Abstract
Patients infected with the new SARS-CoV-2 appear to be associated with higher risk of thromboembolic disease, especially stroke and pulmonary embolism. We report a case of a 79-year-old woman that presented with stroke and was found to have COVID-19 pneumonia and concomitant large burden pulmonary arterial clot. Early imaging of suspected thromboembolic disease may lead to improved patient morbidity and mortality.
Keywords: Covid-19, Thromboembolic disease, Pulmonary embolism, Stroke
Introduction
The outbreak of coronavirus disease (COVID-19) was first reported in Wuhan, China, in December 2019, and has quickly reached pandemic levels in the United States. Coronavirus disease is a highly contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and appears to be associated with increased thrombotic disease [1], [2], [3]. The novel coronavirus is theorized to cause both venous and arterial thromboembolic disease due to a cytokine cascade causing excessive inflammation, hypoxia, immobilization, and diffuse intravascular coagulation [2], [3], [4]. We present a unique case of a 79-year-old COVID positive female with imaging features of simultaneous acute pulmonary embolism and stroke secondary to large intracranial vessel occlusion.
Case presentation
A 79-year-old, previously functionally independent female with a past medical history of hypertension, hyperlipidemia, and diabetes, was brought to the emergency department with slurred speech and left-sided weakness upon awakening. She was last known well about 8 hours prior. On examination, she was found to have aphasia and left hemiparesis with a National Institutes of Health Stroke Scale (NIHSS) of 21. She was afebrile, had a normal sinus rate and rhythm, but tachypneic with an oxygen saturation of 88%.
