Abstract
Although pneumonia caused by severe acute respiratory syndrome coronavirus 2 is a prominent feature of COVID-19, clinicians must consider whether treatment for additional potential causes of community-acquired pneumonia (CAP) is appropriate. The cochairs of the recently released American Thoracic Society and Infectious Diseases Society of America Guideline for Treatment of Adults with CAP offer their interpretation of this guideline's application to the evaluation and treatment of patients with COVID-19.
The rapidly escalating coronavirus disease 2019 (COVID-19) pandemic has focused attention on the diagnosis and treatment of patients with acute respiratory infection in an unprecedented manner. Although most of the lung injury patients have is believed to be caused by the virus, concern over bacterial co-infection also informs current treatment approaches for patients with COVID-19–related pneumonia. As the cochairs of the recently released American Thoracic Society and Infectious Diseases Society of America Guideline for Treatment of Adults with Community-Acquired Pneumonia (CAP) (1), we offer our interpretation of the guideline as it applies to the management of patients with COVID-19 (Table).
Table. Principles for Management of Pneumonia in Patients With COVID-19.
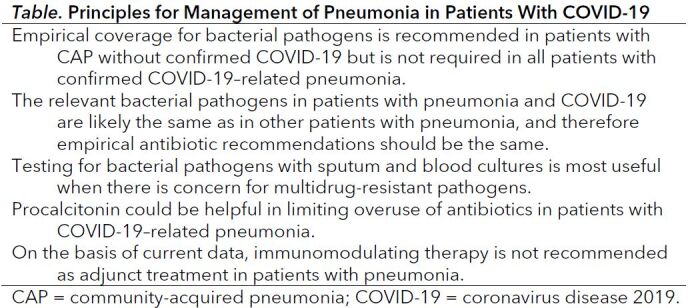
1. Empirical coverage for bacterial pathogens is recommended in patients with CAP without confirmed COVID-19 but is not required in all patients with confirmed COVID-19–related pneumonia.
Community-acquired pneumonia is diagnosed in patients with signs and symptoms of respiratory infection (especially cough, sputum production, and fever) and radiographic evidence of lung involvement. The cause of CAP includes a range of bacteria and viruses, and with the introduction of the pneumococcal conjugate vaccine, viruses are an increasingly frequent cause (2). Despite this trend, the new guideline continues to emphasize prompt antibacterial drug therapy for all patients diagnosed with CAP. Antibacterial therapy continues to be featured so prominently in CAP guidelines because before the COVID-19 pandemic, bacterial causes of CAP were associated with the highest mortality and empirical antibacterial therapy is proven to be effective and save lives.
Unfortunately, the classic microbiological diagnostic tests for CAP, sputum and blood cultures, fail to reveal a definitive pathogen in many cases (3), and although the identification of a specific pathogen can help narrow treatment decisions, the delay in obtaining a result leads to the need for initial empirical coverage, which is active against the common bacterial pathogens.
Recent studies have highlighted that findings of pulmonary involvement on chest imaging in patients with confirmed COVID-19 are common, including lobar consolidation, ground glass opacities, and reticular infiltrates (4). One series estimated that 59% of hospitalized patients have abnormalities on initial chest radiography, which is consistent with pneumonia, and 86% have abnormalities on chest computed tomography (5). A largely untested hypothesis is that most of these patients with radiographic abnormalities likely have isolated severe acute respiratory syndrome coronavirus 2 infection in the lung without any additional pathogen. However, a recent case series reported that serologic evidence of co-infection with bacterial pathogens (including chlamydia) was not uncommon among fatal cases of COVID-19 pneumonia (6).
2. Although data are limited, it is likely that the relevant bacterial pathogens in patients with COVID-19 and pneumonia are the same as in previous patients with CAP and therefore empirical antibiotic recommendations should be the same.
The bacterial pathogens responsible for CAP are reflective of the bacteria that often colonize the upper airway and opportunistically infect the lung during a respiratory illness. Therefore, we believe the same range of pathogens, including Streptococcus pneumoniae, Haemophilus influenzae, Chlamydia pneumoniae, and Staphylococcus aureus, should be considered in patients with COVID-19–related pneumonia. For low-risk inpatients (typically those on the general medical floors), the guideline recommends a β-lactam (for example, ampicillin–sulbactam, ceftriaxone, or cefotaxime) plus either a macrolide (azithromycin or clarithromycin) or doxycycline as combination therapies or a respiratory fluoroquinolone (levofloxacin or moxifloxacin) as monotherapy. For high-risk inpatients (typically those in the intensive care unit), the guideline recommends a β-lactam plus macrolide or β-lactam plus fluoroquinolone. We believe these same recommendations apply to patients with COVID-19.
3. Testing for bacterial pathogens with sputum and blood cultures is most useful when there is concern for multidrug-resistant pathogens.
An additional issue addressed by the CAP guideline was multidrug-resistant pathogens, specifically Pseudomonas aeruginosa and methicillin-resistant S aureus. In prior CAP guidelines, antibiotic coverage for these pathogens had been recommended in the presence of several risk factors associated with what was termed health care–associated pneumonia. In the current guideline, the focus is on a more limited set of risk factors, especially evidence that the patient was previously infected with either of these pathogens. Moreover, the guideline recommends that in all cases when more expanded antibiotic therapy is initiated, blood and sputum cultures should be obtained to confirm or rule out the presence of these pathogens. If results of cultures are negative and the patient is improving, the expanded therapy for P aeruginosa and methicillin-resistant S aureus should be narrowed within 48 hours of starting therapy.
