like a monumental task for the young child. The world’s languages contain thousands of words that can be combined to convey an infinite number of meanings. Children are born without knowing which of the world’s languages they must learn. If born in Brazil, they must learn Portuguese; if born in the Philippines, they must learn Tagalog. If born in Belgium or Quebec, or into an immigrant or refugee family, they may need to learn two different languages simultaneously. Despite these challenges, most children acquire the fundamentals of language effortlessly in the toddler-preschool years, without formal instruction or explicit feedback. By age 5, they have a vocabulary of thousands of words; create sentences with complex grammatical features; differentiate literal from non-literal meanings, such as humor or metaphor; observe the social conventions of conversation; and apply language skills in the service of learning to read. By age 8, their speech sound inventory is mature.
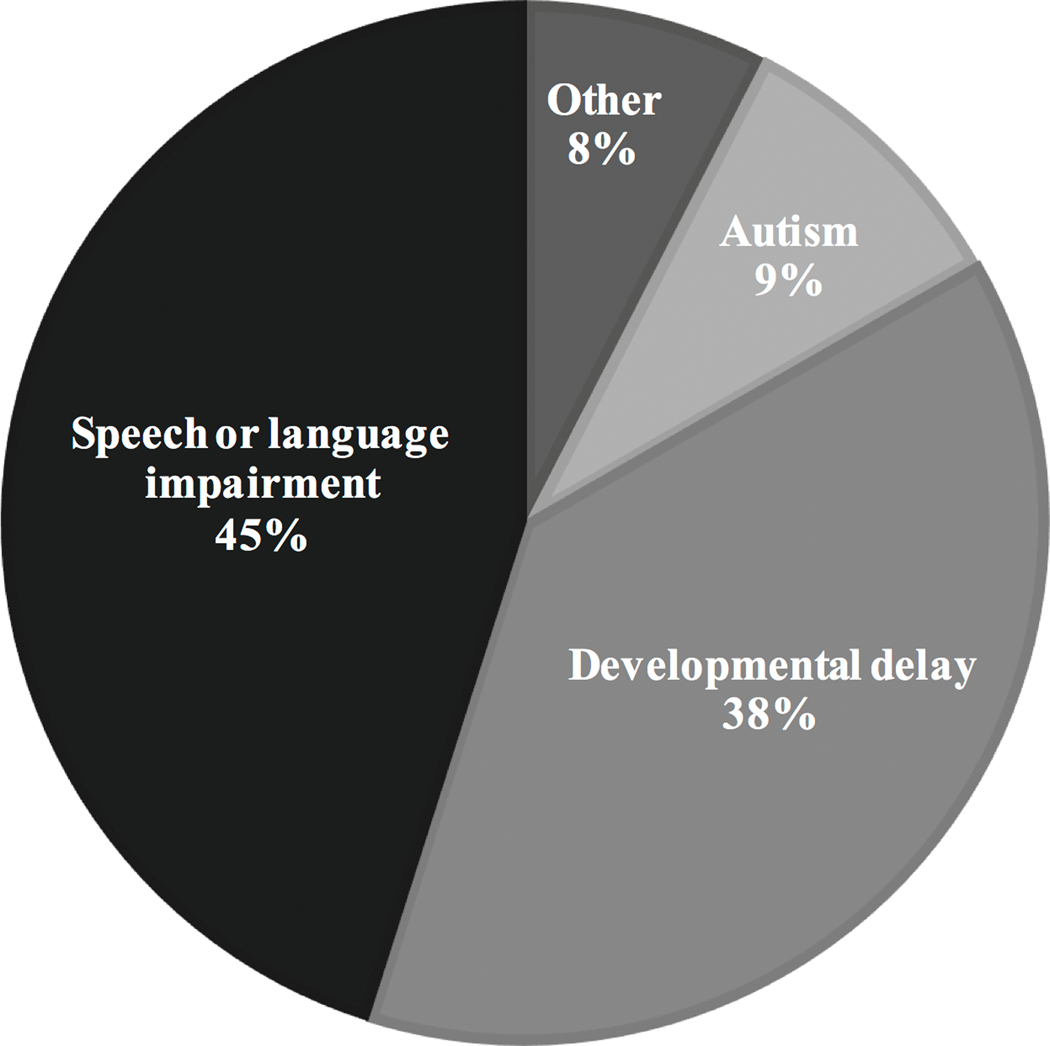
Variation in the rate and efficiency of language development is substantial. Approximately 16% of children experience delays in the initial phases of language learning and approximately half of those children show persistent difficulties (1). Among children ages 3 to 5 years, speech and language impairment is the most prevalent eligibility criteria that warrants enrollment in special education preschool services (Figure 1) (2). Among school aged children, the category of learning disabilities, often a late manifestation of language and speech disorders, predominates as the eligibility criterion for special education; however, speech-language impairment ranks second. Deficits in language or speech that are sufficiently severe to interfere with daily functioning, including learning, communication, and/or social interactions meet criteria as a disability.
Figure 1.
Percentages of the >750,000 children ages 3 to 5 years in special education services across the United States by eligibility criteria.
Pediatric clinicians are on the front line for primary, secondary, and tertiary prevention of language and speech disorders (3). Primary prevention, like immunizations, prevents the condition from occurring. Secondary prevention requires early detection and treatment of a disorder to result in a milder variant than would have occurred otherwise. Tertiary prevention may not change the disorder but improves functional outcomes of affected children. The over-riding objective of this review is to empower pediatric clinicians with prevailing theories, recent evidence, and recommendations to be used to promote primary, secondary, and tertiary prevention of language and speech disorders.
Definitions
Language is the distinctly human form of communication that binds human social groups. Language uses arbitrary but socially-agreed upon signals (words and sentences) in a rule-governed system to convey meaning. Unlike animal communication, human language uses signals creatively to communicate beyond the here-and-now, allowing discussion of past or future events and abstract, hypothetical, or imaginary ideas. Speech is the usual output of the language system, created by the complex and coordinated movements of respiratory, laryngeal, velopharyngeal, and oral structures. Other outputs include sign languages or written language. Language is subdivided into receptive (ability to understand) and expressive (ability to produce) language. Language is further thought to be comprised of interacting subsystems or components: phonology (the system of speech sounds), lexicon (vocabulary), syntax (grammar), semantics (meaning) and pragmatics (social aspects of language that take into account the speaker and the context). Speech is also comprised of subsystems: articulation (speech sounds), voice and resonance, and fluency.
