Abstract
Background
Our objective is to identify seasonal and weather trends associated with pediatric trauma admissions.
Methods
We reviewed all trauma activations leading to admission in patients ≤18 years admitted to a regional pediatric trauma center from January 1, 2000, to December 31, 2015. We reviewed climatologic measures of the mean temperature, mean visibility, and precipitation for each admission in the 6 h prior to each presentation in addition to time of arrival, weekday/weekend presentation, and season. We used a negative binomial regression model with multivariable analysis to estimate associations between weather and rate of trauma admissions. Results were presented as incidence rate ratios (IRR) with 95% confidence intervals (CI).
Results
In total, 3856 encounters [2539 males (65.8%), mean age 10.2 years ± SD 5.1 years] were included. Results from multivariable analysis (IRR, 95% CI) suggested an association of admissions with rain (0.82, 0.75–0.90) and overnight hours (23:51–05:50; 0.69, 0.58–0.82) as compared to morning (05:51–11:50). The IRR of trauma increased during the afternoon (11:51–17:50; 4.05, 3.57–4.61), night periods (17:51–23:50; 5.59, 4.94–6.33), and weekends (1.24, 1.15–1.32), and with every 1 °C increase in temperature (1.04, 1.03–1.04). After accounting for other variables, season was not found to be independently predictive of trauma admission.
Conclusion
Trauma admissions had a higher rate during afternoon, evening hours, and weekends. The presence of rain lowered the rate of pediatric trauma admission. Each degree increase in temperature increased the rate of trauma admissions by 4%. The findings provide information from the perspective of emergency preparedness, resource utilization, and staffing to pediatric trauma centers.
Introduction
Trauma is the leading cause of mortality in children over 1 year of age [1]. Data from the Healthcare Cost and Utilization Project in the USA suggest that injury and poisoning are the most common reason for visits to emergency departments (EDs) among children [2]. The management of pediatric trauma is a complex process with significant regional variation and requires coordination between emergency medical services, EDs, and trauma centers. In the USA, the cost of caring for pediatric trauma in 2012 was estimated to be $23 billion [3].
A growing body of evidence suggests seasonal and timing characteristics may be predictive of trauma events. Multiple investigators have evaluated the role of weather patterns in relation to trauma. Motor vehicle crashes (MVCs), for example, have been found to occur more frequently in the presence of rain and snow [4, 5]. In contrast, data from centers that primarily serve adults suggest that rain decreases the risk of trauma admission, whereas warmer weather increases it [6–8].
Little has been reported on the role of seasonal, timing, and weather changes in association with pediatric trauma. Previous investigators have identified that trauma events are likely to occur on warmer, sunnier days, and less likely to occur following rain [9–11]. However, these studies used daily averages for weather, such as daily maximum and minimum temperatures and the total daily rainfall, and were unable to identify weather patterns at the time of the traumatic event. Additionally, these investigations did not specifically exclude trauma presentations outside the immediate vicinity of the hospital or interfacility transports where weather patterns may have been different. Granular data with respect to pediatric trauma would be beneficial from the perspective of emergency preparedness, staffing, and resource management.
Using data from a dedicated regional pediatric trauma center and national weather archives, we aimed to identify seasonal and weather patterns associated with pediatric trauma admissions to a regional dedicated pediatric level 1 trauma center. We hypothesized that rainfall and frozen precipitation would be negatively associated with trauma and that admissions would occur more frequently at higher temperatures.
Methods
Study setting
We reviewed admissions at a pediatric level 1 trauma center in Allegheny County, Pennsylvania. Our institution is the only dedicated pediatric level 1 trauma center in this region, serving a catchment area of >2.6 million people, and cares for the majority of pediatric patients presenting with traumatic injuries. Allegheny County, located in Western Pennsylvania, is 1890 km2 in land area and has a population of 1,223,338, of which 18.8% are under 18 years per 2010 US Census data [12]. On average, over the course of a year, Allegheny County has 10 days below 0 degrees Celsius (°C) and 10 days above 32 °C, as well as 189 days with rain and 79 days with freezing precipitation [13]. Prior to data acquisition, institutional review board approval was obtained from the University of Pittsburgh.
