On January 14, 2020 the first case of COVID-19, the disease caused by the SARS-CoV-2 virus, was confirmed in the United States.1 In the subsequent weeks the virus spread rapidly and ultimately the World Health Organization (WHO) made the assessment that COVID-19 could be characterized as a pandemic.2 As part of the effort to curb the spread of virus and prioritize resources for screening and treatment of patients, the Centers for Medicare and Medicaid Services (CMS), most states, and some professional organizations including the American College of Surgeons (ACS) made the recommendation that elective surgery should be postponed. Hospital leaders and surgeons rapidly made arrangements with patients to postpone surgery whenever appropriate.
Now, as most regions of the country are beyond the peak of the pandemic, surgeons and hospital leaders are beginning to think about how to safely and effectively resume elective surgery.3 Because thousands of surgical procedures have been delayed, providers are balancing the pent up need for elective surgery versus available supplies and workforce, all the while trying to mitigate the risk of exposure and spread of the virus. This unprecedented event has left surgeons without a roadmap for safely navigating the road to recovery. Previously, we presented a framework regarding how to navigate the decision and implementation to delay elective procedures – comply with guidelines, leverage content experts, frequently assess disease burden and resources available, and consider immediate local needs while being sensitive to national needs.4 Here we provide surgeons with special considerations and specific examples from our institution (Table 1 ) as a roadmap to recovery for elective surgery.
Table 1.
Institutional playbook for Administrative and Surgical Staff for rescheduling elective surgery.
| Surgical Staff |
Administrative staff |
|
|---|---|---|
| Before Telehealth Visit | ||
|
|
|
|
Date of Telehealth visit | ||
|
|
|
|
After Telehealth Visit | ||
|
|
|
Initiating recovery
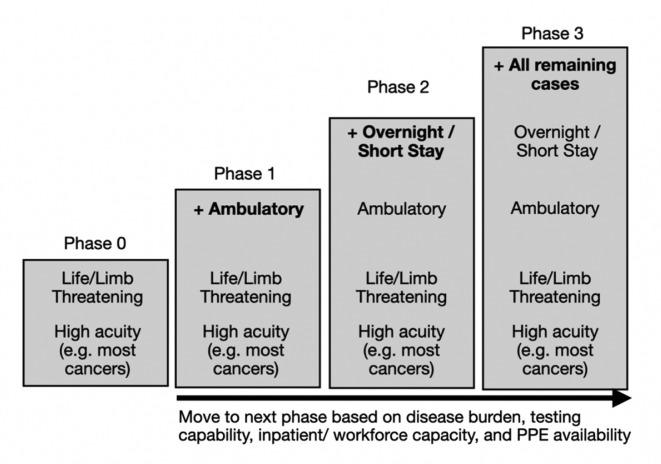
Similar to the implementation of ramping down elective surgical procedures, many states have provided either executive orders or guidelines regarding the timing of resuming surgery.5 As before, surgeons and hospital leaders should comply and work with their state and public health officials to establish a safe strategy for resuming surgery. What constitutes an elective or non-essential surgical procedure will vary to some degree across states and even among organizations. Regardless of definition, cases should be resumed in a graduated fashion (Fig. 1 ) as the outbreak subsides, as COVID-19 will be persistent and “hot-spot outbreaks” or local surges are still possible. Surgeons should work to develop comprehensive protocols and plans for each phase of recovery, as well as identify prior indicators that may signal a second wave or resurgence of COVID-19. Most importantly, ramping up will require centralized planning to model phased demand and capacity, anticipate and address operational hurdles, and roll out a plan acceptable to staff and patients.
Fig. 1.
Institutional phases for reimplementing elective surgery.