Primary prevention
Language learning is a product of the interaction of the child’s learning capacities with the language environment (4). Insights about how young children learn language derive from computer simulation models based on “parallel distributed processing” or “connectionist frameworks,” that are designed to mimic characteristics of human brain structure and function (5). Basic processing units in these models are simple and highly interactive, analogous to neurons in the brain. Units that become active simultaneously develop connections and connections that occur in unison form networks. Knowledge is conceptualized as patterns of activity within the network; learning represents changes in the patterns of activity within and across networks. Networks do not require any initial biases or built-in organization but rather organize based on experiences in the environment. These models can explain how infants can learn whatever language they are exposed to. These computer models have been found to explain many of the phenomena of language learning, such as how children learn to correctly conjugate both regular verbs and irregular verbs (5).
A challenge for the infant is segmenting the sound stream into meaningful units, such as words, that serve as inputs for learning. Children use “statistical learning” for this purpose. Statistical properties of sound sequences vary. For example, sounds that occur within words have a higher frequency of co-occurrence than sounds that occur between words. Infants, as young as age 8-month, unconsciously detect these distributional statistical properties and use them to segment the continuous sound stream into word-like units (6). Sequential statistical learning allows the young child to detect sequential ordering and co-occurrence of words within sentences to explain the acquisition of syntax (7). Moreover, infants and children can take advantage of statistics of word-referent co-occurrences to learn the meaning of words (8). Statistical learning is facilitated when parents use child-directed language, colloquially known as baby talk. Child-directed language is characterized by limited vocabulary, short sentences, multiple repetitions, relatively few errors, and exaggerated intonation (9).
An important ingredient for language learning is the social context. Early language learning requires human interactions; televisions and computers are not sufficient. Warm, mutually respectful, low stress exchanges between infants and competent language users, adults or other children, facilitate learning. Language learning requires the child’s active engagement with the input. Children must monitor the input, detecting, for example, differences between what they heard and what they might have said or what they thought a word meant. Recognition of the discrepancy helps children progress in learning semantics and syntax. Talking about what a child is doing or expanding what a child has just said facilitates the child’s active engagement.
Another challenge for the infant is learning to map speech perception to speech production (10). Most of the structures that generate speech sounds in the vocal tract are hidden from view. “Mirror neurons” that fire both when an individual performs an action and when the individual perceives others performing the same action are plausible mechanisms for linking perception to production. Human mirror neuron populations appear to be clustered in several cortical areas in the brain, including the pre-frontal cortex, which are often implicated in language use (10).
Primary prevention of language and speech delays or disorders may be achieved by providing children with a rich language environment within positive social relationships. Therefore, recommendations that primary care clinicians can give to parents of infants and young toddlers are as follows:
Speak often to infants and young children. Baby talk, the use of simple sentences with exaggerated intonation, is well suited to children’s learning needs.
Use language to describe or explain what a young child is doing or to expand what a child has just said in order to engage the child for language learning.
Use of language during social interactions, such as reading books and playing. Reading is associated with more language input than meals, baths, or play (11).
Limit screen time (12) in favor of active interactions.
Support public policy initiatives that provide education to parents about language learning, such as nurse home visiting programs, or that support effective language environments for children, such as publicly funded universal preschool.
Early detection of language and speech delays
Early detection of language and speech delays is predicated on knowledge of the pattern of development. Table 1 documents milestones in the development of language and speech from infancy to age 8 years. Children produce their first words at about age 1 year. Initial lexical growth is slow, approximately 1–2 words/week. Once the vocabulary reaches about 50 words, the pace of development accelerates. Lexical growth increases to 1–2 new words/day and children begin combining words into two-word phrases. The “vocabulary spurt” has been attributed to biological factors, such as myelination of white matter language pathways (13). An increase in the pace of learning also conforms to self-organization of a neural network (5). Between ages 2 and 4 years, children build their lexicon and grammatical skills. Patterns of development vary across children, most likely as a function of their experiences in the environment. By school age, all of the fundamentals of language are typically mastered. Children may still show immaturities in motor speech skills to age 8 years, but intelligibility at school age should be about 100%.
Table 1:
Key Milestones in the development of receptive and expressive language, and speech
| Age | Receptive Skills | Expressive Skills | Speech |
|---|---|---|---|
| Newborn | • Attends to voice • Regards face |
• Cries | • |
| 3 months | • Smiles when spoken to | • Differentiates cry • Coos (makes vowel-like musical sounds) • Coos reciprocally with an adult |
• |
| 6 months | • Turns when name is called | • Begins to babbles (adds consonant sounds, such as b, d, m) | • |
| 9 months | • Stops when told “No” • Learns routines, such as “Wave bye-bye” |
• Points to wants or to interesting objects or actions • Says “mama” or “dada” non-specifically |
• |
| 12 months | • Follows simple commands with gestures | • Says “ma-ma” or “dada” specifically • Jargons (strings of babble that sound like speech) • Says first words |
• |
| 15–18 months | • Points to body parts • Follows single command without gesture |
• Acquires words slowly • Uses simple and idiosyncratic forms • Participates in conversations |
• |
| 18–24 months | • Understands sentences | • Exhibits vocabulary of ≥50 words • Learns new vocabulary items easily • Uses 2-word phrases |
• 50% correctly use p, m, h, n, w, b |
| 24–36 months | • Follows 2 and 3-step commands • Answers “wh-questions” |
• Uses >2 word phrases • Uses increasing complex grammar, such as negation, questions |
• 50% correctly use k, g, d, t, ng, f, y |
| 36–48 months | • Understands plurals, pronouns, and possessives • Understands questions of “who”, “why”, and “how many” |
• Combines 3–4 words in a sentence • Uses conjunctions, such as and or but |
• 90% correctly use p, m, h, n, w, b • 50% correctly use r, l, s, ch, sh, z • Able to produce final consonants in words, such as bus • No longer replaces sound made in the back of the mouth (g, k) with sounds made in the front of the mouth (d, t) |
| 48–60 months | • Understands concepts, such as same/different | • Uses mature grammar at near-adult levels • Constructs narrative discourse, such as tells or retells stories, makes explanations |
• 50% correctly use j, v, voicless th (thing) • 90% correctly use k, g, d, t, ng, f, y • Correct production of consonant clusters, such as st in stop • No longer deleting weak and unstressed syllables, such as in banana |
| 60–84 months | • Limited by the child’s conceptual knowledge, not language skills • Understands humor, metaphor |
• Mature language constructions • Increasing use of sophisticated vocabulary and complex grammar |
• 90% correctly use r, l, s, ch, sh, z, j, v, th • No longer substitutes liquids (r, l) with glides (w, j) • Can correctly use fricatives, such as voiceless th |
Developmental surveillance may detect children at high risk for disorders in language and speech. Surveillance uses all clinical approaches (history, physical and neurological exam, observations) at all health supervision visits. “Red flags” (Table 2) are delays or differences that indicate a high prevalence for persistent disorders and should prompt an evaluation:
Table 2.
