Abstract
Emergency departments are facing an unprecedented challenge in dealing with patients who have coronavirus disease 2019 (COVID-19). The massive number of cases evolving to respiratory failure are leading to a rapid depletion of medical resources such as respiratory support equipment, which is more critical in low- and middle-income countries. In this context, any therapeutic and oxygenation support strategy that conserves medical resources should be welcomed. Prone positioning is a well-known ventilatory support strategy to improve oxygenation levels. Self-proning can be used in the management of selected patients with COVID-19 pneumonia. Here, we describe our experience with two COVID-19-positive patients who were admitted with respiratory failure. The patients were successfully managed with self-proning and noninvasive oxygenation without the need for intubation.
Keywords: Acute respiratory distress syndrome, Prone positioning, Noninvasive ventilation, Coronavirus, COVID-19, Pulmonary ventilation
1. Introduction
The surge of the COVID-19 pandemic is putting a huge amount of stress on medical facilities around the world. The massive number of cases admitted to emergency departments and the rapid evolution to respiratory failure have quickly depleted critical care resources, especially respiratory support equipment, such as ventilators, and intensive care unit (ICU) beds. In this context, any therapeutic and oxygenation support strategy that conserves medical resources should be welcomed. Prone positioning is a well-known ventilatory support strategy to improve oxygenation levels, typically applied in mechanically ventilated patients with acute respiratory distress syndrome (ARDS). The proposed mechanism by which this strategy works involves reducing ventilation/perfusion (V/Q) mismatch and making lung perfusion more uniform [1,2]. Here, we describe our experience with two COVID-19 patients who presented to the emergency department with respiratory failure and were admitted to the ICU. Both cases were successfully managed with self-proning and noninvasive oxygenation, without the need for intubation.
2. Case 1
A 43-year-old man presented to the emergency department with an 8-day history of myalgia, unmeasured fever, and a productive cough, having evolved to diarrhea, hyporexia, and anosmia. He tested positive for infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A computed tomography scan showed pulmonary opacities, with peripheral, multifocal, ground-glass attenuation, involving 25–50% of the pulmonary parenchyma in both lungs, together with consolidation in both lower lobes (Fig. 1). Because he had tachypnea and tachycardia, he was admitted to the ICU and started on oxygen, applied through a nonrebreather face mask at 10 L/min. Nonetheless, he continued to complain of dyspnea and was tachypneic, with a respiratory rate of 30 breaths/min, despite 100% peripheral oxygen saturation (SpO2) having been achieved. He was then instructed to switch to the prone position for as long as he could. The proning time was approximately 10 hours and resulted in significant improvement of the symptoms and a progressive reduction in his need for oxygen—from 10 L/min to 5 L/min—together with improvement of his tachypnea and tachycardia. He was discharged from the ICU after 24 hours (on day 9 after symptom onset).
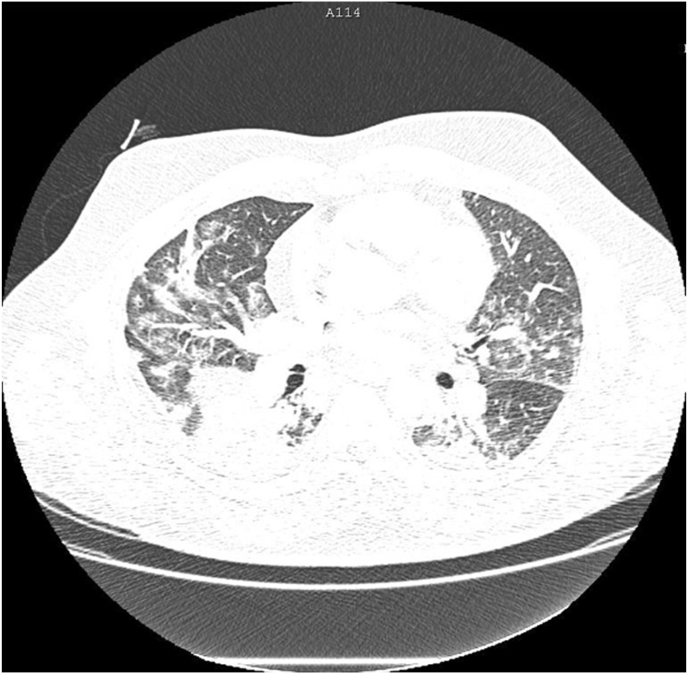
Fig. 1.
