Abstract
Objective
This study aimed to evaluate the protocol adopted during the emergency phase of the COVID-19 pandemic to maintain elective activity in a vascular surgery unit while minimising the risk of contamination to both patients and physicians, and the impact of this activity on the intensive care (IC) resources.
Methods
The activity of a vascular surgery unit was analysed from 8 March to 8 April 2020. Surgical activity was maintained only for acute or elective procedures obeying priority criteria. The preventive screening protocol consisted of nasopharyngeal swabs (NPS) for all patients and physicians with symptoms and for unprotected contact infected cases, and serological physician evaluations every 15 days. Patients treated in the acute setting were considered theoretically infected and the necessary protective devices were used. The number of patients and the possible infection of physicians were evaluated. The number and type of interventions and the need for post-operative IC during this period were compared with those in the same periods in 2018 and 2019.
Results
One hundred and fifty-one interventions were performed, of which 34 (23%) were acute/emergency. The total number of interventions was similar to those performed in the same periods in 2019 and 2018: 150 (33, of which 22% acute/emergency) and 117 (29, 25% acute/emergency), respectively. IC was necessary after 6% (17% in 2019 and 20% in 2018) of elective operations and 33% (11) of acute/emergency interventions. None of the patients treated electively were diagnosed with COVID-19 infection during hospitalisation. Of the 34 patients treated in acute/emergency interventions, five (15%) were diagnosed with COVID-19 infection. It was necessary to screen 14 (47%) vascular surgeons with NPS after contact with infected colleagues, but none for unprotected contact with patients; all were found to be negative on NPS and serological evaluation.
Conclusion
A dedicated protocol allowed maintenance of regular elective vascular surgery activity during the emergency phase of the COVID-19 pandemic, with no contamination of patients or physicians and minimal need for IC resources.
Keywords: COVID-19, Regular practice, Surgery, Vascular surgery
WHAT THIS PAPER ADDS.
This paper evaluates the protocol adopted during the emergency phase of the COVID-19 pandemic to maintain elective activity in a vascular surgery unit while minimising the risk of contamination to both patients and physicians. All elective patients were submitted to nasopharyngeal swabs; all emergency patients were considered as possibly contaminated, in order to minimise contamination possibilities to other patients and hospital professionals. This approach should be considered in an emergency situation in high risk areas.
Introduction
The pandemic infection of coronavirus disease 2019 (COVID-19) drastically reduced the normal activity of vascular surgery units in Italy over the first 30 days of national lockdown, with elective surgery maintained in only a few designated hospitals.1
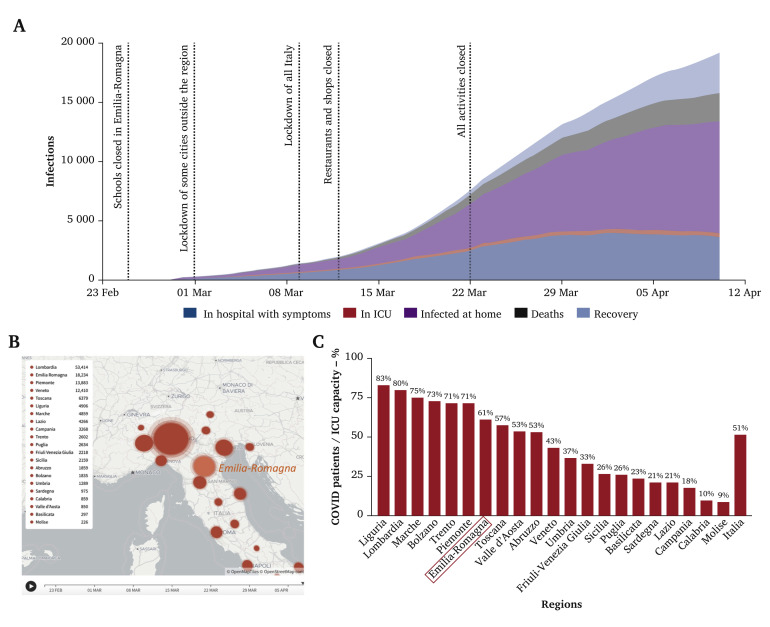
The national health system in Italy is directed by regional governance with specific and partially independent duties; Emilia-Romagna, with a population of 4.459 million people divided into nine provinces, had the second highest level of documented cases of COVID-19 infections, after Lombardia. In Emilia-Romagna, from 8 March to 8 April 2020, 18 000 infections were identified, with 3750 symptomatic patients admitted to hospital and 360 intensive care unit (ICU) beds, 61% of the overall available ICU beds in the region, occupied by patients with COVID-19 (Fig. 1 ).2 , 3
Figure 1.