Red flags indicting high risk of language or speech disorder and prompting evaluation
| By age | Red flag or indication for referral for evaluation |
|---|---|
| Any age | Failure to participate freely and frequently in social interactions |
| 6 months | Lack of ability to laugh, vocalize, respond to sound, participate in reciprocal vocal interactions |
| 9 months | Failure to respond differentially to name or produce babble (such as baba, dada) |
| 12 months | Inability to point to objects or actions Lack of use of gestures, such as shaking head “no” Inability to participate in verbal routines, such ability to wave to “wave bye-bye” No use of mama or dada specifically for a parent |
| 18 months | Less than 5 words beyond mama and dada Failure to follow simple commands with gestures |
| 24 months | Vocabulary less than 50 words No two-word combinations < 50% of utterances intelligible to unfamiliar adults |
| 36 months | Inability to follow simple directions without gestures No 3 or more word combinations < 75% of utterances intelligible to unfamiliar adults |
| ≤ 36 months | Loss of language and speech skills, particularly in the presence of regression in social abilities and in the absence of regression in motor skills |
The America Academy of Pediatrics (AAP) recommends developmental screening with a validated instrument at least at ages 9, 18, and 24 to 30 months of age (14, 15). Screening establishes whether a non- or pre-symptomatic child is at high or low risk for a language or speech disorder. A two-step screening process is important. The first step should use a general screening instrument, such as two commercial products, the Parents’ Evaluation of Developmental Status (http://www.pedstest.com/), the Ages and Stages Questionnaires, Third Edition (ASQ-3) (http://agesandstages.com/products-services/asq3/), or other tools that have been developed for use in low and middle income countries (16, 17). The second screen establishes the risk of autism spectrum disorder, using an instrument such as the Modified Checklist for Autism in Toddlers, Revised with Follow-Up (M-CHAT-R/F) (18). Autism screening alone may not be sufficient for establishing risk of language and speech disorders, which are more prevalent than autism (Figure 1). Autism screening may detect some children missed on global screens.
Screening is not necessary when the child is known to have delays, has another condition associated with language or speech disorder, such as hearing loss or preterm birth (see below), or is enrolled in therapy for language or speech. In such cases, further description of the child’s strengths and difficulties may be useful for monitoring the child’s progress. The following commercially available instruments could be used in such situations within the clinical setting:
MacArthur-Bates Communicative Development Inventory (https://mb-cdi.stanford.edu/), a parent report instrument for children age 8–37 months.
Language Development Survey, a parent report instrument for children age 18–35 months (http://www.aseba.org/research/language.html).
The Clinical Linguistic and Auditory Milestone Scale of The Capute Scales (http://www.brookespublishing.com/resource-center/screening-and-assessment/the-capute-scales/), a combination of direct assessment and parent report for children birth to 36 months.
Communication and Symbolic Behavior Scales Developmental Profile (CSBS DP) Infant Toddler Checklist (http://brookespublishing.com/wp-content/uploads/2012/06/csbs-dp-itc.pdf), an direct assessment of social communication for children age 6–24 months.
Variations in language and speech development that do not cause delay
Boys may show mild delays in the development of language and speech skills compared to girls (19). However, the differences are modest. Boys have higher rates of language and speech disorders than girls. Therefore, the probability that a boy with an early delay will develop a disorder is high.
Children raised in bilingual environments are capable of learning two languages at the same time (20), even children with disabilities, such as Down syndrome (21). Bilingual children may have smaller vocabularies in each of their languages than monolingual children, though their combined vocabulary should be comparable in size to that of monolingual children (22). They may initially show mixing of the two languages, though over time separation of the two languages occurs (22).
Another source of variation is the child’s birth order. Later-born children are likely to hear less adult-generated language directed toward them, but more likely to overhear conversations between adults and their older siblings and have the older siblings as role models (23). Overall, studies show that later-born children do not acquire language at a later age than do firstborns. Clinicians should use the same assessment and management approaches in the care of later-born children as they do with first-born children with comparable delays
Chronic otitis media with effusion does not cause developmental delays in language or speech. Randomized clinical trials comparing early tympanostomy tube placement to watchful waiting showed that the operation did not change the outcomes in preschool or school aged children (24, 25). Chronic otitis media is more prevalent in situations that also put language learning at risk, including poverty, crowding, limited breast feeding, and parental smoking (26), suggesting that it may be marker for adverse conditions that are associated with poor language or speech development. Clinicians should consider multiple reasons that children with chronic otitis media with effusion develop language or speech delays.
In summary, it is a misconception that children from the following categories with delays in early language or speech development will catch up to peers without any intervention:
Boys
Children from bilingual homes
Later born children
Children with chronic otitis media with effusion
In all these cases, the same thresholds should be used to define delays and disorders and the same clinical procedures should be followed.
Language and speech delays
The term” delays” implies that the development of language or speech skills is slower than expected for age and follows the usual developmental pattern. A delay becomes clinically relevant when the rate of development falls < 75% expected, such as when a skill expected at 18 months is not present in a 24-month child (18/24=3/4 or 75% the expected rate). Approximately half of children who are delayed in language at age 2 years catch up by age 3 years. Children who show good symbolic play skills and/or normal receptive language despite delayed expressive language have a better prognosis than those with delays in symbolic play and receptive language. Children with either language or speech delay should receive a comprehensive pediatric evaluation. Table 3 describes the components of a comprehensive pediatric evaluation. Based on the results of that assessment, the clinician may refer the child for treatment or place the child on an enhanced surveillance schedule. Factors that cause language or speech delays and should prompt treatment are as follows.
Table 3.
Evaluation of a child with language or speech delay or disorder
| Component of evaluation | Critical Information |
|---|---|
| History | Age at onset, initial presentation and subsequent course Affected subcomponents Effects of previous treatments |
| Past medical history | Birth history Previous illness and chronic conditions |
| Review of systems | Associated signs and symptoms |
| Family history | Family members with language, reading, or intellectual disorders Other health conditions |
| Psychosocial factors | Primary caregivers, parent education Number in the household, financial resources, stress Nature of parent-child interactions Amount and quality of child-directed speech Out of home care, including daycare, preschool, or school |
| Physical exam | Growth parameters Dysmorphic features Oral-motor structure and function |
| Neurological exam | Structural abnormalities, such as asymmetry in tone or reflexes Functional disorders, such as seizures |
| Audiological assessment | Ear specific information or sound field testing |
| Cognitive skills | Developmental assessment or an intelligence test |
| Symptoms of autism | Social communication and restrictive or repetitive behaviors |
Environmental factors.
