As highlighted by Nianguo Dong (1), coronavirus disease-2019 (COVID-19) can cause myocardial injury. Putative mechanisms are acute coronary syndrome, demand ischemia, microvascular ischemic injury, cytokine dysregulation, or myocarditis (2). However, myocardial injury does not always correlate exclusively with COVID-19, and it may also reveal incidental cardiomyopathy. Thus, physicians must stay alert, and careful causative assessment is required in these patients. As contagious risk and patient instability may preclude initial work-up, reassessing the patient after the acute phase is of utmost importance. To illustrate, we report the case of an acute myocarditis with an underlying isolated ventricular noncompaction (IVNC) in a COVID-19 patient with heart failure.
A 27-year-old male without medical history was admitted for respiratory distress, and COVID-19 was diagnosed. High-sensitivity troponin I and N-terminal pro–B-type natriuretic peptide concentrations were elevated (100 ng/l and 9,300 pg/ml, respectively) suggesting myocardial involvement. In addition, echocardiography revealed an enlarged left ventricle with impaired left ventricle ejection fraction (LVEF) of 20%. The patient improved on a regimen of high-dose diuretic agents and noninvasive ventilation. He was discharged 9 days later with prescriptions for bisoprolol, furosemide, and spironolactone. One month later, his LVEF improved to 40% and showed normal filling pressure and cardiac output. Echocardiography revealed a 2-layered structure of the myocardium suggesting IVNC (3). CMR confirmed the IVNC diagnosis but also revealed acute myocarditis (Figure 1 ). Coronary computed tomography angiography results ruled out coronary artery disease. Patients with IVNC have variable prognosis, ranging from a prolonged asymptomatic course to severe cardiac disability. Prognosis is worse in patients hospitalized for heart failure, New York Heart Association functional classes III to IV, lower LVEF, and elevated LV filling pressures (4). Management involved treating the patient’s heart failure, and genetic screening of both the patient and family members was conducted.
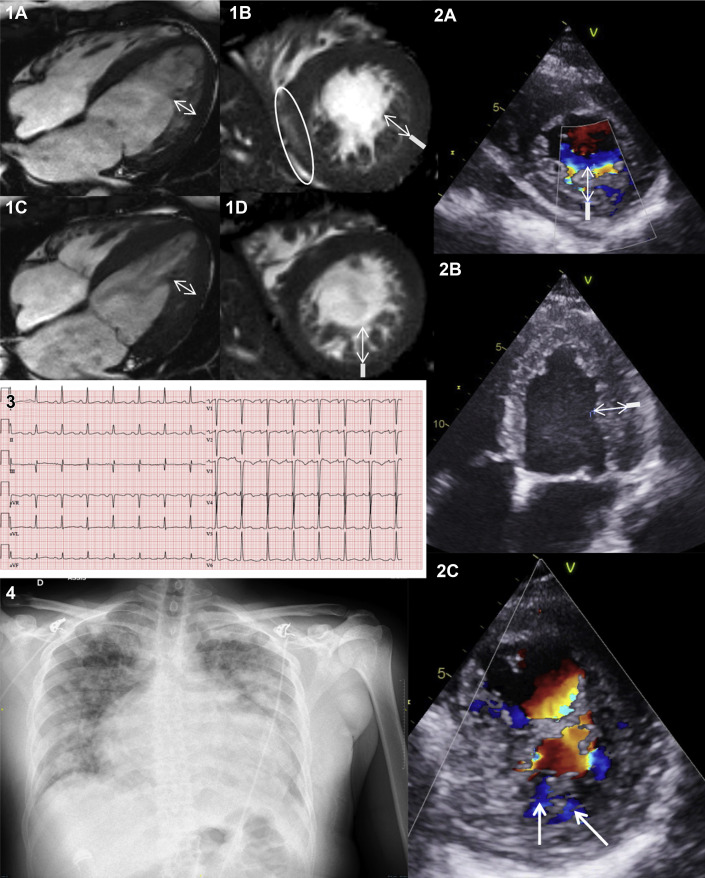
Figure 1.
Multimodal IVNC and Myocarditis
CMR. (1A and 1C) Four-chamber and (1B and 1D) middle short-axis views. Subepicardial late gadolinium enhancement in cine T2- or T1-weighted images suggesting acute myocarditis (open circle). Double-layered myocardium with a thin compacted epicardial layer (open line) and a thicker noncompacted endocardial band (double arrows) consisting of trabecular recesses suggesting IVNC. Transthoracic-echocardiography. (2A and 2B) Noncompacted endocardial layer (double white-arrows) and compacted layer (white lines). (2C) Trabecular recesses deeply perfused in color Doppler (open arrows). Electrocardiogram. (3) Sinus tachycardia, Q-wave and T-wave inversion in V1 to V3 leads, left axis deviation. Chest radiography. (4) Bilateral consolidation and significant heart enlargement. CMR = cardiac magnetic resonance; IVNC = imaging of ventricular noncompaction.
In this case, reassessing the patient after the COVID-19 acute phase allowed us to diagnose an underlying severe case of IVNC and subsequently initiate appropriate treatment and follow-up.
Footnotes
Please note: The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Heart Failureauthor instructions page.
References
- 1.Dong N., Cai J., Zhou Y., Liu J., Li F. End-stage heart failure with COVID-19: strong evidence of myocardial injury by 2019-nCoV. J Am Coll Cardiol HF. 2020;8:515–517. doi: 10.1016/j.jchf.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hendren N.S., Drazner M.H., Bozkurt B., Cooper L.T. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141:1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jenni R., Oechslin E., Schneider J., Attenhofer Jost C., Kaufmann P.A. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart. 2001;86:666–671. doi: 10.1136/heart.86.6.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Habib G., Charron P., Eicher J.-C. Isolated left ventricular non-compaction in adults: clinical and echocardiographic features in 105 patients. Eur J Heart Fail. 2011;13:177–185. doi: 10.1093/eurjhf/hfq225. [DOI] [PubMed] [Google Scholar]