Spread of infection of SARS-CoV-2 in the Emilia-Romagna region of Italy in February–April 2020. (A) Rise in infections, deaths, and recoveries in Emilia-Romagna and (B) geographical location of infections in Emilia-Romagna and other regions in Italy; panels modified from Ref.12. (C) Percentage of patients with COVID-19 in relation to intensive care unit (ICU) availability in different regions in Italy.
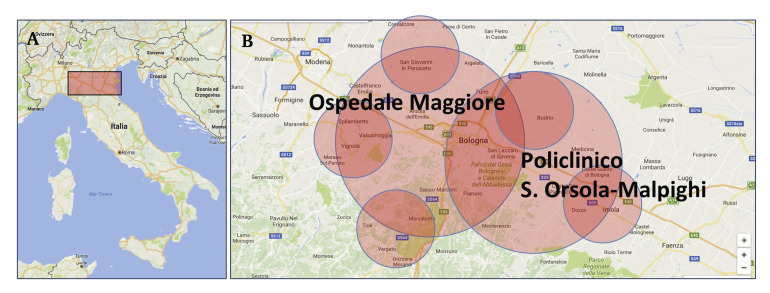
During the first month after the lockdown, all regional vascular surgery activities were limited to acute cases. Metropolitan vascular surgery in the city of Bologna, the main centre of the Emilia-Romagna region with about one million citizens, serves two tertiary hospitals, and provides service for five peripheral hospitals (Fig. 2 ). The healthcare system of the city of Bologna maintained some elective surgical activities during the pandemic emergency, such as cardiac, oncological, and vascular surgery; however, keeping patients undergoing such procedures separated from the COVID-19 patients posed a major set up challenge. In total across the city hospitals, 800 ward beds were reserved for patients with COVID-19, in addition to a total of 130 ICU beds (with a further 50 [60%] ICU beds in the two main hospitals). With the purpose of minimising physician and patient exposure to COVID-19, there was wide application of nasopharyngeal swabs (NPS) for nucleic acid based polymerase chain reaction (PCR) analysis to identify infected patients; patient isolation measures were also widely applied.4
Figure 2.
(A) Geographical location of Emilia Romagna region in Italy and (B) Bologna hospitals locations; panels modified from www.google.com/maps/@41.5453707,12.1086237,6z?hl=it and www.google.com/maps/@44.4531805,11.1198542,10z?hl=it, respectively (last accessed 10 April 2020).
The present study aimed to evaluate the protocol adopted during the emergency phase of the COVID-19 pandemic to maintain elective activity in a vascular surgery unit while minimising the risk of contamination to both patients and physicians and the ICU resources necessary to maintain such activity.
Methods
Period examined and vascular surgery activity
The period examined was from 8 March to 8 April 2020, covering the highest recorded rate of infections from COVID-19 in the Emilia-Romagna region in Italy. During this period, the healthcare system of the city of Bologna allowed continuation of elective arterial surgery according to a priority score similar to other countries,5 with the limitation of reducing to a minimum the need for post-operative ICU beds for electively treated patients. However, differently from other countries, regional directions identified with a similar priority score the treatment of symptomatic stenosis and that of asymptomatic high risk carotid stenosis (pre-occlusive stenosis, rapidly increasing stenosis). The vascular surgery team comprises 30 physicians, 15 consultants and 15 residents, and serves two tertiary hospital hubs (Policlinico Sant’Orsola-Malpighi and Ospedale Maggiore), connected with five peripheral hospitals within the metropolitan area of Bologna, home to one million citizens. During the lockdown period, the regional health system reduced most outpatient activities and stopped all venous disease procedures.
