Leung et al. [1] have recently published, in the European Respiratory Journal, a paper on the expression of angiotensin-converting enzyme II (ACE-2) in the small airway epithelia of smokers and COPD patients, discussing its effects on the risk of severe coronavirus disease 2019 (COVID-19). The authors found an increased expression of the ACE-2 gene in the airways of subjects with COPD and in current smokers. Indeed, a recent systematic review reporting data on the smoking habits of patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), concluded that smoking may be associated with a negative progression of the disease and with the adverse outcome [2].
Short abstract
Nicotine via alpha7-nicotinic receptor induces ACE-2 overexpression in human bronchial epithelial cells (HBEpC) https://bit.ly/3eJ5b35
To the Editor:
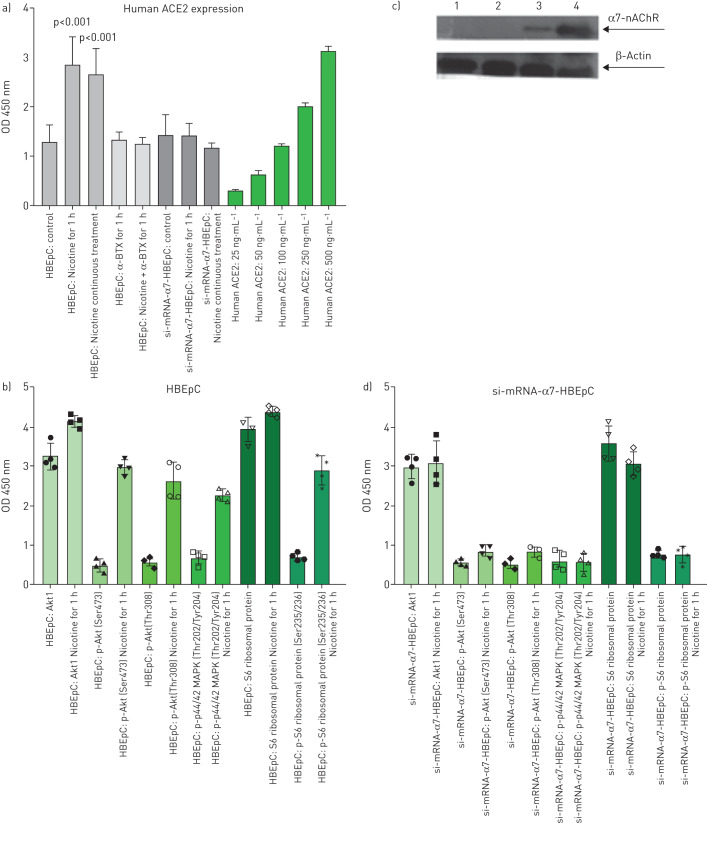
Leung et al. [1] have recently published, in the European Respiratory Journal, a paper on the expression of angiotensin-converting enzyme II (ACE-2) in the small airway epithelia of smokers and COPD patients, discussing its effects on the risk of severe coronavirus disease 2019 (COVID-19). The authors found an increased expression of the ACE-2 gene in the airways of subjects with COPD and in current smokers. Indeed, a recent systematic review reporting data on the smoking habits of patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), concluded that smoking may be associated with a negative progression of the disease and with the adverse outcome [2]. These conclusions were challenged in a correspondence by Cai [3] on the basis that a reliable mechanism explaining this association was missing. The need for these results to be supported by additional studies is quite clear, but we believe that a robust mechanistic explanation exists. Nicotine has a known influence on the homeostasis of the renin–angiotensin system (RAS) up-regulating the angiotensin-converting enzyme (ACE)/angiotensin (ANG)-II/ANG II type 1 receptor axis, and down-regulating the compensatory ACE-2/ANG-(1–7)/Mas receptor axis, contributing in turn to the development of cardiovascular and pulmonary diseases [4]. Different airway cells, such as bronchial epithelial cells, type II alveolar epithelial cells and interstitial lung fibroblasts, express nicotinic acetylcholine receptors (nAChR), specifically the α7subtype [5]. All these cells express components of the RAS [4]. In addition, nicotine increases the expression and/or activity of ACE in the lung [4], an increase which has been found also in the serum of smokers, and that required at least 20 min to return to control level [4]. ACE-2 serves as a physiologically relevant cellular entry receptor for SARS-CoV, for the human respiratory coronavirus NL63, and probably for SARS-CoV-2 [6]. ACE binds the SARS-CoV-2 S protein, and through its tissutal expression mediates the localisation and the efficiency of the infection [6]. Moreover, nicotine induces the epithelial–mesenchymal transition (EMT) [5, 7], a mechanism sufficient to allow “normal” differentiated cells to acquire the stem cell-like characteristics and properties. We planned experiments on human bronchial epithelial cells (HBEpC), obtained from Cell Applications Inc. (www.cellapplications.com/product number 