4. Procalcitonin could be helpful in limiting overuse of antibiotics in patients with COVID-19–related pneumonia.
Before the COVID-19 pandemic, the inflammatory biomarker procalcitonin was shown to safely reduce antibiotic use in patients with CAP, but much of the effect was related to reducing the duration of therapy as opposed to withholding antibiotics altogether (7). Moreover, no procalcitonin threshold perfectly distinguishes viral from bacterial pneumonia (8). Procalcitonin may also be elevated in patients with COVID-19 because of generalized inflammatory activation rather than bacterial co-infection (9). Still, we endorse the use of a low procalcitonin value early in the course of confirmed COVID-19 illness to guide the withholding or early stopping of antibiotics, especially among patients with less severe disease. Perhaps more important, 5 days of antibiotic therapy is adequate for most patients with CAP.
5. Although it is likely that host immunologic processes play a key role in the lung damage that leads to respiratory failure and adverse outcomes in patients with COVID-19, immunomodulating therapy is not currently recommended in patients with pneumonia.
Before COVID-19, much attention was given to the potential benefits of adding corticosteroids to the treatment of adults with CAP. However, on the basis of a review of published studies (with an additional study since added [10]), the guideline committee ultimately recommended against using corticosteroids in patients with CAP. We do not currently recommend corticosteroids or other immunomodulating therapies as adjunct treatments for patients with COVID-19–related pneumonia.
Looking forward, it is clear there are many unanswered questions in the management of patients with COVID-19–related pneumonia. More detailed epidemiologic studies are needed to help guide the settings in which bacterial co-infection is more common and whether the involved pathogens are the same as those found in prior studies of CAP or if other pathogens, including multidrug-resistant pathogens, are more common. The role of biomarkers, including procalcitonin, should be similarly investigated in this regard. Ongoing trials will help clarify whether immunomodulating therapies are beneficial in patients with COVID-19–related pneumonia.
Biography
Disclosures: Authors have disclosed no conflicts of interest. Forms can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-2189.
Corresponding Author: Joshua P. Metlay, MD, PhD, Massachusetts General Hospital, 100 Cambridge Street, 16th Floor, Boston, MA 02114; e-mail, jmetlay@mgh.harvard.edu.
Current author addresses and author contributions are available at Annals.org.
Current Author Addresses: Dr. Metlay: Massachusetts General Hospital, 100 Cambridge Street, 16th Floor, Boston, MA 02114.
Dr. Waterer: Royal Perth Hospital and University of Western Australia, Level 3, Executive Corridor, Royal Perth, Perth, Australia.
Author Contributions: Conception and design: J.P. Metlay, G.W. Waterer.
Drafting of the article: J.P. Metlay, G.W. Waterer.
Critical revision of the article for important intellectual content: J.P. Metlay, G.W. Waterer.
Final approval of the article: J.P. Metlay, G.W. Waterer.
Collection and assembly of data: J.P. Metlay, G.W. Waterer.
Footnotes
This article was published at Annals.org on 7 May 2020.
References
- 1. doi: 10.1164/rccm.201908-1581ST. Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia: an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45-e67. [PMID: 31573350] doi:10.1164/rccm.201908-1581ST. [DOI] [PMC free article] [PubMed]
- 2. doi: 10.1056/NEJMoa1500245. Jain S, Self WH, Wunderink RG, et al; CDC EPIC Study Team. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373:415-27. [PMID: 26172429] doi:10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed]
- 3. doi: 10.1080/0036554021000026967. Lidman C, Burman LG, Lagergren A, et al. Limited value of routine microbiological diagnostics in patients hospitalized for community-acquired pneumonia. Scand J Infect Dis. 2002;34:873-9. [PMID: 12587618] [DOI] [PubMed]
- 4. doi: 10.1007/s00330-020-06801-0. Ye Z, Zhang Y, Wang Y, et al. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020. [PMID: 32193638] doi:10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed]
- 5. doi: 10.1056/NEJMoa2002032. Guan WJ, Ni ZY, Hu Y, et al; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [PMID: 32109013] doi:10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed]
- 6. doi: 10.1164/rccm.202003-0543OC. Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020. [PMID: 32242738] doi:10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed]
- 7. doi: 10.1164/rccm.200512-1922OC. Christ-Crain M, Stolz D, Bingisser R, et al. Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med. 2006;174:84-93. [PMID: 16603606] [DOI] [PubMed]
- 8. doi: 10.1093/cid/cix317. Self WH, Balk RA, Grijalva CG, et al. Procalcitonin as a marker of etiology in adults hospitalized with community-acquired pneumonia. Clin Infect Dis. 2017;65:183-190. [PMID: 28407054] doi:10.1093/cid/cix317. [DOI] [PMC free article] [PubMed]
- 9. doi: 10.1016/S0140-6736(20)30566-3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [PMID: 32171076] doi:10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed]
- 10. doi: 10.1001/jamainternmed.2019.1438. Lloyd M, Karahalios A, Janus E, et al; Improving Evidence-Based Treatment Gaps and Outcomes in Community-Acquired Pneumonia (IMPROVE-GAP) Implementation Team at Western Health. Effectiveness of a bundled intervention including adjunctive corticosteroids on outcomes of hospitalized patients with community-acquired pneumonia: a stepped-wedge randomized clinical trial. JAMA Intern Med. 2019; 179:1052-1060. [PMID: 31282921] doi:10.1001/jamainternmed.2019.1438. [DOI] [PMC free article] [PubMed]