Considering the metropolitan vascular surgery activity as a whole, one hybrid room and two operating rooms (OR) were dedicated to vascular surgery elective activity every day (5/7). One other hybrid room and one other surgical OR were kept ready for patients with COVID-19 for both cardiac and vascular surgery activities. Negative pressure was maintained in all the ORs, as well as in most of the ICU. There was no specific air conditioning system in the wards; infected and non-infected patients were kept separate.
Protocols for COVID-19 infection prevention
Outpatient activities. These were limited to urgent visits and wound care; all other outpatient activities, such as duplex ultrasound examinations, follow up and first time clinical visits, were stopped, similar to all venous surgical procedures and non-urgent venous clinical visits (Table 1 ). Before entrance to the medical office, patient checkpoints evaluated possible patient symptoms and surgical masks were provided. Visits were scheduled to avoid patient crowding. All physicians attended the visits wearing surgical masks and using generous amounts of antiseptic gel.
Table 1.
Modification of vascular surgical activities during pandemic COVID-19 infection in the Emilia-Romagna region, Italy, from 8 March to 8 April 2020
| Activity | Modification |
|---|---|
| Outpatient visit arterial disease | Closed |
| Wound care | Reduced |
| Duplex lab | Closed |
| Outpatient urgent visit | Maintained |
| Clinical consultation in hub hospitals | Maintained |
| Clinical consultation in peripheral hospitals | Maintained |
| Elective surgery for arterial disease | Maintained |
| Elective surgery for venous disease | Closed |
| Urgent emergency surgery | Maintained |
| Support to ICU activities | New activity |
ICU = intensive care unit.
Elective surgery. All patients already in hospital in the vascular surgery ward and awaiting intervention had NPS in case of fever or cough or close contact with other COVID-19 positive patients. All new elective admissions had NPS the day before admission.
All patients with suspected COVID-19 were isolated in dedicated rooms and had NPS. Patients with fever or cough or radiological signs of pneumonia were considered suspicious for COVID-19 and had three NPS taken serially on day 1, day 3, and 15 days after initiation of symptoms, to reduce the risk of false negative results.6 Possible other causes of fever, for example foot infection, were not considered a valid reason to avoid NPS testing. All elective operations were planned and executed only in patients negative for COVID-19. Patients admitted for elective surgery met priority criteria, with a request from the public health system to limit the planned use of ICU (Table 2 ). All patients admitted to hospital wore surgical masks at all times.
Table 2.
Priority criteria for elective vascular surgery during pandemic COVID-19 infection in the Emilia-Romagna region, Italy, from 8 March to 8 April 2020
| Vascular surgical activity | Priority criteria |
|---|---|
| Carotid artery stenosis | Symptomatic or asymptomatic sub-occlusive or rapidly growing plaque (the rapid increase of stenosis from less than 60%, according to NASCET criteria, to >90% in the last year) |
| Peripheral artery disease | Critical limb treating ischaemia, Rutherford 5–6 or symptomatic peripheral artery aneurysms |
| Aortic aneurysm | Large diameter aneurysm (>6 cm [maximum diameter] abdominal aortic aneurysm or >7 cm thoracic aortic aneurysm) |
| Arteriovenous fistula for haemodialysis | Cases of fistula malfunction or new fistula in patients requiring a haemodialysis vascular access in the next month |
NASCET = North American Symptomatic Carotid Endarterectomy Trial Collaborators.11
Acute/emergency surgery. All patients who underwent acute/emergency surgery were considered to be potentially positive for COVID-19. All patients had NPS before the intervention or immediately after it, if not possible before. The patients were maintained in isolation until the response from the first NPT-PCR analysis. For clinical suspicion of infection (fever, cough contact with patients positive for COVID-19), patients were maintained in isolation until the third NPS after two weeks.6 Two operating rooms, one surgical and one hybrid, were constantly kept ready for the treatment of a patient with COVID-19, with only very essential surgical material inside and all fixed devices protected by plastic removable covers (Fig. 3 ), with a dedicated area for individual protection device exchange.
Figure 3.
(A) Fast track preparation area for COVID-19 patient acute/emergency vascular surgery and (B, C, D) pre-emptive isolation of hybrid room devices for COVID-19 patient acute/emergency intervention in Emilia-Romagna region, Italy, in 2020.