502K-05a). Cells were maintained as adherent monolayer in complete bronchial/tracheal epithelial cell growth medium (www.cellapplications.com/product) at 37°C in 95% air/5% CO2, seeded at an initial density of 7.5×104 cells·cm−2, and sub-cultured with a 0.25% trypsin–1 mM EDTA solution (Sigma-Aldrich, Milan, Italy) when cultures reached 80% confluence. HBEpC are derived from the surface epithelium of normal human bronchi non-diseased (i.e. asthma, COPD or type 2 diabetes). The morphology is consistent with epithelial origin, and is positive for epithelial cell marker cytokeratin 18. Semi-confluent HBEpC at fourth passage (7.5×104 cells·cm−2) were treated: 1) for 1 h with zero or 1.0×10−7 M nicotine (Sigma-Aldrich, Milan, Italy) dissolved in saline in complete medium; 2) with 1.0×10−6 M α-Bungarotoxin (α-BTX; Sigma-Aldrich, Milan, Italy) dissolved in saline, in the continued presence of nicotine at zero or 1.0×10−7 M for 1 h; 3) treated continuously with nicotine for additional passages, 1 passage every 48 h for a total of 16 passages. We showed, for the first time, that nicotine at 1×10−7 M (the concentration present on the alveolar lining fluids after one cigarette is in the range 6×10−6 to 6×10−5 M [5]) is able to increase ACE-2 (figure 1a) in HBEpC. Treatment with nicotine induces phospho-S6 ribosomal protein (Ser235/236), Akt1, phospho-Akt (Ser473), phospho-Akt (Thr308) and phospho-p44/42 MAPK (Thr202/Tyr204) (figure 1b). To verify the hypothesis that ACE-2 is induced by nicotine through α7-nAChR, HBEpC, at fourth passage, in the exponential growth phase, plated at a density of 1×106 cells·mL−1, were incubated with α7-nAChR siRNA (0.1 μg) diluted in 100 μL of siRNA transfection medium. Transfection was performed as described by Li et al. [8], who transfected, successfully, HBE16 human airway epithelial cell line (unaffected cells). A clone of transfected HBEpC that did not express α7-nAChR proteins, also after treatment with nicotine (figure 1c), and is not able to induce phospho-S6 ribosomal protein (Ser235/236), Akt1, phospho-Akt (Ser473), phospho-Akt (Thr308) and phospho-p44/42 MAPK (Thr202/Tyr204) after nicotine treatment (figure 1d), was selected for further experiments. Nicotine did not induce ACE-2 in this clone (si-mRNA-α7-HBEpC) (figure 1a). This observation supports the hypothesis that ACE-2 increase is specifically mediated by α7-nAChR. Moreover, when HBEpC were incubated simultaneously with nicotine and α-BTX, an α7 nicotine antagonist [9], no induction of ACE-2 was observed (figure 1d). Importantly, treatment with nicotine, α-BTX or with the combination is not cytotoxic (data not shown). On these bases, we suggest that smoking may promote cellular uptake mechanisms of SARS-CoV-2 through α7-nAChR signalling. A possible α7-nAChR down-stream mechanism may be the induction of phospho-Akt and phospho-p44/42 MAPK. This mechanism was hypothesised, partially, by Olds and Kabbani [10] on their schematic model explaining how nicotine exposure increases the risk of SARS-CoV-2 entry into lung cells. α7-nAChR is present both in neuronal and non-neuronal cells (i.e. lung, endothelial, lymphocyte); consequently, smoking may impact COVID-19 pathophysiology and clinical outcome in several organ systems, including the brain.
FIGURE 1.