Despite approval to resume elective/non-essential surgery at the state level, hospital leaders and surgeons need to assess independently their specific medical center disease burden, local hospital resources, as well as the available workforce prior to making decisions to resume non-essential surgery. For instance, hospitals in regions of a state that have been largely spared of COVID-19 may be ready to resume surgery at a different pace than hospitals in heavily affected areas. The varying incidence and prevalence of COVID-19 in any given local area needs to be weighed relative to the risk to patients (e.g. peri-operative complications, disease progression) and providers (e.g. exposure to COVID-19). In turn, resuming elective non-essential cases should include a review of the incidence of new COVID-19 cases in the relevant geographic area, the availability of appropriate numbers of intensive care unit (ICU) and non-ICU beds at a given hospital, availability of personal protective equipment (PPE) and ventilators, as well as the available compliment of trained staff to perform non-essential surgical procedures without taxing resources needed to deal with the ongoing COVID-19 crisis.
Before initiating non-essential surgery, facilities should establish a policy and procedure for preoperative COVID-19 testing. In particular, due to the risk of asymptomatic patients being positive for COVID-19, all asymptomatic patients undergoing a non-emergent surgery or procedure that is “high-risk for aerosol generation” must undergo COVID-19 testing prior to a surgery or procedure. Other asymptomatic patients not meeting these criteria may be tested for COVID-19 at the request of the provider performing the surgery or procedure. Patients having elective surgery are tested at one of the outpatient swab sites. At our institution we utilize a polymerase chain reaction (PCR) based protocol because in most instances the test the rapid antibody test has a lower accuracy especially among asymptomatic patients.6 Timing of the COVID-19 swabbing test depends on the patient’s day of surgery. At our medical center, the patient needs to obtain their test 72–120 hours prior to surgery to ensure adequate time for the test to result prior to surgery. It is expected that the patient will remain at home except to minimize contact with other individuals, including those in their household, between the time of the COVID-19 testing and the planned procedure. As such, ancillary testing (e.g. blood work, imaging) related to the surgery/procedure need to be scheduled prior to COVID-19 testing. In turn, the considerable logistics of contacting and screening patients, as well as organizing COVID-19 testing prior to surgery needs to be tackled early. Additionally, facilities should establish policies that address the indications, requirements, and frequency for staff to be tested for COVID-19. Protocols to notify and guide patients who have a COVID-19 positive test need to be put into place prior to initiating non-essential surgery. Specifically, policies around proceeding versus delaying non-essential surgical procedures in COVID-19 patients need to be discussed and protocolized.
Facilities should resume non-essential surgical procedures only if there is adequate PPE and medical surgical supplies with respect to the number and types of procedures that will be performed. In particular, medical centers should leverage local electronic medical record data to build resource utilization tools. These tools can include historical data on metrics such as inpatient length of stay, ICU utilization, blood utilization, ventilator utilization, readmission rates, emergency department visit rates, and discharge to other inpatient facilities.7 Use of such data analytic tools can provide accurate estimates of anticipated resource utilization and help approximate the resources that may be need to perform different types of cases. In turn, such models can allow for assessment of supply and demand relative to the type of non-essential cases being re-booked. Cases that require relatively little resources such as example ambulatory cases that will not require an overnight stay should be prioritized as part of the initial phase of ramping up. As the COVID-19 disease burden continues to decrease and resources become more available, then facilities may precede with cases that will require more resources. Each phase of recovery should be predefined based on disease burden, resources, supplies, and workforce available, as well as projected utilization of resources and supplies related to the projected new surgical volume. At our institution, moving from one phase to another phase of recovery occurs in a stepwise fashion. Specifically, moving to a new phase only occurs after reevaluating policies, data, and metrics gathered during the current phase (Fig. 1).