Protocols for COVID-19 infection prevention for physicians
All physicians performed activities wearing surgical masks and with generous antiseptic gel washing during all activities, according to recommendations from the World Health Organization (Table 3 ). All face to face meetings were substituted by video conferences. For a patient with COVID-19 infection or suspicion of infection, all manoeuvres and protection devices were set to minimise the risk of contamination: double surgical cap, FFP2 mask, facial shield, and complete body and leg coverage, all according to current recommendations.7
Table 3.
World Health Organization recommendations for healthcare in contact with patients with COVID-19
| Activity | Type of personal protective equipment |
|---|---|
| Providing direct care to patients with COVID-19 | Medical mask |
| Eye protection (goggles or face shield) | |
| Gown | |
| Gloves | |
| Aerosol generating procedures performed on patients with COVID-19 | Respirator N95 or FFP2 standard, or equivalent |
| Eye protection | |
| Apron | |
| Gown | |
| Gloves |
Physicians underwent NPS after contact with patients or other health professionals positive for COVID-19 without the appropriate protection devices. General screening of physicians with NPS was not performed.
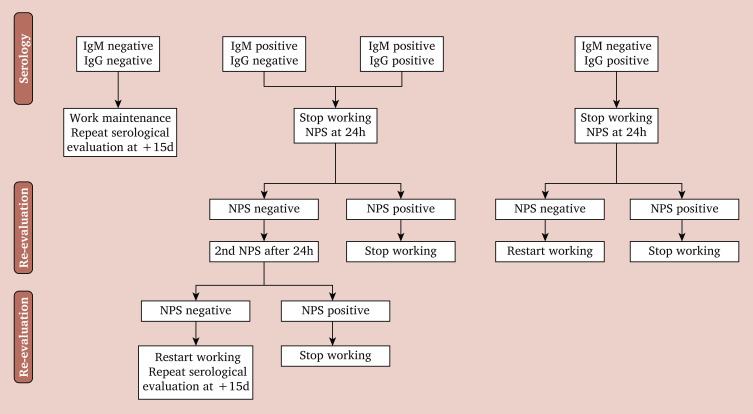
From 30 March, sequential (every two weeks) physician serological IgG and IgM screening was initiated and NPS performed for IgM positive cases (Fig. 4 ).
Figure 4.
Flow chart for serological evaluation for immunoglobulins M and G (IgM and IgG) of vascular surgeons and further use of nasopharyngeal swabs (NPS) during pandemic COVID-19 infection in Emilia-Romagna region, Italy, from 8 March to 8 April in 2020.
Evaluation of the protocols for COVID-19 infection prevention and surgery activities
For the evaluation of the protocols adopted, the number of positive cases among patients submitted to elective surgery and among the vascular surgery team was recorded. The surgical activity and the need for ICU (election and acute/emergency) was compared with the same periods from 2019 and 2018.
Results
Evaluation of surgical activities
In the first 30 days of lockdown, the Bologna metropolitan vascular surgery unit performed a total of 151 interventions, 34 (23%) of which were in the emergency or acute settings. Compared with the same period in 2019, the number of arterial interventions was lower with 150 cases treated, of which 33 (22%) were in the acute setting. Table 4 summarises the interventions performed.
Table 4.
Vascular surgical activity in the Emilia-Romagna region, Italy, from 8 March to 8 April during the pandemic COVID-19 infection in 2020 compared with years 2018 and 2019
| Intervention | Patients in one month observation period – year |
||
|---|---|---|---|
| 2020 (n = 152) | 2019 (n = 150) | 2018 (n = 117) | |
| Elective∗ | 118 | 117 | 88 |
| Carotid disease | 43 (36) | 17 (15) | 20 (23) |
| Peripheral artery disease | 51 (43) | 61 (52) | 35 (40) |
| Aortic aneurysm | 8 (7) | 16 (14) | 18 (20) |
| Peripheral aneurysm | 3 (3) | 5 (4) | 1 (1) |
| Arteriovenous fistula | 13 (11) | 17 (15) | 14 (16) |
| Acute/emergency† | 34 | 33 | 29 |
| Carotid disease | 3 (9) | 1 (3) | 2 (7) |
| Peripheral artery disease | 10 (29) | 12 (37) | 7 (24) |
| Aortic aneurysm | 8 (24) | 6 (18) | 8 (28) |
| Bleeding/haematoma | 9 (26) | 5 (15) | 4 (14) |
| Acute ischaemia | 2 (6) | 9 (27) | 5 (17) |
| Trauma | 2 (6) | 0 (0) | 3 (10) |
Data are provided as n (%).