Effect of nicotine on human bronchial epithelial cells (HBEpC) or si-mRNA-α7-HBEpC. a) Angiotensin-converting enzyme II (ACE-2) detection. ACE-2 was measured with human ACE-2 ELISA kit ab235649 (www.abcam.com/human-ace2-elisa-kit-ab235649.html) according to the manufacturer's instructions. Data are mean±sem; p-vaule was evaluated using t-test. The green plots are the human ACE-2 standard. Experiments were performed twice in triplicate. b) Induction of phospho-S6 ribosomal protein (Ser235/236), Akt1, phospho-Akt (Ser473), phospho-Akt (Thr308) and phospho-p44/42 MAPK (Thr202/Tyr204) in HBEpC. Data were obtained using PathScan® cell growth Multi-target Sandwich ELISA kit n.7239 (Cell Signaling) PathScan® Cell Growth Multi-Target Sandwich ELISA Kit is a solid phase sandwich ELISA that combines the reagents necessary to detect endogenous levels of S6 ribosomal protein, phospho-S6 ribosomal protein (Ser235/236), Akt1, phospho-Akt (Ser473), phospho-Akt (Thr308) and phospho-p44/42 MAPK (Thr202/Tyr204). Data are mean±sem; p-value was evaluated using t-test. Experiments were performed twice in duplicate. c) α7-nAChR protein detection. Western blotting was performed as described previously [11]. Human α7-nAchR antibody NBP1-49348 was purchased from Novus Biologicals (www.novusbio.com). 1–2 si-mRNA-α7-HBEpC treated with zero (lane 1) or 1.0×10−7 M nicotine (lane 2) for 1 h. 3–4 HBEpC treated with zero (lane 3) or 1.0×10−7 M nicotine (lane 4) for 1 h. Experiments were performed twice. d) as in panel b, but treated cells are si-mRNA-α7-HBEpC.
Shareable PDF
Supplementary Material
Footnotes
Conflict of interest: P. Russo has nothing to disclose.
Conflict of interest: S. Bonassi has nothing to disclose.
Conflict of interest: R. Giacconi has nothing to disclose.
Conflict of interest: M. Malavolta has nothing to disclose.
Conflict of interest: C. Tomino has nothing to disclose.
Conflict of interest: F. Maggi has nothing to disclose.
References
- 1.Leung JM, Yang CX, Tam A, et al. ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J 2020; 55: 2000688. doi: 10.1183/13993003.00688-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis 2020; 18: 20. doi: 10.18332/tid/119324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir Med 2020; 8: e20. doi: 10.1016/S2213-2600(20)30117-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oakes JM, Fuchs RM, Gardner JD, et al. Nicotine and the renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol 2020; 315: R895–R906. doi: 10.1152/ajpregu.00099.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cardinale A, Nastrucci C, Cesario A, et al. Nicotine: specific role in angiogenesis, proliferation and apoptosis. Crit Rev Toxicol 2012; 42: 68–89. doi: 10.3109/10408444.2011.623150 [DOI] [PubMed] [Google Scholar]
- 6.Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020; 579: 270–273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santoro A, Tomino C, Prinzi G, et al. Tobacco smoking: risk to develop addiction, chronic obstructive pulmonary disease, and lung cancer. Recent Pat Anticancer Drug Discov 2019; 14: 39–52. doi: 10.2174/1574892814666190102122848 [DOI] [PubMed] [Google Scholar]
- 8.Li Q, Zhou X, Kolosov VP, et al. The expression and pharmacological characterization of nicotinic acetylcholine receptor subunits in HBE16 airway epithelial cells. Cell Biochem Biophys 2012; 62: 421–431. doi: 10.1007/s12013-011-9324-z [DOI] [PubMed] [Google Scholar]
- 9.Wang YY, Liu Y, Ni XY, et al. Nicotine promotes cell proliferation and induces resistance to cisplatin by α7 nicotinic acetylcholine receptor-mediated activation in Raw264.7 and El4 cells. Oncol Rep 2014; 31: 1480–1488. doi: 10.3892/or.2013.2962 [DOI] [PubMed] [Google Scholar]
- 10.Olds JL, Kabbani N. Is nicotine exposure linked to cardiopulmonary vulnerability to COVID-19 in the general population? FEBS J 2020; in press [https://doi.org/10.1111/febs.15303]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trombino S, Cesaro A, Margaritora S, et al. Alpha7-nicotinic acetylcholine receptors affect growth regulation of human mesothelioma cells: role of mitogen-activated protein kinase pathway. Cancer Res 2004; 64: 135–145. doi: 10.1158/0008-5472.CAN-03-1672 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-01116-2020.Shareable (333.8KB, pdf)