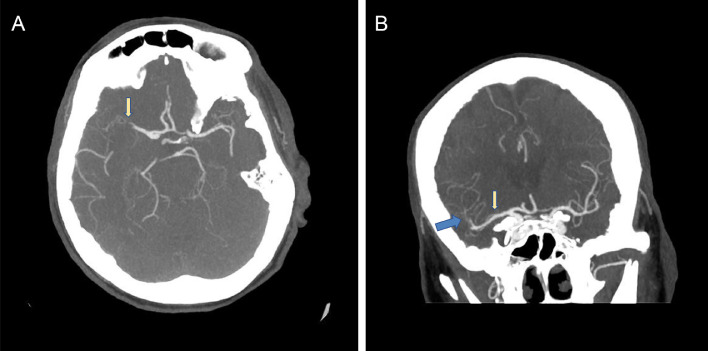
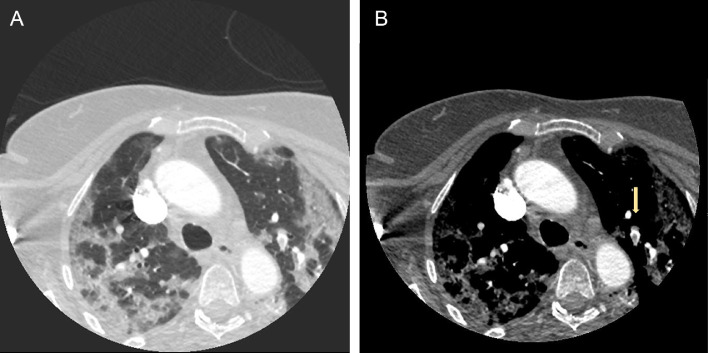
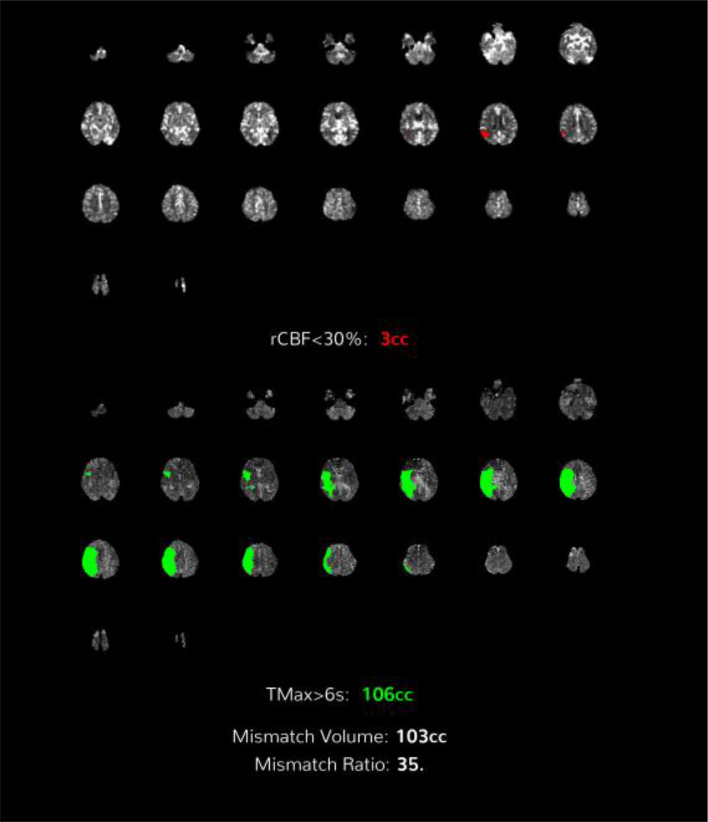
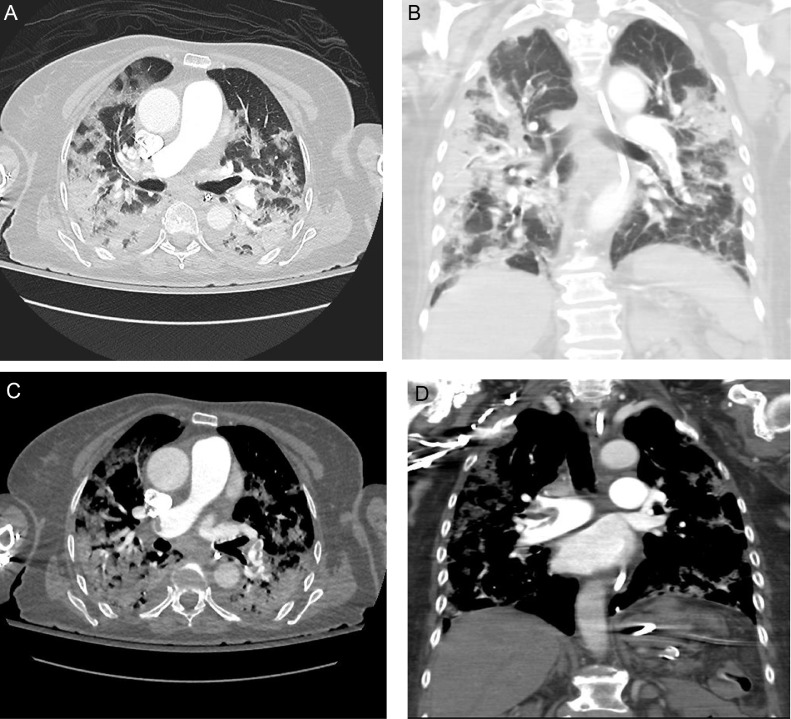
Code stroke work-up was initiated. Noncontrast head CT did not demonstrate hemorrhage. CT angiogram (CTA) of the head and neck demonstrated a partial right Sylvian segment (M2), superior division occlusion and right opercular (M3), parietal segment occlusions, respectively (Fig. 1). Bilateral, peripheral, upper lobe ground glass opacities were also found in the lung apices in the CTA of the neck suggesting a severe viral pneumonia (Fig. 2A). CT perfusion revealed a large area of penumbra involving the right MCA(middle cerebral artery) territory with a comparatively tiny infarction (Fig. 3).
Fig. 1.
(A) Axial MIP CTA of the head demonstrates a cutoff of the right M2 superior division (yellow arrow). (B) Coronal MIP CTA of the head demonstrates a cut off of the right M2 superior division (yellow arrow) and parietal M3 branches (blue arrow).
Fig. 2.
(A,B) Axial contrast-enhanced CTA of the neck (A, lung window; B, soft tissue window) demonstrates diffuse bilateral peripheral ground-glass opacities and consolidations compatible with COVID-19 pneumonia. A filling defect in a left upper lobe segmental artery is compatible with a left upper lobe segmental pulmonary emboli (yellow arrow).
Fig. 3.
CT perfusion demonstrates a large, mapped area of penumbra (green) in the right MCA territory and comparatively tiny infarction (red).