Percentages calculated among elective patients.
Percentages calculated among acute/emergency patients.
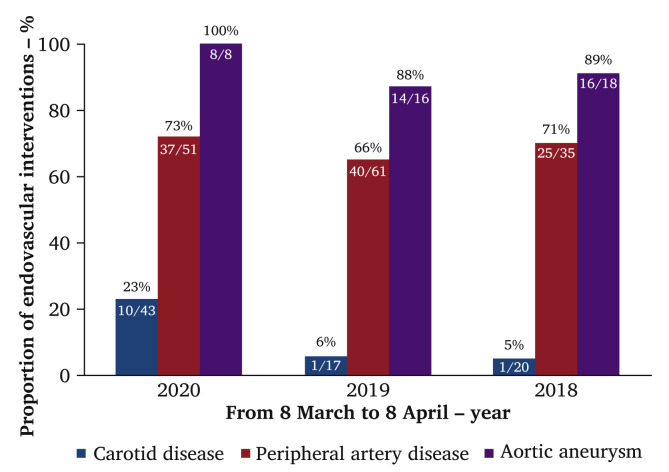
All the abdominal aortic aneurysms were larger than 6 cm in diameter or were rapidly increasing (>1 cm/year). All the arteriovenous fistulas were considered to be high priority by the nephrologist. All the peripheral arterial occlusive disease (PAOD) cases had critical ischaemia with gangrene and the peripheral artery aneurysms were symptomatic. The patients with carotid stenosis were symptomatic in 20 cases and asymptomatic in 23 (in 10 cases carotid artery stenting was performed because of the high location [four], presence of chronic obstructive pulmonary disease [four], one post-actinic lesion, and one paralysis of the ispilateral vocal cord from previous thyroid surgery). Fig. 5 shows the percentage of endovascular elective treatments in the periods examined. The elective mortality was zero in all years examined, with one death after ruptured abdominal aortic aneurysm repair in both 2019 and 2020. In 2018 two deaths occurred, one in a patient with critical limb ischaemia submitted to tibial angioplasty and forefoot amputation and one for multiorgan failure for sepsis after a peripheral bypass.
Figure 5.
Percentage of elective endovascular interventions from all vascular interventions in Emilia-Romagna region, Italy, from 8 March to 8 April during pandemic COVID-19 infection in 2020 and in years 2018 and 2019.
Acute/emergency surgery for acute ischaemia was not increased: 2/34 in 2020 and 9/33 in 2019. Post-operative ICU was necessary in 6% (n = 7) of elective operations, which is lower than in the same period of 2019, and in 33% (n = 11) of acute/emergency operations (Table 5 ).
Table 5.
Intensive care unit (ICU) bed requirement for elective and urgent/emergency vascular surgery in the Emilia-Romagna region, Italy, from 8 March to 8 April during pandemic COVID-19 infection in 2020 and in the years 2018 and 2019
| Patients needing ICU bed | Year 2020 |
Year 2019 |
Year 2018 |
|||
|---|---|---|---|---|---|---|
| Patients n (%) |
Median length of stay (IQR) – d | Patients n (%) |
Median length of stay (IQR) – d | Patients n (%) |
Median length of stay (IQR) – d | |
| Elective surgery | 7/118 (6) | 2 (2) | 20/117 (17) | 3 (2) | 18/88 (20) | 3 (2) |
| Peripheral artery disease | 2 | 6 | 8 | |||
| Aortic aneurysm | 5 | 14 | 10 | |||
| Acute/emergency surgery | 11/34 (32) | 3 (2) | 10/33 (30) | 3 (2) | 13/29 (45) | 3 (2) |
| Aortic aneurysm | 8 | 6 | 8 | |||
| Bleeding/haematoma | 2 | 3 | 2 | |||
| Acute ischaemia | 1 | 1 | – | |||
| Trauma | – | – | 3 | |||
ICU = intensive care unit; IQR = interquartile range.