Case prioritization and patient engagement
Facilities will need to either develop or leverage existing data collection systems to track postponed cases and to minimize loss to follow-up. These systems should be updated regularly to reflect clinical urgency, reevaluation of patient symptoms/disease status, as well as consider other factors (e.g. chemotherapy or anticipated postoperative non-home discharge). To this end, facilities should create steering committees to help design protocols to prioritize case scheduling (Table 1). At our institution postponed cases are rescheduled using priority scoring systems that consider 1) the patient’s desire to proceed with non-essential surgery 2) clinical urgency of the clinical diagnosis 3) resources required to do the case (e.g. PPE, staff, number of hospital days, etc.), and 4) length of delay that the patient has already experienced due to the COVID-19 postponement. Some hospitals have begun to utilize the Medically-Necessary, Time-Sensitive (MeNTS) scoring system, or a modification thereof, to help prioritize postponed cases.8 Alternatively, facilities may develop their own objective scoring system based on case specific historical institutional data to help prioritize cases in a way that is equitable and sensitive to resource allocation. At our institution we have developed our own scoring system by leveraging our experts, the electronic health record, and data warehouse management to develop a proprietary, objective scoring system (Fig. 2 ). The scoring system considers patient characteristics in addition to historical case specific data (e.g. operative time, length of stay).
Fig. 2.
Example of possible worksheet to help stratify patients for re-scheduling of surgery.
In many instances, patients originally scheduled for ambulatory surgery (i.e. outpatient) should be scheduled first for a telehealth visit (i.e. video visit). Within the non-essential ambulatory group of postponed cases, consideration may be given to prioritizing those patients who have waited the longest (i.e. had their operation postponed the earliest). Patients originally scheduled for non-ambulatory surgery (i.e. extended recovery, overnight stay, or inpatient) can also be scheduled for a telehealth visit, yet typically after scheduling ambulatory surgery patients who are involved in phase 1 of recovery. A protocol for patient preference for timing of rescheduling their operation should be established. For example, some patients may not want to pursue rescheduling their operation at the moment and may not want to initiate further discussion about rescheduling in the future. Alternatively, other patients may be unsure about rescheduling their operation at the current time, but would likely reschedule at a later date; other patients may want to proceed with rescheduling immediately. At our institution, we are utilizing a green/yellow/red light system to identify and track patients desire to have their non-essential surgery re-scheduled (Table 1).
Once patients have been contacted and are agreeable to rescheduling their non-essential surgery, providers can use telemedicine approaches to perform the preoperative assessment. In the instance in which a patient may not have access to telehealth, providers do have “in-person” clinics at which appropriate precautions are taken. Surgeons should discuss and confirm the indications and need for surgery including the impact of symptoms on quality of life and non-surgical options. Discussions about the patient’s current health situation and pertinent changes from the previous clinical visit, including the need to reschedule any required ancillary testing and/or evaluation, should also be undertaken. During the preoperative re-evaluation an updated inform consent should be discussed. We have implemented an updated informed consent process that includes an explicit discussion about the steps the institution has taken to mitigate the risk of contracting COIVD-19 during the elective surgery, including pre-operative testing, daily screening of staff, and use of appropriate PPE. Patients should also be informed about visitor restrictions. Our institution has a “No Visitor” policy which extends to elective ambulatory surgery. For major inpatient surgery, one person is allowed to accompany a patient on the day of surgery and one day after surgery. During surgery, family/visitors are required to wait off site so as to avoid congregation and to encourage social distancing. Additionally, the provider should discuss that contracting COVID-19 could affect the post-operative recovery process and that rehabilitation services and post-operative care may be provided utilizing virtual visits or telephone visits in order to limit in-person interactions. At our institution, we have instituted a separate COVID-19 specific informed consent form.