A recent systematic review found that family environmental factors, such as socioeconomic status and parental education, parental health, and the level of engagement of parents with children are all associated with the rate of language development (27). Variation in the amount of language a child hears may mediate the effect of adverse social conditions on development. The classic observation that social class impacts language outcomes came from the work of Hart and Risley (28) who estimated the number of words children heard by recording weekly samples of conversations in their homes. Children of low socioeconomic status (SES) were exposed to 30 million fewer words than children of high SES. Recent studies using day-long recordings of home language have confirmed that amount of speech that children hear at age 16 or 18 months predicts lexical growth and speed of language processing at older ages (11, 29). In interpreting these environmental influences on child language, it is important to recognize the possibility of shared genetic variance between parent and child (30).
Infants raised in orphanages have profound delays in the development of language and speech along with many other health and developmental disorders (31). The Bucharest Early Intervention project demonstrated that these devastating effects could be eliminated though placement in foster care before 15 months of age. Adverse effects were moderated through placement in foster care before but not after 24 months of age (32). These encouraging data demonstrate the plasticity of language in its earliest stages.
Sex differences.
Boys have higher rates of language and speech delays and disorders than girls (33). This finding may be reflective of genetic variation, implicating sex chromosomes. Male sex is associated with pro-inflammatory forces and placental lesions (34). The maternal immune response against the invading interstitial trophoblast may be an initial event leading ultimately to sex differences in language disorders. Another possibility is that prenatal hormones, such as testosterone, exert important influences on the developing brain, influencing structural features such as the degree of laterality or difference between the left and right hemisphere (35).
Biological factors interact with environmental factors to explain sex differences in language and speech. Girls prefer to remain in close proximity and engage in social interactions with adults; boys prefer active, rough and tumble play. Sex differences interact with SES. Boy-girl sex differences have been found in low-SES but not high SES children (19). Clinicians are often slow to refer boys with language delays for treatment on the assumption that the child will eventually catch up. However, since boys are at higher risk than girls for disorders, clinicians should proceed to evaluation and treatment when a delay is detected.
Genetic factors.
Genetic variation appears to be important for variation in how quickly and efficiently children learn (36). Disorders of speech and language cluster in families; the median incidence of language difficulties was found to be over 3-times higher in families of children with language impairment than in unaffected families (37). Twin studies have confirmed that concordance of speech and language disorders is higher in monozygotic pairs than it is in dizygotic twins pairs. The presence of reading disorders in the family also put children at risk for language disorders (38).
The first reports identifying a specific genetic alteration associated with language and speech disorders came from studies of a large three-generation family, called the KE family, in which approximately half of the members had complex speech difficulties. A single nucleotide change on a gene called FOXP2, located on chromosome 7q31differentiated affected and unaffected family members. Curiously, this gene is one of a family of genes controlling transcription of other genes rather than coding traits. One theory is that FOXP2 influences the expression of other genes, such as CNTNAP2, that encodes a neurexin and is expressed in the developing human cortex. Genetic variation in CNTNAP2 has been associated with language impairment.
Beyond these findings, it has proven difficult to identify specific genes associated with language and speech disorders (39). It is possible that multiple genes may be involved (40) or that despite behavioral similarities, the disorders are heterogeneous, each with a distinctive genetic etiology. Decisions about genetic testing for children with speech and language disorder should be individualized, based on the phenotype, symptom severity, family history and related factors.
Primary disorders of language and speech
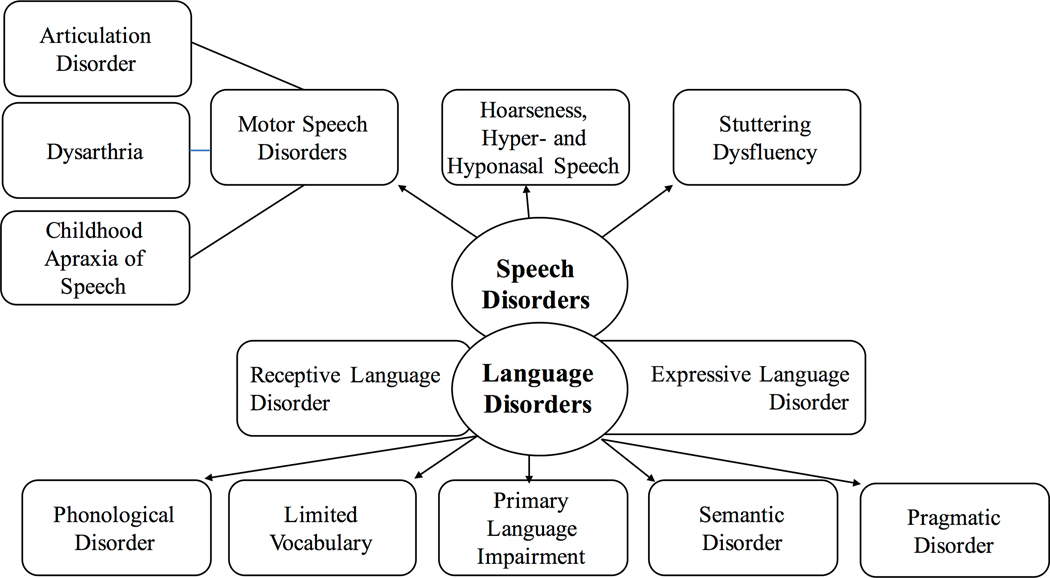
Secondary or tertiary prevention is predicated on early detection of language or speech disorders and prompt treatment, because early treatment is generally associated with better outcomes than delayed treatment. Language disorders represent deficiencies in the ability to express or understand human communication. Delays become disorders when they persist to school age, follow different developmental trajectories, are severe, and/or negatively impact functioning. One classification of language disorders subdivides them into receptive, expressive, and mixed expressive-receptive language disorders. However, this classification system may not be accurate. Difficulties with language expression may be accompanied by limitations in language comprehension and processing that are subtle and more difficult to detect than the problems of expression [REF]. An alternative classification of disorders of language is based on the aspects of language affected (Figure 2), aligned with subcomponents of phonology (the system of speech sounds), lexicon (vocabulary), syntax (grammar), semantics (meaning) and pragmatics (social aspects of language that take into account the speaker and the context). Speech disorders can also affect one or more subcomponents (Figure 2), representing difficulties with speech sounds, vocal quality and resonance, and/or fluidity.
Figure 2.
Components of language and speech
A persistent and serious delay in the acquisition of language skills in the absence of other developmental, health, or mental health conditions goes by many names: spoken language disorder, primary, or specific language impairment (SLI)(41). SLI indicates that though the language disorder is the most relevant finding, associated conditions, may also be present. SLI is clinically heterogeneous. Usually, difficulties with syntax are prominent (Figure 3). Other features may include delays in phonologic development, semantics, and/or pragmatics. Children with SLI typically present with delayed emergence of single words, phrases, and sentences. Comprehension often appears relatively spared. Speech skills also may or may not be impaired.