No patients undergoing elective operations developed COVID-19 infection during hospitalisation; one patient admitted for elective surgery for aortobifemoral graft removal for graft infection was found to be positive for COVID-19 and the procedure was postponed. The patient was admitted with fever, which was initially attributed to the graft infection; however, she was preventively isolated even though two previous NPS-PCR had been performed in a peripheral hospital and had been negative for COVID-19 infection.
Of the 34 patients treated in the acute/emergency setting, five (15%) were positive: three of these patients were known to be positive before the intervention, one patient in the COVID-ICU with acute ischaemia caused by aortic thrombosis and peripheral embolisation, one patient in the COVID-ICU with malposition of central vein catheter in the subclavian artery, and one patient admitted with suspected femoral patch infection. The other two acute cases were identified to be positive for COVID-19 after the intervention: one case of severe foot infection in a diabetic patient with peripheral artery disease, and one patient with brachial artery bleeding.
Physician infection screening
Thirty physicians, 15 consultants and 15 residents, were working in the metropolitan vascular surgery unit. All the physicians had contact with patients with COVID-19 infections for interventions, wound care, and support in the ICU, but as the contact always occurred with appropriate protection, the physicians did not have NPS in most cases. However, 14 physicians (46%) were screened with NPS and found to be negative. All the NPS were performed following contacts with colleagues, one anaesthetist and one cardiac surgeon, who were identified positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) before the onset of symptoms. All physicians were tested and results were negative for both IgG and IgM.
Discussion
The present study aimed to evaluate organisation of a vascular surgery unit, attempting to maintain a normal volume of elective activity during the COVID-19 pandemic. This work is observational and limited to a short time, however it may help planning the activity of other units at different times of contamination.
The Emilia-Romagna region had the second highest number of COVID-19 infections in Italy, after Lombardia; by 8 April, the official number of patients infected was 18 000, diagnosed by 78 000 NPS, with 3750 patients admitted to hospitals and 360 receiving intensive care. The infection mortality rate was 12%, for a total number of 2234 deaths.2 The availability of ICU beds in Emilia-Romagna is usually 449, with an increase to 573 (+124/+28%) during the pandemic phase. Three hundred and sixty/573 ICU (i.e. 63% of the total) beds were for patients with COVID-19 on 8 April; fortunately, a decrease in this number began after this date.3 The healthcare system organisation allowed maintenance of selected elective surgery activities: cancer surgery, cardiac surgery and vascular surgery for pathologies with a top priority level, as designated in non-pandemic time, with cessation of most outpatient activities and all venous surgical procedures. The metropolitan vascular surgery unit of Bologna was the only one in the region performing elective surgery, accepting patients planned for surgery at the vascular surgery unit.
During a pandemic, any elective surgical activity requires specific attention to avoid patient and physician infections. The primary approach to avoid in hospital infection was to submit all pre-pandemic in hospital patients with history of risky contacts or symptoms to NPS, as well as all newly admitted patients. Use of isolation and protection devices for any acute/emergency surgery case and in all patients potentially contaminated prevented the spread of COVID-19 infection to other patients and to the vascular surgery team, despite five interventions (34% of acute/emergency cases) being performed on patients positive for COVID-19.
Physicians were submitted to NPS only after close contact with other healthcare professionals with infection or unprotected contacts with infected patients. The need for scrupulous and constant screening of the healthcare personnel is therefore fundamental to avoid in hospital contamination. Standardisation and validation of screening criteria is of paramount importance in an ideal prevention plan.