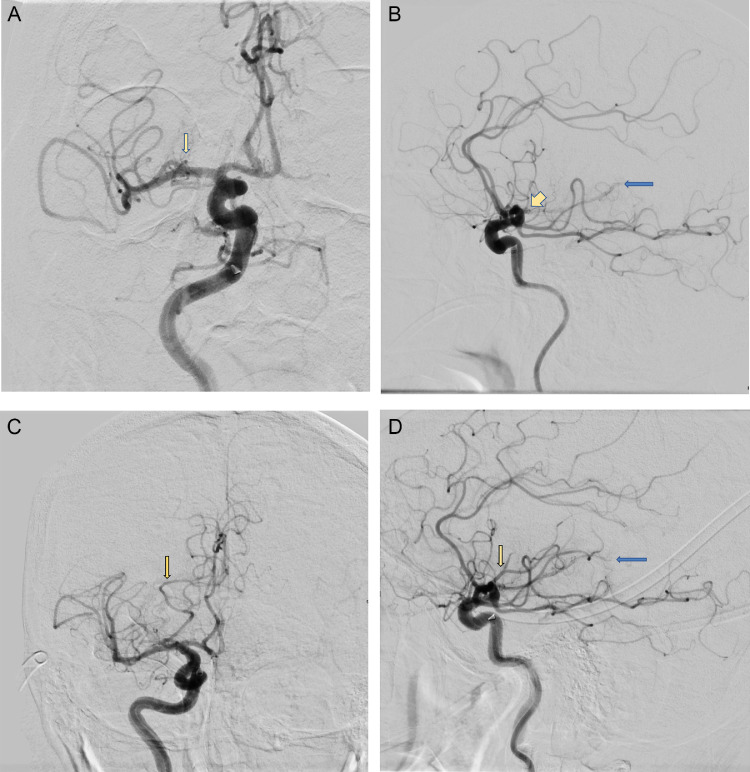
Intravenous tissue plasminogen activator (tPA) was withheld, as the patient was outside of the tPA window. She was sent to the interventional radiology (IR) suite for thrombectomy. After 4 passes, partial recanalization of an occluded superior M2 branch was obtained, with no significant change in patients NIHSS score of 20-21 (Fig. 4).
Fig. 4.
(A) Frontal digital subtraction angiography (DSA) demonstrates cutoff of the superior division M2 branches (yellow arrow). (B) Lateral DSA demonstrates decreased flow of the right M3 branches feeding the parietal lobe (blue arrow) and distal M2 branches feeding the frontal lobe (yellow arrow). (C) Frontal DSA post-treatment demonstrates partially recanalized flow in the superior division, right M2 branch (yellow arrow) that feeds the posterior frontal and opercular frontal lobe. (D) Lateral DSA post-treatment demonstrates flow in superior M2 branch (yellow arrow) that feeds the posterior frontal and opercular frontal lobe. The parietal branch M3 occlusion persists (blue arrow).
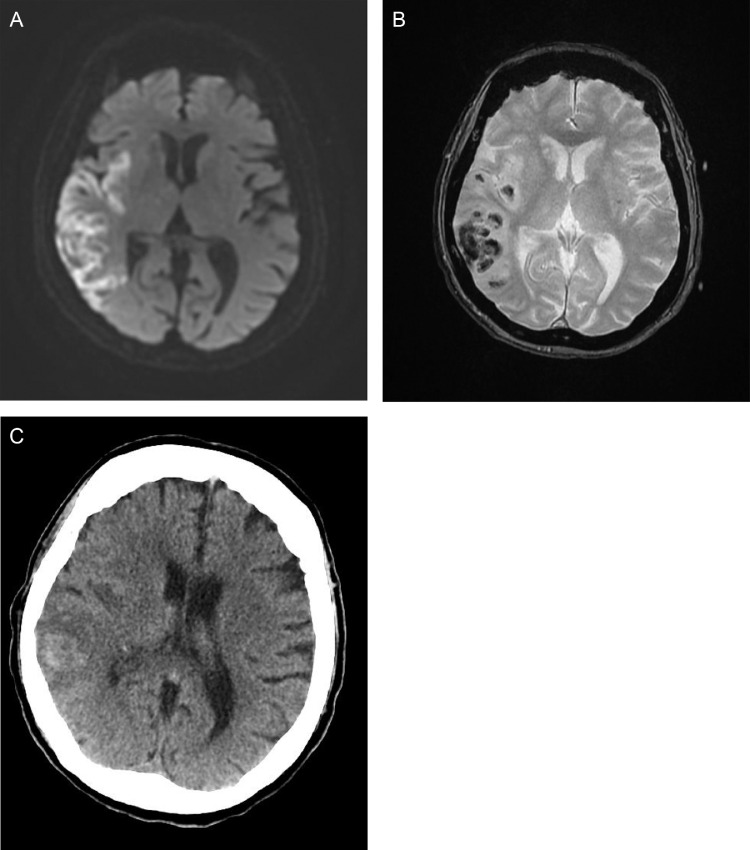
A follow-up brain magnetic resonance imaging (MRI) and head CT showed multiple, discrete, peripheral acute infarctions of the right MCA territory with some hemorrhagic conversion (Fig. 6).
Fig. 6.
(A) Axial DWI demonstrates restricted diffusion involving the right MCA territory. (B) Axial GRE demonstrates susceptibility artifact in the region of right MCA stroke, compatible with hemorrhage. (C) Axial head CT demonstrates right MCA subacute infarction with effacement of involved cerebral sulci, edema, and hemorrhage in the parietal lobe and insular cortex.
The patient continued to require high flow oxygen with D-dimer of 8.24 units and C-reactive protein of 50 mg/L. Given the patient's declining oxygen saturation, a chest radiograph was obtained and demonstrated bilateral peripheral opacities (Fig. 5). A positive nasopharyngeal swab Polymerase chain reaction test confirmed suspicion for COVID-19.
Fig. 5.
AP chest radiograph demonstrates multiple bilateral peripheral consolidations.
At this time, the upper chest on the initial CTA of the neck was re-reviewed with the added finding of a single segmental thrombus within a left upper lobe pulmonary artery (Fig. 2B). A lower extremity venous ultrasound was performed with no deep vein thrombosis identified.
A subsequent CTA of the pulmonary arteries revealed diffuse ground-glass opacities and bibasilar consolidations compatible with severe COVID-19 pneumonia with high burden bilateral acute pulmonary emboli (Fig. 7). Pulmonary emboli involved the right main pulmonary artery, right lung lobar arteries and bilateral segmental arteries. No radiological signs for right heart strain were identified.
Fig. 7.
Axial and coronal CT chest angiogram images (lung and angiogram windows) demonstrate filling defects in the right main pulmonary artery and left lobar artery. Bilateral peripheral consolidations and ground glass areas are present.
During the admission, the patient continued to require oxygen supplementation and was treated with nonbolus intravenous Heparin drip and hydroxychloroquine. At the time of submission, the patient was hospitalized with stable respiratory symptoms and progressive neurologic improvement.
Discussion
This case illustrates why the COVID-19 pandemic leads to poor outcomes and thrombotic complications in some patients. This case demonstrates the presence of concomitant thromboembolic events in the cerebral arterial system and pulmonary vasculature, in the absence of additional risk factors including atrial fibrillation, family history of hypercoagulability, and lower extremity deep vein thrombosis. These findings are supported by the current evidence that COVID-19 may predispose patients to increased thromboembolic disease [1], [2], [3], [4], [5]. Furthermore, patients may present with thromboembolic complications, such as stroke prior to respiratory symptoms.
COVID-19 has presented a number of diagnostic challenges, in particular those with neurologic and respiratory findings. Our patient was admitted with the diagnosis of stroke and the concomitant decreased oxygen saturation that was initially attributed to COVID-19 pneumonia. The suspicion for pulmonary embolism occurred later in the inpatient hospital course, resulting in re-reviewing the initial neck CTA to diagnose the initial pulmonary embolism and triggered a subsequent CT pulmonary angiogram that showed high burden pulmonary emboli.
This case also highlights that treating physicians should have a low threshold for diagnostic head and neck CTA and CT pulmonary angiogram in COVID-19 patients with respiratory deterioration and neurologic findings. Early recognition and treatment of thromboembolic disease may lead to improved patient morbidity and mortality. This case supports the growing body of data that hypercoagulability is a major contributor to COVID-19-related complications and may serve to alert the medical community to heightened vigilance for thromboembolic complications in COVID-19 positive patients. Thromboembolic disease may even be the initial presentation of the disease. COVID-19 has been shown in preliminary analysis to be an independent risk factor for stroke and possibly large vessel occlusion [6]. Larger cohorts of patients of COVID-19 need to be studied to assess the risk of acute thromboembolic disease, of all types, as an independent risk factor.
References
- 1.Oudkerk M, Oudkerk M, Buller H, Kuijpers D, Van Es N, Oudkerk S, McLoud T, Gommers D. Diagnosis, prevention, and treatment of thromboembolic complications in COVID-19: report of the National Institute for Public Health of the Netherlands. Radiology. 2020;23 doi: 10.1148/radiol.202020169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok FA, Kruip M, Van Der Meer J, Arbous M, Gommers D, Kant K. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oxley T, Mocco J, Majidi S, Kellner C, Shoirah H, Singh I. Large-vessel stroke as a presenting feature of COVID-19 in the young. N Engl J Med. 2020 doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bikdeli B, Madhavan M, Jimenez D, Chuich T, Dreyfus I, Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. JACC. 2020 doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruggeman R, Gietema H, Jallah B, Ten Cate H, Stehouwer C, Spaetgens B. Arterial and venous thromboembolic disease in a patient with COVID-19: a case report. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kihira S, Schefflein J, Chung M, Mahmoudi K, Rigney B, Delman B, Mocco J, Doshi A, Belani P. Incidental COVID-19 related Lung Apical Findings on Stroke CTA during the COVID-19 Pandemic. JNIS. 2020 doi: 10.1136/neurintsurg-2020-016188. [DOI] [PubMed] [Google Scholar]