Several general neuropsychological processes, such as speed of language processing and memory, are associated with SLI. Speed of language processing at age 18 months, as measured in an eye tracking task, has been found to be associated with measures of language skills up to age 8 years (42). Children who are late talkers at age 2 years and at high risk for SLI have slower speed of processing than children with typical early language. Slow speed of processing may result in SLI because affected children have difficulty understanding, anticipating, and learning from rapid-paced speech or sentences of increasing length. Deficits in phonological short-term and working memory are also associated with SLI (43), presumably because it is essential to hold sound patterns in mind in order to learn new words and structures. Phonological short-term memory can be measured by a non-word repetition task that requires children to listen to novel phonetic sequences of varying lengths and repeat them back. At older ages, children with SLI may meet criteria for Attention Deficit Hyperactivity Disorder and/or may have difficulties with executive functions, such as response inhibition, working memory, organization or planning. Children with SLI are at risk for later reading disorders because reading rests on a foundation of language abilities (44).
Disorders of speech may occur in isolation or in conjunction with disorders of language. Articulation disorders are motor speech disorders that represents difficulties producing specific sounds of the language (Figure 3). Mild articulation disorders are highly prevalent and rarely disrupt communication or social functions. Severe articulation disorders may impact other domains of function. Dysarthria is a disorder of the muscle movements required for speech production and often occurs in the aftermath of brain injury. Childhood Apraxia of Speech is considered a disorder of planning and executing speech sounds. Hallmarks of the condition include delays in the onset of babbling or single word productions, errors in articulating vowel sounds, inconsistent errors in producing words, increasing difficulty with words or phrases of increasing length, increased difficulty with production of spontaneous as opposed to well-rehearsed sentences, and effortful speech. The importance of differentiating Childhood Apraxia of Speech from other disorders is that the treatment approach is distinctive; children typically require an approach that emphasizes motor programming and motor learning to improve production of speech sounds. They also need intensive and frequent practice of staged and specific speech targets.
Stuttering is a disorder of fluency (Figure 3). Children often experience dysfluency before age 4 years as their thinking processes outpace their speech processes. Developmental dysfluency involves repetition of entire words or phrases. Stuttering is a non-developmental problem that includes repetition of individual speech sounds (p-p-p-pop); prolongations (mmmme); abnormal pauses between sounds; excessive use of fillers, such as uh or um; and use of behavioral strategies, such as self-slapping to try to get the words out. Even at ages < 4, the presence of the features of stuttering should prompt referral for further evaluation and treatment.
Speech-Language Disorders secondary to known conditions.
Secondary and tertiary prevention require early detection and treatment of language and speech disorders among children with other health or neurodevelopmental conditions. The use of parent-reported questionnaires or direct observation language and speech instruments within pediatric subspecialty care is recommended for children, especially for those who are not receiving speech-language pathology services, early intervention or special education (see above). Recommendations for the evaluation of children with language and speech delays or disorders are designed to rule out known causes, including adverse psychosocial conditions (Table 2).
Hearing loss. Language and speech disorders are highly likely with severe to profound hearing loss (threshold > 55 decibels). Individuals with mild (threshold of 26–40 decibels) to moderate (threshold of 41 to 55 decibels) sensorineural hearing loss may be able to detect and discriminate vowel sounds and low-frequency consonants, such as /m/ and /b/, but may not detect or discriminate high-frequency consonants, such as /f /, /th/ and /sh/. Universal newborn hearing screening has increased early identification of children with moderate to profound hearing loss. Reevaluation of hearing in children with language or speech abnormalities is critical because the newborn test may have been a false negative, the hearing loss may be mild, or the child may have a progressive hearing loss.
Global developmental delay and intellectual disability. Language and speech delay may be the initial presentation of children with global developmental delays. If delays persist and are accompanied by deficits in adaptive skills, children may meet criteria for intellectual disability. Intellectual disability ranges from mild (IQ 55–69) to profound levels (IQ < 25). Language skills are generally commensurate with other developmental abilities. Even children with severe intellectual disability (IQ 25–39) typically learn at least minimal language skills.
Autism. Autism is defined by two key criteria: deficits in the domain of social communication and excessive restricted or repetitive behaviors. The presenting problem in autism is often delays or regression in speech and language skills. The prevalence of autism had been increasing over the last two decades and has stabilized over the last 8 years (45). Prognosis is better when children receive early intervention services than when behavior management and education are delayed. For these reasons, consideration of the diagnosis of autism is critically important in the evaluation of children with language delay.
Known genetic variations. Chromosomal and genetics conditions have distinctive profiles in terms of speech and language. For example, in trisomy 21 or Down syndrome, deficits in speech and language skills are often more severe than deficits in non-verbal skills. In Williams Syndrome (WS), caused by a deletion on chromosome 7, deficits in non-verbal skills are more severe than deficits in language. Fragile X is caused by a trinucleotide repeats and mutations in the FMR1 gene. Individuals with Fragile X have deficient language skills in association with poor social skills, high levels of anxiety, and frequent hyperactivity. About 20–25% of individuals with Fragile X meet criteria for a diagnosis of autism.
Neurological disorders. Structural brain injuries may affect language and speech. Children with injury to left or right hemisphere frontal and temporal regions may show delays in the early phases of language development and subsequent disorders, though their symptoms are milder than those of adults with similar injuries (46, 47). Notably, environmental factors influence the rate of language learning after brain injury. By age 5, children from high SES families with brain injury outperformed children without brain injury from low SES families (48). Functional magnetic resonance imaging studies have found that children with early left hemisphere injury show multiple pathways of plasticity, associated with variation in outcome (49) Specific epilepsy syndromes are associated with language and speech disorders. Landau Kleffner is a rare seizure disorder associated with regression in speech and language skills and therefore part of the differential diagnosis in autism with regression. However, whereas the regression in autism typically occurs before age 3, the regression in Landau Kleffner occurs later. The cardinal finding is auditory agnosia, a profound disruption of language comprehension with resulting adverse effects on language production. Other neurological conditions with effects on language and speech include tuberous sclerosis.
Cleft palate. Cleft palate is failure of fusion of the hard and/or soft palate. Even if the defect is repaired, weak velopharyngeal muscles allow air to flow through the nose rather than out the mouth in the production of speech sounds, resulting in hypernasal speech. Children with cleft palate, even as an isolated condition and not part of a broader syndrome, may also experience delays or disorders in the development of language as well as speech though the reasons are not clear.
Other health conditions. Meta-analyses show that children born preterm show persistent delays in the development of language (50), independent of socioeconomic status, and even among samples that include only children without major disabilities, such as cerebral palsy, intellectual disabilities, and sensory impairments (51). These deficits have been attributed to subtle neurological deficits that may be present even in the absence of telltale signs on neuroimaging. Similarly, children with congenital heart disease show delays in the development of language, associated with changes in white matter (52).