Trauma data source and inclusion
Trauma admission electronic medical record data were acquired using Collector (Digital Innovations, Forest Hill, MD), the software product utilized by the State of Pennsylvania for trauma medical record chart abstraction. Elements for abstraction have been defined by the Pennsylvania Trauma Systems Foundation to ensure compliance with the American College of Surgeons standards for trauma care delivery. Trauma admissions from ED trauma activations for patients ages 18 and under were included between January 1, 2000, 00:51 and December 31, 2015, 23:51. We excluded admissions where the reported injury was outside the county of our hospital where weather may have been different. Additionally, patients who were admitted after an interfacility transport were excluded because the timing of transports is often delayed some time from the traumatic event. Patients with primary burn-related trauma were also excluded, as our hospital is not a burn center. Patient information collected from the database included demographics, date and time of trauma activation, mechanism of injury as defined by External-Cause-of-Injury Coding (E-Code), and admission information including fatality and duration of admission.
Weather data
Hourly weather data, including dry temperature (°C), visibility (statute miles), precipitation (inches), and weather events, were acquired from January 1, 2000, 00:51 to December 31, 2015, 23:51. Data were acquired from public records from the National Oceanic and Atmospheric Administration (NOAA) for Pittsburgh International Airport, located within Allegheny County, Pennsylvania (latitude 40.48, longitude – 80.21) [14]. We defined weather events for this study using Meteorological Terminal Aviation Routine Weather Report (METAR) codes as rain (drizzle, rain, and thunderstorm) or frozen precipitation (snow, ice crystals, hail, ice pellets, snow shower, snow pellets, and snow grains). Weather parameters from the reporting station were assessed every 51 min past the hour.
Data abstraction
Trauma events and weather characteristics were summarized by hour. Weather statistics were summarized from the preceding 6 h and calculated as (1) mean temperature, (2) mean visibility, (3) total precipitation (taken as a continuous variable), and (4) the presence of any weather event (rain or frozen precipitation), neither, or both, taken as a categorical variable. In addition to weather data, we also calculated timing data of each trauma event with respect to day of the week (weekday and weekend), season by meteorological definition (winter, December 1 to February 28; spring, March 1 to May 31; summer, June 1 to August 31; and fall, September 1 to November 30), and time into four windows (morning, 05:51 to 11:50, afternoon, 11:51 to 17:50; night 17:51 to 23:50, overnight, 23:51 to 05:50).
Data analysis
Our outcome of interest was the hourly rate of pediatric trauma admissions. We attempted to identify independent predictors of the outcome. Following methods used by other studies of trauma admission rates [10, 15], we used a negative binomial regression model to estimate associations between regional weather and rate of trauma center admissions, taking the number of trauma events as count data. After converting units from the NOAA dataset to SI units (visibility from statute miles to kilometers, inches of precipitation to centimeters), univariate analysis was done using a generalized linear model with a negative binomial distribution. Results with p < 0.05 were used in the development of a multivariable model. As weather-related factors were our primary area of interest, we started with temperature and precipitation in our model, adding other variables in a forward selection approach. Variables with p < 0.05 were kept in the multivariable model. Results for univariate and multivariable models are reported as incidence rate ratios (IRR) with 95% confidence intervals (CI). We additionally compared our findings to those of an alternative model using season, time of day, and day of week variables alone, without the incorporation of other weather characteristics. In order to identify if rates of different trauma types varied by month, we re-classified admissions into three groups of MVCs (E-Codes 810–825), falls (E-Codes 880–888), and all others and obtained the percentage of events in totality and in subgroups by months. Data management and analysis were performed using the tidyverse package in RStudio v.1.1.423 (Boston, Massachusetts) and IBM SPSS Statistics for Windows v25.0 (IBM Corporation, Armonk, New York).