Computed tomography scan showing pulmonary opacities with peripheral, multifocal ground-glass attenuation in both lungs, involving 25–50% of the pulmonary parenchyma, accompanied by consolidation in both lower lobes.
3. Case 2
A 37-year-old man was transferred to our hospital and admitted to the emergency department with diagnosis of COVID-19 and a 7-day history of a productive cough, myalgia, and fever. A computed tomography scan showed pulmonary opacities with peripheral, multifocal and bilateral ground-glass attenuation associated with small areas of consolidation involving approximately 50% of the pulmonary parenchyma (Fig. 2). On admission, he was tachypneic and tachycardic and oxygen was applied through a nonrebreather face mask at 10 L/min. He continued to complain of dyspnea, he had a respiratory rate of 28 breaths/min, and his SpO2 was 94%. He was then instructed to switch to the prone position for as long as he could. After approximately 8 hours spent predominantly in the prone position, there was a significant improvement of the symptoms, as well as reductions in the respiratory rate and heart rate (Table 1). There was also an improvement in the arterial oxygen tension/fraction of inspired oxygen (PaO2/FiO2) ratio, together with a reduction in the level of oxygen support needed (Table 2). Over the next two days, the patient continued to receive oxygen via a nasal cannula. However, he no longer complained of dyspnea and there was progressive improvement of his clinical condition.
Fig. 2.
Computed tomography scan showing pulmonary opacities with peripheral, multifocal ground-glass attenuation, together with small areas of consolidation involving approximately 50% of the pulmonary parenchyma, in both lungs.
Table 1.
Clinical (emergency department) data related to case 2.
| Variable | 4 May, 2020 |
|
|---|---|---|
| 08:00 | 18:00 | |
| Respiratory rate (breaths/min) | 28 | 22 |
| Heart rate (bpm) | 100 | 85 |
| Peripheral oxygen saturation (%) | 94 | 96 |
| Oxygen via a nonrebreather face mask (L/min) | 10 | – |
| Oxygen via a nasal cannula (L/min) | – | 3 |
Table 2.
Biochemical data related to case 2.
| Variable | 4 May, 2020 |
|
|---|---|---|
| 08:27 | 17:58 | |
| pH | 7.51 | 7.48 |
| pO2 | 41.7 | 50 |
| pCo2 | 31.2 | 35.2 |
| Bicarbonate | 26.5 | 26.9 |
| Base excess | 1.9 | 2.6 |
| SaO2 | 83.6 | 89.3 |
| SpO2 | 83 | 89 |
| Oxygen support | Room air | Room air |
| Lactic acid | 11 | 12 |
| PaO2/FiO2 | 198 | 238 |
pO2, oxygen tension; pCo2, carbon dioxide tension; SaO2, arterial oxygen saturation; SpO2, peripheral oxygen saturation; PaO2/FiO2, arterial oxygen tension/fraction of inspired oxygen.
4. Discussion
Emergency physicians around the world are facing an unprecedented challenge in dealing with COVID-19 patients. The massive number of patients with respiratory failure admitted to the emergency wards have rapidly depleted medical resources, which are more critical in low- and middle-income countries. As an additional pressure on hospital stockpiles, concerns related to the risks involving aerosol generation that could potentially increase virus dispersion, have precluded the use of noninvasive ventilatory strategies and have promoted earlier intubation [3]. In this setting, any respiratory support strategy that can conserve critical medical resources should be carefully evaluated.
Prone positioning has long been known to be a useful maneuver to improve oxygenation and lung recruitment during invasive mechanical ventilation in patients with ARDS [1,2]. Placing the patient in the prone position results in more uniform alveolar architecture and perfusion, thus reducing regional V/Q mismatch and improving oxygenation. The consequent improvement in oxygenation leads to further improvement of the V/Q mismatch and is associated with reduced mortality [1,2]. In one previous study, this strategy was successfully applied in 20 awake, non-intubated patients with moderate to severe ARDS [4]. In that study, early prone positioning combined with high-flow nasal cannula oxygen therapy/noninvasive ventilation (HFNC/NIV) avoided the need for intubation in more than half of the patients, and the PaO2/FiO2 increased by 25–35 mmHg in those patients [4].