Management and Treatment
Children with language or speech delays or disorders have failed to learn language from observation and social participation. Therefore, watchful waiting is rarely a good approach. Therapy is warranted. The speech-language pathologist is the professional charged with designing and implementing the treatment plan for a child with language or speech delays or disorders. Speech-language pathology services alone may be adequate for the child with mild to moderate language or speech delays or isolated disorders without complications. Early intervention for children birth to 3 or special education services for children over age 3 is appropriate for children with moderate to severe language and speech disorders, other developmental conditions, and/or behavioral challenges that compromise participation and cooperation. Referral to therapy services is appropriate even while the comprehensive evaluation of the disorder is ongoing because of the long delays for many diagnostic services.
Though the causes of language and speech disorders are diverse, including genetic or neurological conditions, manipulation of the child’s experience in the environment is the main lever available to improve the child’s skills and functioning. The speech-language pathologist, implicitly or explicitly, creates environments that increases the odds of the child’s learning the weak or missing skill. Effective language interventions may provide a higher number of effective language learning episodes than would be available to children in their typical environment. Therapy may increase the child’s opportunities to listen and speak, increase the salience of elements that the child has not mastered, and/or encourage expression of weak and developing skills. Therapy may also provide corrective feedback, such as recasting, that facilitates learning correct forms. Critical ingredients for therapeutic intervention, analogous to primary learning, are the child’s active engagement and a warm supportive relationship. Therapy for toddlers and preschoolers is typically play-based rather than drill. The specific activities chosen for a session focus on interests of the child. An example of home-based speech-language therapy can be found at the following url: https://www.youtube.com/watch?v=9gTPS0cX4VQ.
The data on the efficacy or effectiveness of speech and/or language therapy, especially using randomized controlled trials is limited. However, a systematic review and meta-analysis found that speech and language therapy is generally effective for children with phonological or expressive vocabulary difficulties but less clear for children with expressive syntax difficulties. Little evidence was available considering the effectiveness of intervention for children with receptive language difficulties (53).
Children often get a minimal dose of speech-language therapy, such as 30 to 60 minutes of therapy a week or less. The low dose of treatment is driven in part by child factors, such as children’s relatively weak attentional capacity and by systems issues, such as high costs and limited availability of therapists. Participation of parents, family members and teachers in the program leverages the otherwise limited intensity of service. A systematic review found no significant differences between interventions administered by trained parents and clinicians (53). A second systematic review reported that home programs can lead to growth in a child’s skills and are more effective than no intervention, provided that a high dose of program is delivered by parents who have received direct training in the intervention techniques (54). Another strategy to increase the dose of treatment is to provide group therapy sessions; the duration of treatment is not the 30 to 60 minutes reserved for a single child, but 2 to 3 hours for 4 to 8 children. The added advantage of group therapy is that children practice their developing skills with other children in semi-naturalistic settings. A systematic review found no differences in the effects of individual versus group therapies (41). Language and speech therapy are often part of a child’s individual educational plan at school. Teachers as well as parents should know the goals and strategies that the speech-language pathologists are using and apply them in the classroom to maximize the impact of therapeutic services.
As children age, it becomes increasingly important that they can use language and speech skills in the service of functional domains, including learning, communication, and social interaction. A systematic review of school-based treatment procedures addressing social communication behaviors found that gains were seen in conversational abilities, including topic management skills, narrative production, and repairs of inadequate or ambiguous comments (55).
For children with poor motivation or disordered behavior, behavioral measures may be included with rewards and consequences for desired and undesired behaviors, respectively. Behavioral approaches are typically required for children with autism who lack motivation to communicate. Developmental and naturalistic behavioral techniques are particularly appropriate for young children because they can be applied in everyday activities. For children with motor speech disorders, especially Childhood Apraxia of Speech, a motor learning component is included in the therapy; the child practices carefully planned sequences of emerging sound patterns. Examples of therapies for Childhood Apraxia of Speech can be found at the following website: https://www.youtube.com/watch?v=sq7vFWLqodM. Recommendations for therapy for Childhood Apraxia of Speech include frequent but short sessions, at least four times per week, with family and school participation in the treatment program; preliminary evidence demonstrates promising outcomes (56). Use of non-speech oral motor exercises, such as blowing, lip strengthening, and lateral tongue movements are not beneficial for the treatment of motor speech disorders primarily because speech sounds do not use the oral mechanisms in the same movements as eating or drinking. However, cues to placement of the tongue or lips for proper speech sound production may be helpful. For children with extremely limited verbal output, assistive and augmentative communication devices (AACs), such as sign language, picture exchange, or voice activated software, may also be considered. AAC methods are often taught in schools. Unfortunately, high technology devices may not be able to travel home with the student. In addition, family members may not learn the AAC methods and therefore cannot help their child to use the technique in home and community settings. To be most effective, AAC parents and teachers should get training in the use of the AAC method and should encourage the child to use the method in all communication settings.
Summary
Language is a distinctly human form of symbolic communication. Delays and disorders of language and speech are prevalent (1). The main points of this review and the clinical implications are as follows:
Research shows that the amount of child-directed speech is a strong contributor to the child’s language development (11, 27, 28). Based on clinical consensus in relation to these data, primary care clinicians play a role in primary prevention of language and speech disorders by counseling families about the importance of the learning environment. The US Preventive Services Task Force concluded that no studies have yet examined the effects of screening on speech and language or other functional outcomes (57). However, based on some research and consensus, professional organizations recommend a developmental screening at age 9, 18 and 24 or 30 months and, in addition, autism screening at 18 and 24 or 30 months (14,15).
Research shows that bilingualism (19), later birth order (22), and otitis media (23–25) are not causes of language delays. Therefore, children with delays and these conditions should be managed in the same manner as all other children with delays.
The specific diagnoses of language and speech disorders are predicated on the component of language or speech affected. Additionally, disorders may be classified as primary when no other major disorder is present (41). Disorders may be secondary to other conditions, including severe psychosocial deprivation, hearing loss, global developmental delay or intellectual disability, known genetic variants, and neurological conditions, and other health conditions, such as prematurity.
Speech-language therapy has been shown to be useful for some though not all disorders of language and speech disorders (53, 57). Nonetheless, based on this research, clinical consensus is that children should be referred for language and/or speech therapy, either in isolation or as part of an early intervention or special education program.
On-going monitoring by the primary care clinician may allow early detection of attention deficits, executive function limitations, or reading disorders, all of which may be associated with language or speech disorders. The ultimate goal of all screening, assessment, referral and on-going monitoring is to allow children to reach their maximal functional capacity for language and speech and to participate fully and joyfully within the human community.
Figure 3.