If an efficient safety protocol can be set to minimise the risk of infections for patients and physicians, elective vascular surgical activity can be maintained. In the present authors’ experience, the number of surgical interventions performed was similar compared with the same periods in 2019 and 2018; aortic interventions were kept to a minimum to spare ICU resources, which were maintained for complex endovascular repair or patients with abdominal aortic aneurysms >6 cm, a similar number of critically ischaemic limbs and an increasing number of carotid interventions for symptomatic and rapidly evolving asymptomatic stenoses The latter were maintained because of their low impact on hospital resources, scarce or no need for post-operative ICU, easy scheduling, and high priority in the recommendations of many regional health systems in Italy.8 Concerning these recommendations, the present authors have recently suggested an extensive revision of the priority scale, following current scientific evidence in particular for carotid interventions for asymptomatic patients but their treatment remains an objective for the regional health system. Patients requiring carotid intervention were also recruited from peripheral hospitals. A similar number of interventions was performed in the acute/emergency setting compared with previous years; an increase in the number of interventions for acute ischaemia (one in a patient positive for COVID-19) was not seen, despite the potential effect of the infection on thrombogenic mechanisms and the report of a higher number of cases of acute ischaemia: data are occasionally reported with a possible role for COVID-19 in determining a hypercoagulable condition.9 It is important to select as many patients as possible not requiring post-operative intensive care, to spare those resources for COVID-19 complications. In the present series only seven elective cases required ICU, with a median stay of two days. Keeping the use of strategic resources such as ICU beds for COVID-19 patients in the pandemic period is a key element; current advances in vascular and endovascular surgery allow a very effective response to this need.10
The present study has some limitations such as the scarce number of procedures and its retrospective nature, and moreover the present data are not associated with a control group to evaluate the real efficacy of the protocols adopted. Another element of reflection is the rate of false negative tests, which can lead to spread of the infection despite precautions.
The present study evaluated the protocol adopted in the emergency phase to maintain elective vascular surgery activity, while minimising risk of contamination to patients and physicians. This short experience suggests that extensive use of NPS and serological analysis will help to prevent any infection.
Conflicts of Interest
None.
Funding
None.
References
- 1.Italian Society for Vascular and Endovascular Surgery Il Monitoraggio SICVE su Covid 19. Post del Consiglio Direttivo. www.sicve.it/il-monitoraggio-sicve-su-covid-19-post-del-consiglio-direttivo/ Available at:
- 2.National Italian Public Heath Office Covid-19 - situazione in Italia. www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?lingua=italiano&id=5351&area=nuovoCoronavirus&menu=vuoto Available at:
- 3.Emilia-Romagna Public Heath Office Posti di terapia intensiva in Italia : TI in Italia. https://docs.google.com/spreadsheets/d/1EPoJ_T221tEy0K5QTkaZKjA-lHo9VAEr6rFPJ_Qdtds/htmlview#gid=0 Available at:
- 4.Poljak M., Korva M., Knap Gašper N., Fujs Komloš K., Sagadin M., Uršič T. Clinical evaluation of the cobas SARS-CoV-2 test and a diagnostic platform switch during 48 hours in the midst of the COVID-19 pandemic. J Clin Microbiol. 2020 doi: 10.1128/JCM.00599-20. JCM.00599-20 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Surgeons COVID-19 guidelines for triage of vascular surgery patients. www.facs.org/covid-19/clinical-guidance/elective-case/vascular-surgery Available at:
- 6.Winichakoon P., Chaiwarith R., Liwsrisakun C., Salee P., Goonna A., Limsukon A. Negative nasopharyngeal and oropharyngeal Swabs do not rule out COVID-19. J Clin Microbiol. 2020;58:e00297–20. doi: 10.1128/JCM.00297-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19) https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf Available at:
- 8.Chisci E., Masciello F., Michelagnoli S. Creation of a vascular surgical hub responding to the COVID-19 emergency: the Italian USL Toscana Centro model. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.019. S0741–5214(20)30605–4. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y., Xiao M., Zhang S., Xia P., Cao W., Jiang W. Coagulopathy and antiphospholipid antibodies in patients with covid-19. N Engl J Med. 2020;382 doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Björck M., Boyle J.R., Dick F. The need of research initiatives amidst and after the covid-19 pandemic: a message from the editors of the European journal of vascular and endovascular surgery. Eur J Vasc Endovasc Surg. 2020;59:695–696. doi: 10.1016/j.ejvs.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Barnett H.J.M., Taylor D.W., Haynes R.B., Sackett D.L., Peerless S.J., Ferguson G.G. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 12.GEDI VISUAL Coronavirus, the situation in Italy. https://lab.gedidigital.it/gedi-visual/2020/coronavirus-i-contagi-in-italia/ Available at: