COVID-19, the disease associated with SARS-CoV-2 infection, is in some 20% of acutely affected patients associated with respiratory distress syndrome (ARDS) often necessitating respirator treatment and associated with a high mortality [1–3]. Epidemics in Wuhan in China and Lombardy in Italy have been devastating, and SARS-CoV-2 has developed into a pandemic necessitating urgent worldwide co-operation. Until effective treatment of COVID-19 including a useful vaccination against SARS-CoV-2 is found, it is important to seek ways of limiting or avoiding ARDS. Virus-related ARDS is initiated from a high level of angiotensin II (Ang-II) via the type 1 receptor pathway [4], and Ang-II has already been demonstrated to be high in COVID-19 and linearly associated with lung injury [5]. Inhibitors of the renin–angiotensin system (RASi), cornerstones of treatment of patients with hypertension and heart failure, have attracted attention as they may in theory influence the Ang-II level in COVID-19 and thereby the risk of ARDS [4,6]. In short, Ang-II activity is influenced by the balance of Ang-converting enzyme (ACE) and ACE2 receptor activity. The activity of ACE2 normally lowers the level of Ang-II, but SARS-CoV-2 virus binds to ACE2 receptors, lower their activity and hence increase Ang-II activity [1]. While RASi lower Ang-II levels, and may in this respect be helpful, chronic RASi treatment may on the other hand also increase pulmonary ACE2-receptor numbers hence providing a possible higher SARS-CoV-2 viral load. As suggested from animal experiments, chronic treatment with RASi can therefore, in theory, both increase and lower the risk of ARDS in SARS-CoV-2-infected patients. Studies early listed heart disease, hypertension, and diabetes as risk factors for ARDS [1–3], but unfortunately medication has not yet been reported on, and clinical data on the relative importance of RASi for outcome in COVID-19 are now urgently needed.
Approved by the Danish Patient Safety Authority and the Danish Data Protection Agency, we related medication to outcome in all SARS-CoV-2 PCR positive patients, who, between 1 March and 1 April 2020, had remained admitted with infection to hospital for at least 24 h in two of five Danish regions (2.6 million inhabitants). We looked at a composite outcome of ICU-admission or death and determined the relative risk of RASi in logistic regression models estimating odds ratios of ICU-admission adjusted for time to event or censoring.
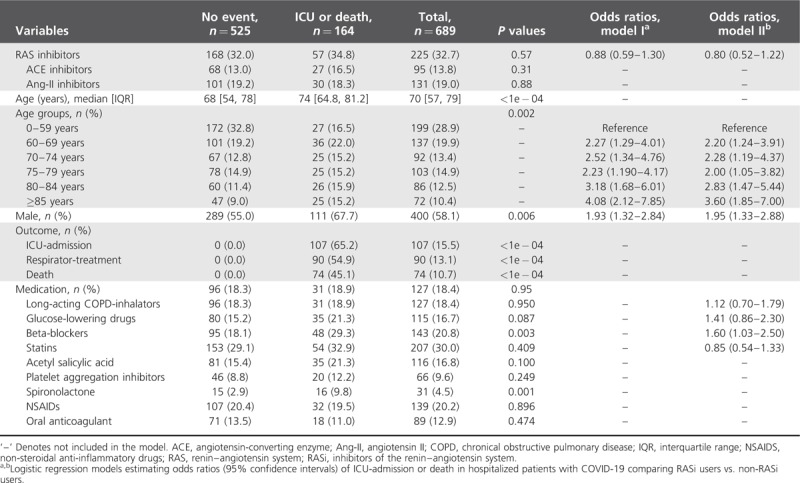
Out of a total of 2700 PCR positive patients, 689 patients (25.5%) were acutely ill and remained hospitalized for at least 24 h. Of these 689 patients 71.1% were 60 years or older; 58.1% were male; and 32.7% were treated with RASi. Out of 689 patients 525 did not experience an outcome, whereas 164 (23.8%) experienced ICU and/or death (Table 1). Eighty-four percent of the patients admitted to ICU needed respirator treatment. Mean risk time from having been admitted for 1 day till ICU was only 2.04 further days (SD 2.29; range 0–10). Medical treatment for chronic obstructive pulmonary disease, statins, antithrombotic drugs, and RASi were equally prevalent among outcome groups, while beta-blockers and spironolactone seem unevenly distributed with higher prevalence among patients, who were admitted to the ICU or died (Table 1). Glucose-lowering drugs tended to be unevenly distributed between groups (P = 0.087). In logistic regression analyses incorporating sex, age, risk-time, and selected medical treatment, we found that male sex, increasing age, and the use of beta-blockers independently increased odds for ICU-admission or death, but RASi treatment did not.
TABLE 1.
Characteristics of patients hospitalized for at least 24 h with PCR proven COVID-19, stratified by a composite outcome of admission to ICU or death
Current consensus [4,6] recommends not changing RASi treatment in patients with SARS-CoV-2 infection. Whereas we found other heart failure medication to be of importance, probably mainly reflecting the underlying cardiac phenotype and comorbidity, our data do not suggest any significant influence from chronic RASi treatment and hence our data bring some reassurance to the consensus of not changing RASi medication. Randomized studies on RASi treatment intervention in patients at risk of COVID-19 should consider timing the intervention early in the course of the disease or well before infection, since if patients do develop ARDS they do so after a very short time period.
ACKNOWLEDGEMENTS
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020; 323:1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Xiang J, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis 2020; 94:91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD. Renin–angiotensin–aldosterone system inhibitors in patients with COVID-19. N Engl J Med 2020; 382:1653–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCOV infected patients linked to viral loads and lung injury. Sci China Life Sci 2020; 63:364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Esler M, Esler D. Can angiotensin receptor-blocking drugs perhaps be harmful in the COVID-19 pandemic? J Hypertens 2020; 38:781–782. [DOI] [PubMed] [Google Scholar]