Disorders of language and speech based on affected component
ABP Content Specifications :
Content Specifications for General Pediatrics
Domain 1: A. Normal Growth and Development, 4. Language Development
Domain 1: D. Screening and Disease Prevention, 3. Psychosocial Screenings
Domain 5: A. Cognition, language, learning, and neurodevelopment 1. Clinical presentation (eg, development delay - cognition, language, learning or social)
Domain 5: A. Cognition, language, learning, and neurodevelopment. 2. Disorders and conditions, c. Autism
Practice Gaps:
To prevent delays and disorders and to provide effective clinical care to children with disorders of language and speech occur, pediatric clinicians must become familiar with prevailing theories, evidence, and recommendations of professional organizations. Pediatricians should not postpone evaluation and treatment for boys, children from bilingual environments, second- or third-born children, or children with chronic otitis media with effusion.
Acknowledgments
Funding source: Ballinger-Swindells Endowed Professorship for Developmental and Behavioral Pediatrics at Stanford University School of Medicine
Abbreviations
- AAC
Assistive and augmentative communication
- SLI
Specific Language Impairment
- SES
Socioeconomic Status
Footnotes
Conflict of Interest and Financial Disclosure statements: None
Learning objectives: By completion of this article, readers should be able to
1. Apply current theories regarding how young children learn language and speech to accomplish primary prevention of language and speech disorders
2. List key milestones of typical language development and indicators of high risk status for language or speech disorders to assist in early detection of disorders
3. Justify the use of both general and autism-specific screening tools for screening language and speech disorders
4. Discuss primary and secondary causes of language and speech disorders to develop strategies for secondary prevention
5. Evaluate intensity and nature of speech-language pathology therapy to treat children with language disorders as part of secondary and tertiary prevention
REFERENCES
- 1.Speech and language disorders in children: Implications for the Social Security Administration’s Supplemental Security Income program. Washington, DC: National Academies Press; US; 2016. [PubMed] [Google Scholar]
- 2.Number of Children Receiving Early Intervention and Special Education Services under IDEA, Birth through Age 5 2016. [Available from: http://www.ksits.org/download/KS-acc-statedatadisplay-Part-C.pdf.
- 3.Simeonsson RJ. Primary, secondary, and tertiary prevention in early intervention. J Early Interv. 1991;15(2):124–34. [Google Scholar]
- 4.Poll GH. Increasing the odds: applying emergentist theory in language intervention. Lang Speech Hear Serv Sch. 2011;42(4):580–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joanisse MF, McClelland JL. Connectionist perspectives on language learning, representation and processing. Wiley Interdiscipl Rev Cog Sci. 2015;6(3):235–47. [DOI] [PubMed] [Google Scholar]
- 6.Saffran JR. Words in a sea of sounds: the output of infant statistical learning. Cognition. 2001;81(2):149–69. [DOI] [PubMed] [Google Scholar]
- 7.Kidd E Implicit statistical learning is directly associated with the acquisition of syntax. Dev Psychol. 2012;48(1):171–84. [DOI] [PubMed] [Google Scholar]
- 8.Smith LB, Suanda SH, Yu C. The unrealized promise of infant statistical word-referent learning. Trends Cogn Sci. 2014;18(5):251–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thiessen ED, Girard S, Erickson LC. Statistical learning and the critical period: how a continuous learning mechanism can give rise to discontinuous learning. Wiley Interdiscipl Rev Cog Sci. 2016;7(4):276–88. [DOI] [PubMed] [Google Scholar]
- 10.Casserly ED, Pisoni DB. Speech perception and production. Wiley Interdiscipl Rev Cog Sci. 2010;1(5):629–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weisleder A, Fernald A. Talking to children matters: early language experience strengthens processing and builds vocabulary. Psychol Sci. 2013;24(11):2143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Council On Communications Media. Media and Young Minds. Pediatr. 2016;138(5):11. [Google Scholar]
- 13.Pujol J, Soriano-Mas C, Ortiz H, Sebastian-Galles N, Losilla J, Deus J. Myelination of language-related areas in the developing brain. Neurology. 2006;66(3):339–43. [DOI] [PubMed] [Google Scholar]
- 14.Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatr. 2006;118(1):405–20. [DOI] [PubMed] [Google Scholar]
- 15.Workgroup Bright Futures Periodicity Schedule, Committee on Practice, Ambulatory Medicine. 2014 recommendations for pediatric preventive health care. Pediatri. 2014;133(3):568–70. [Google Scholar]
- 16.Ertem IO, Dogan DG, Gok CG, Kizilates SU, Caliskan A, Atay G, et al. A guide for monitoring child development in low-and middle-income countries. Pediatr. 2008;121(3):e581–e9. [DOI] [PubMed] [Google Scholar]
- 17.Khan N, Muslima H, Shilpi A, Begum D, Akhtar S, Parveen M, et al. Validation of a home-based neurodevelopmental screening tool for under 2-year-old children in Bangladesh. Child Care Health Dev. 2013;39(5):643–50. [DOI] [PubMed] [Google Scholar]
- 18.Robins DL, Casagrande K, Barton M, Chen C-MA, Dumont-Mathieu T, Fein D. Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatr. 2014;133(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barbu S, Nardy A, Chevrot J-P, Guellaï B, Glas L, Juhel J, et al. Sex Differences in Language Across Early Childhood: Family Socioeconomic Status does not Impact Boys and Girls Equally. Front Psychol. 2015;6:1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoff E, Core C. Input and language development in bilingually developing children. Semin Speech Lang. 2013;34(4):215–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bird EK-R, Cleave P, Trudeau N, Thordardottir E, Sutton A, Thorpe A. The language abilities of bilingual children with Down syndrome. Am J Speech Lang Pathol. 2005;14(3):187–99. [DOI] [PubMed] [Google Scholar]
- 22.Hoff E, Core C. What Clinicians Need to Know about Bilingual Development. Semin Speech Lang. 2015;36(2):89–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oshima-Takane Y, Goodz E, Deverensky JL. Birth order effects on early language development: Do secondborn children learn from overheard speech? Child Dev. 1996;67(2):621–34. [Google Scholar]
- 24.Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Rockette HE, Pitcairn DL, et al. Tympanostomy tubes and developmental outcomes at 9 to 11 years of age. N Engl J Med. 2007;356(3):248–61. [DOI] [PubMed] [Google Scholar]
- 25.Paradise JL, Feldman HM, Campbell TF, Dollaghan CA, Colborn DK, Bernard BS, et al. Effect of early or delayed insertion of tympanostomy tubes for persistent otitis media on developmental outcomes at the age of three years. N Engl J Med. 2001;344(16):1179–87. [DOI] [PubMed] [Google Scholar]