To our knowledge, there have been only two case reports and one case series in which prone positioning was applied in awake, non-intubated patients with COVID-19 [[5], [6], [7]], In the case series [7], fifty such patients were evaluated and the median peripheral oxygen saturation (SpO2) increased from 80% while breathing room air to 84% after application of supplemental oxygen. After 5 minutes of proning, the median SpO2 improved significantly (to 94%). In 13 patients (26%), the SpO2 failed to improve and endotracheal intubation was required within 24 hours after their arrival in the emergency department.
Our two patients also presented good outcomes. Both reported relief from their respiratory symptoms and presented an improvement in their PaO2/FiO2 that allowed the amount of oxygen supplied to be reduced. In the patient described in case 2, however, the improvement in PaO2 seen in the blood gas analysis after prone positioning was paradoxically accompanied by a slight worsening of the arterial carbon dioxide tension (PaCO2) The expected change in PaCO2 during prone positioning may be variable. The behavior of the PaCO2 depends mainly on that of the alveolar ventilation and its relationship with the total ventilated lung volume [1]. We believe that the improvement in the PaO2 promoted the decrease in the respiratory rate, which was the ultimate determinant of the increase in the PaCO2 in this case.
Taken together, these reported experiences of prone positioning in awake, spontaneously breathing patients with COVID-19 indicate that this strategy is a potentially useful tool for improving oxygenation and relieving symptoms with minimal impact on the already overburdened health system. Proning is simple, reduces costs, and does not require additional personnel [7].
Concerns related to increased aerosol generation, mainly associated with HFNC/NIV, can be mitigated by cohorting patients, providing adequate personal protective equipment for staff, and placing surgical masks on the patients [5].
Finally, well-designed, prospective randomized controlled trials are warranted in order to define which COVID-19 patients would benefit most from this strategy. The benefits of proning a conscious spontaneously breathing patient, thus avoiding mechanical ventilation, should be weighed against the risks of postponing an inevitable intubation. Choosing the right patients could improve survival by avoiding unnecessary intubation, as well as conserving valuable medical resources in these critical times.
Funding
There was no funding for the present paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101096.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gattinoni L., Quintel M., Busana M., Giosa L., Macrì M.M. Prone positioning in acute respiratory distress syndrome. Semin. Respir. Crit. Care Med. 2019;40:94–100. doi: 10.1055/s-0039-1685180. [DOI] [PubMed] [Google Scholar]
- 2.Kallet R.H., Faarc R.R.T. A comprehensive review of prone position in ARDS. Respir. Care. 2015:1660–1687. doi: 10.4187/respcare.04271. di. [DOI] [PubMed] [Google Scholar]
- 3.Ñamendys-Silva Silvio A. Correspondence Respiratory support for patients with COVID-19. Lancet Respir Med. 2020;8 doi: 10.1016/S2213-2600(20)30110-7. (April):2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ding L., Wang L., Ma W., He H. vols. 1–8. 2020. (Efficacy and Safety of Early Prone Positioning Combined with HFNC or NIV in Moderate to Severe ARDS : a Multi-Center Prospective Cohort Study). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slessarev M., Cheng J., Ondrejicka M. Patient self-proning with high-flow nasal cannula improves oxygenation in COVID-19 pneumonia. Can J Anesth Can Anesth. 2020:19–21. doi: 10.1007/s12630-020-01661-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elkattawy S., Noori M. A case of improved oxygenation in SARS-CoV-2 positive patient on nasal cannula undergoing prone positioning. Respir Med Case Rep. 2020:101070. doi: 10.1016/j.rmcr.2020.101070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caputo N., Strayer R., Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED's experience during the COVID-19 pandemic. Acad. Emerg. Med. 2020 doi: 10.1111/acem.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.