On the day of surgery, facilities should establish a “virtual” waiting room to avoid large groups and congregation. Facilities should have social distancing policies for staff, patients and visitors in non-restricted areas that include the number of people who can accompany patients and whether visitors in periprocedural areas should be further restricted. A system to inform and update family members and visitors should be established. After surgery and recovery, patients should ideally be discharged home and not to nursing homes as rates of COVID-19 are higher in those facilities. Patients should be made aware that postoperative visits may need to occur virtually unless there is a concern or indication that needs to be addressed in person. Postoperative visit schedules are highly variable and dependent on patient, disease, and surgery specific nuances. Postoperative visits are conducted by either the operating surgeon or, when appropriate, an advanced practice provider. These visits are, whenever possible, completed via telehealth. In general, these telehealth visits are conducted via a televideo medium; however, if video access is not feasible then a telephonic visit is conducted, as virtually every patient has a phone. In the circumstance where a telehealth visit is not feasible, or an inpatient visit is medically necessary, then an in-person visit is facilitated. In addition, post-operative patients are given instructions about COVID-19 symptoms and are instructed to call the COVID-19 hotline if they develop these symptoms.
Data collection and management
With the resuming of elective surgery, medical centers should have the infrastructure in place to capture and manage data as it pertains to resource availability, as well as the ability to procure additional resources in the event of a second wave of COVID-19. Post-operative patients should be followed closely, not only for postoperative complications but also for symptoms of COVID-19. Policies and procedures should be in place in the event that a patient becomes symptomatic or tests positive for SARS-Cov-2. For instance, policies need to take into account not only testing exposed staff, but also notifying and testing other patients who may have been exposed (i.e. contact tracing). Facilities should reevaluate policies around COVID-19 testing, resources, and other clinical information since information will continue to evolve quickly. Leaders need to be closely attuned to the possibility of a resurgence or second wave. As social distancing recommendations are relaxed throughout the country in the coming weeks, the possibility of increasing spread remains a real possibility. Any indication of such an event should trigger a reevaluation of non-essential surgical procedures.
Conclusion
As we move forward on the road to recovery, surgeons must weigh the tradeoffs between providing surgical care to their patients with the risk of spreading the virus. The decision regarding when and how to resume non-essential surgery is one that should be made at the state level with input from local medical center leadership. Furthermore, the ultimate decision to undergo surgery should be made by each patient, only after having a thorough and honest conversation about risks – including those associated with COVID-19 – and benefits related to the non-essential procedure being considered.
Disclosures
None.
Funding
Dr. Diaz receives funding from the University of Michigan Institute for Healthcare Policy and Innovation Clinician Scholars Program and salary support from the Veterans Affairs Office of Academic Affiliations during the time of this study.
Disclaimer
This does not necessarily represent the views of the United States Government or Department of Veterans Affairs.
References
- 1.CDC. Cent. Dis. Control Prev. 2020 https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/previouscases.html [Google Scholar]
- 2.Anon. https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- 3.Shao C. The COVID trolley dilemma. Am J Surg. 2020;220(3):561–565. doi: 10.1016/j.amjsurg.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diaz A., Sarac B.A., Schoenbrunner A.R. Elective surgery in the time of COVID-19. 2020. http://www.sciencedirect.com/science/article/pii/S000296102030218X [Internet]. Am. J. Surg. [Internet] [DOI] [PMC free article] [PubMed]
- 5.Anon. https://coronavirus.ohio.gov/wps/portal/gov/covid-19/resources/news-releases-news-you-can-use/elective-surgery-order-mental-health-careline
- 6.Anon. NPR.org. https://www.npr.org/sections/health-shots/2020/05/01/847368012/how-reliable-are-covid-19-tests-depends-which-one-you-mean
- 7.Michigan value collaborative. https://michiganvalue.org/wp-content/uploads/2020/04/MVC-Resource-Utilization.pdf
- 8.Prachand V.N., Milner R., Angelos P., Posner M.C., Fung J.J., Agrawal N., Jeevanandam V., Matthews J.B. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020 Apr 9 doi: 10.1016/j.jamcollsurg.2020.04.011. pii: S1072-7515(20)30317-3; [Epub ahead of print] PubMed PMID: 32278725; PubMed Central PMCID: PMC7195575. [DOI] [PMC free article] [PubMed] [Google Scholar]