- 26.Paradise JL, Rockette HE, Colborn DK, Bernard BS, Smith CG, Kurs-Lasky M, et al. Otitis media in 2253 Pittsburgh-area infants: prevalence and risk factors during the first two years of life. Pediatr. 1997;99(3):318–33. [DOI] [PubMed] [Google Scholar]
- 27.Carvalho Ade J, Lemos SM, Goulart LM. Language development and its relation to social behavior and family and school environments: a systematic review. CoDAS,. 2016;28(4):470–9. [DOI] [PubMed] [Google Scholar]
- 28.Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore MD: Brooks Publishing CO; 1995. [Google Scholar]
- 29.Adams K, Marchman V, Loi E, Ashland M, Fernald A, Feldman H. Caregiver Talk and Medical Risk as Predictors of Language Outcomes in Full Term and Preterm Toddlers. Child development. 2017;published on line. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dale PS, Tosto MG, Hayiou-Thomas ME, Plomin R. Why does parental language input style predict child language development? A twin study of gene-environment correlation. J Commun Disord. 2015;57:106–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Windsor J, Glaze LE, Koga SF. Language acquisition with limited input: Romanian institution and foster care. J Speech Lang Hear Res. 2007;50(5):1365–81. [DOI] [PubMed] [Google Scholar]
- 32.Windsor J, Benigno JP, Wing CA, Carroll PJ, Koga SF, Nelson CA, et al. Effect of foster care on young children’s language learning. Child dev. 2011;82(4):1040–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallace IF, Berkman ND, Watson LR, Coyne-Beasley T, Wood CT, Cullen K, et al. Screening for speech and language delay in children 5 years old and younger: A systematic review. Pediatr. 2015;136(2):e449–e62. [DOI] [PubMed] [Google Scholar]
- 34.Challis J, Newnham J, Petraglia F, Yeganegi M, Bocking A. Fetal sex and preterm birth. Placenta. 2013;34(2):95–9. [DOI] [PubMed] [Google Scholar]
- 35.Geschwind N, Galaburda AM. Cerebral lateralization: Biological mechanisms, associations, and pathology: I. A hypothesis and a program for research. Arch Neurol. 1985;42:428–59. [DOI] [PubMed] [Google Scholar]
- 36.Plomin R Genetic factors contributing to learning and language delays and disabilities. Child Adolesc Psychiatr Clin N Am. 2001;10(2):259–77, viii. [PubMed] [Google Scholar]
- 37.Grigorenko EL. Speaking genes or genes for speaking? Deciphering the genetics of speech and language. Child Psychol Psychiatry. 2009;50(1–2):116–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Snowling MJ, Melby-Lervag M. Oral language deficits in familial dyslexia: A meta-analysis and review. Psychol Bull. 2016;142(5):498–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Plomin R Child development and molecular genetics: 14 years later. Child Dev. 2013;84(1):104–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Benyamin B, St Pourcain B, Davis O, Davies G, Hansell N, Brion M, et al. Childhood intelligence is heritable, highly polygenic and associated with FNBP1L. Mol Psychiatry. 2014;19(2):253–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leonard LB. Is expressive language disorder an accurate diagnostic category? Am J Speech Lang Pathol. 2009;18(2):115–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Law J, Garrett Z, Nye C. Speech and language therapy interventions for children with primary speech and language delay or disorder. Cochrane Database Syst Rev. 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marchman VA, Fernald A. Speed of word recognition and vocabulary knowledge in infancy predict cognitive and language outcomes in later childhood. Dev Sci. 2008;11(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Archibald LM, Gathercole SE. Short-term and working memory in specific language impairment. Int J Lang Commun Disord. 2006;41(6):675–93. [DOI] [PubMed] [Google Scholar]
- 45.Hulme C, Snowling MJ. Reading disorders and dyslexia. Curr Opin Pediatr. 2016;28(6):731–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. Autism Spectrum Disorder (ASD): Data and Statistics 2017. [updated March 10, 2017 Available from: https://www.cdc.gov/ncbddd/autism/data.html.
- 47.Newport EL. 45 The Importance of Developmental Plasticity. Scientists Making a Difference: One Hundred Eminent Behavioral and Brain Scientists Talk about Their Most Important Contributions. 2016:210. [Google Scholar]
- 48.Feldman HM, Holland AL, Kemp SS, Janosky JE. Language development after unilateral brain injury. Brain Lang. 1992;42(1):89–102. [DOI] [PubMed] [Google Scholar]
- 49.Rowe ML, Levine SC, Fisher JA, Goldin-Meadow S. Does linguistic input play the same role in language learning for children with and without early brain injury? Dev Psychol. 2009;45(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liégeois F, Connelly A, Cross JH, Boyd SG, Gadian DG, Vargha-Khadem F, et al. Language reorganization in children with early-onset lesions of the left hemisphere: an fMRI study. Brain. 2004;127(6):1229–36. [DOI] [PubMed] [Google Scholar]
- 51.Barre N, Morgan A, Doyle LW, Anderson PJ. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr. 2011;158(5):766–74.e1. [DOI] [PubMed] [Google Scholar]
- 52.van Noort-van der Spek IL, Franken M-CJP, Weisglas-Kuperus N. Language Functions in Preterm-Born Children: A Systematic review and meta-analysis. Pediatr. 2012;129(4):745–54. [DOI] [PubMed] [Google Scholar]
- 53.Rollins CK, Asaro LA, Akhondi-Asl A, Kussman BD, Rivkin MJ, Bellinger DC, et al. White Matter Volume Predicts Language Development in Congenital Heart Disease. J Pediatr 2017;181:42–8. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Law J The implications of different approaches to evaluating intervention: evidence from the study of language delay/disorder. Folia Phoniatr Logop. 2004;56(4):199–219. [DOI] [PubMed] [Google Scholar]
- 55.Tosh R, Arnott W, Scarinci N. Parent-implemented home therapy programmes for speech and language: A systematic review. Int J Speech Lang Pathol. 2017;52(3):253–69. [DOI] [PubMed] [Google Scholar]
- 56.Gerber S, Brice A, Capone N, Fujiki M, Timler G. Language use in social interactions of school-age children with language impairments: an evidence-based systematic review of treatment. Lang Speech Hear Serv Sch. 2012;43(2):235–49. [DOI] [PubMed] [Google Scholar]
- 57.Murray E, McCabe P, Ballard KJ. A systematic review of treatment outcomes for children with childhood apraxia of speech. Am J Speech Lang Pathol. 2014;23(3):486–504. [DOI] [PubMed] [Google Scholar]
- 58.Berkman ND, Wallace I, Watson L, Coyne-Beasley T, Cullen K, Wood C, & Lohr KN Screening for Speech and Language Delays and Disorders in Children Age 5 Years or Younger: A Systematic Review for the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015. Report No.: 13–05197-EF-1 [PubMed] [Google Scholar]