To the Editor:
Infection with severe acute respiratory syndrome caused by the novel coronavirus 2019 (SARS-CoV-2) and resulting coronavirus disease 2019 (COVID-19) is a global pandemic.1 Pediatric cases have some peculiarities, such as milder clinical manifestations and different laboratory abnormalities.2 A systematic review on laboratory data identified 12 articles, with a total of 66 pediatric patients.3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 Lymphopenia was found in only 3% of children, whereas lymphopenia often is described in adult patients.16 , 17 Neutropenia was recorded in 6% of cases, but it was never less than 0.500 × 109/L in this population.3
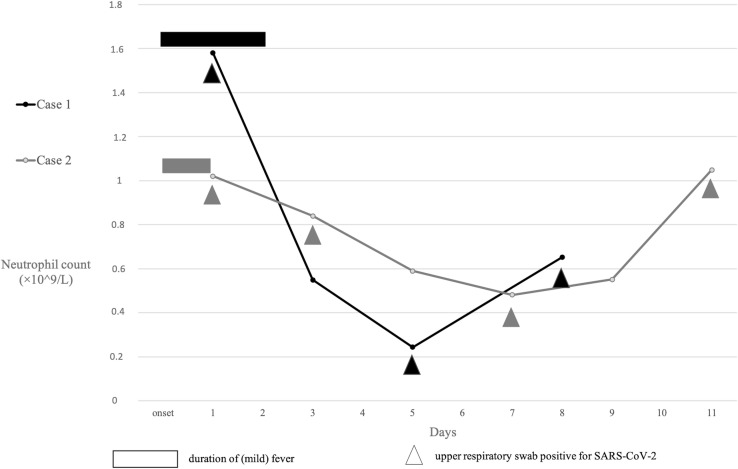
We describe a 23-day-old and a 39-day-old infant with mild COVID-19 and severe neutropenia who were cared for at our tertiary care referral pediatric hospital. They both came to medical attention with low-grade fever and mild respiratory symptoms with a history of contact with an infected person or persons. At admission, leukocyte and neutrophil counts were normal, nasopharyngeal swab tested positive for COVID-19, and co-infection with influenza-like viruses was excluded. On the fifth day and days after the beginning of symptoms, the 39-day-old girl and the 23-day-old girl developed severe neutropenia, with a nadir of 0.244 × 109/L neutrophils and 0.482 × 109/L neutrophils, respectively (Figure ). No other alterations on routine examinations were recorded and the neutrophil values improved without clinical complications.
Figure.
Absolute neutrophil counts in two infants with SARS-CoV-2 infection.
The presence of isolated severe neutropenia has not been described in children with COVID-19. This finding is noteworthy, because postinfectious transient neutropenia has been associated with many other viral infections in infancy, which might share pathogenic mechanisms.18 , 19 Moreover, the evidence of neutropenia in neonates and infants could be another manifestation of the age-related different immunologic response to SARS-CoV-2 infection.
Complete blood counts might be indicated 5-7 days after illness onset to detect neutropenia. We hope to alert providers to evaluate children, especially the youngest, with evidence of new symptoms during the second week after onset of illness to exclude severe neutropenia and possible secondary infection.
References
- 1.World Health Organization Novel coronavirus (COVID-19) situation. https://who.sprinklr.com
- 2.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 [Epub ahead of print] [Google Scholar]
- 3.Henry B.M., Lippi G., Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med. 2020 doi: 10.1515/cclm-2020-0272. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan J.F., Yuan S., Kok K.-H., To K.K., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai J., Xu J., Lin D., Yang Z., Xu L., Qu Z. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa198. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai J.H., Wang X.S., Ge Y.L., Xia A.M., Chang H.L., Tian H. [First case of 2019 novel coronavirus infection in children in Shanghai] Zhonghua Er Ke Za Zhi. 2020;58:86–87. doi: 10.3760/cma.j.issn.0578-1310.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Chen F., Liu Z., Zhang F., Xiong R.H., Chen Y., Cheng X.F. [First case of severe childhood novel coronavirus pneumonia in China] Chin J Pediatr. 2020;58:179–182. doi: 10.3760/cma.j.issn.0578-1310.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Feng K., Yun Y.X., Wang X.F., Yang G.D., Zheng Y.J., Lin C.M. Analysis of CT features of 15 children with 2019 novel coronavirus infectionZhonghua Er Ke Za Zhi. 2020;58:007. doi: 10.3760/cma.j.issn.0578-1310.2020.0007. [DOI] [PubMed] [Google Scholar]
- 10.Kam K., Yung C.F., Cui L., Lin Tzer Pin R., Mak T.M., Maiwald M. A well infant with coronavirus disease 2019 (COVID-19) with high viral load. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa201. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang D., Ju X.L., Xie F., Lu Y., Li F.Y., Huang H.H. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern ChinaZhonghua Er Ke Za Zhi. 2020;58:011. doi: 10.3760/cma.j.cn112140-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y.H., Lin D.J., Xiao M.F., Wang J.C., Wei Y., Lei Z.X. 2019 Novel coronavirus infection in a three-month-old babyZhonghua Er Ke Za Zhi. 2020;58:182–184. doi: 10.3760/cma.j.issn.0578-1310.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Zeng L., Tao X., Yuan W., Wang J., Liu X., Liu Z. China's first neonatal coronavirus pneumoniaChin J Pediatr. 2020;58 [Google Scholar]
- 14.Zhang G., Zjang A., Huang L., Cheng L.Y., Liu Z.X., Peng X.L. Twin girls infected with SARS-CoV-2Chin J Contemp Pediatr. 2020;22:221–225. doi: 10.7499/j.issn.1008-8830.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao R., Shen X., Yu K., Sheng . [A case of children with 2019 novel Coronavirus Infection]. Zhejiang Med J; 2020. [Epub ahead of print] [Google Scholar]
- 16.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J. Chinese Pediatric Novel Coronavirus Study Team. SARS-CoV-2 infection in children. N Engl J Med. 2020 doi: 10.1056/NEJMc2005073. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Husain E.H., Mullah-Ali A., Al-Sharidah S., Azab A.F., Adekile A. Infectious etiologies of transient neutropenia in previously healthy children. Pediatr Infect Dis J. 2012;31:575–577. doi: 10.1097/INF.0b013e318250084a. [DOI] [PubMed] [Google Scholar]
- 19.Karavanaki K., Polychronopoulou S., Giannaki M., Haliotis F., Sider B., Brisimitzi M. Transient and chronic neutropenias detected in children with different viral and bacterial infections. Acta Paediatr. 2006;95:565–572. doi: 10.1080/08035250500477537. [DOI] [PubMed] [Google Scholar]