Results
Description of trauma and weather events
From the original patient sample of 25,782 trauma events reviewed over the 16-year period, a total of 3856 events were included for study. Details regarding patients from these events are provided in Fig. 1. Mean patient age was 10.2 years (standard deviation 5.1) and 2539 (65.8%) events occurred in males (Table 1). The included weather period ranged from January 1, 2000, 00:51 to December 31, 2015, 23:51 and contained data for 139,407 data points. The included weather period contained data for 139,407 data points and summarized 140,257 h of observation. Trauma events month demonstrated a similar distribution by month when classified by subgroup (Fig. 2).
Fig. 1.
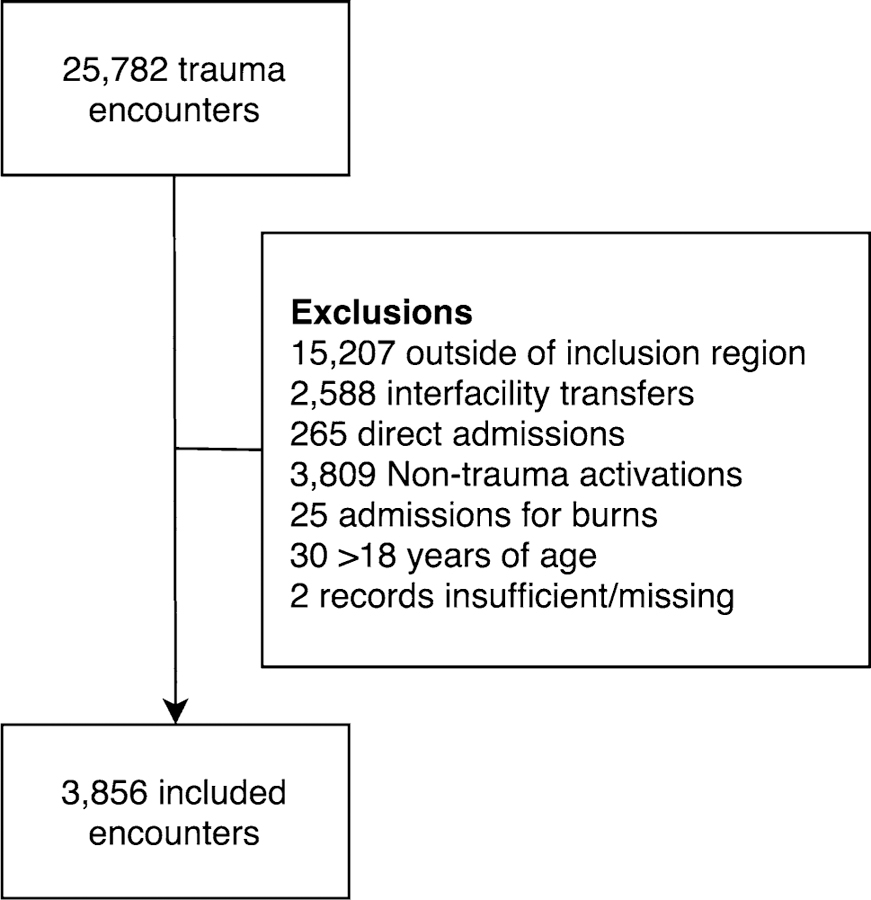
Study patient inclusion
Table 1.
Event descriptive data, mechanisms of trauma, and timing of events by time, day of week, and season
| Number of events | 3856 |
| Mean patient age (±SD) | 10.2 (5.1) |
| Events with males, n (%) | 2539 (65.8) |
| Race, n (%) | |
| White | 2384 (61.8) |
| Black | 1347 (34.9) |
| Other | 78 (2.0) |
| Not documented | 47 (1.2) |
| Admission parameters | |
| Median length of stay, days (IQR) | 1 (1–2) |
| Intensive care unit admissions, n (%) | 295 (7.7) |
| Transferred from ED to operating room, n (%) | 133 (3.4) |
| Outcome, n (%) | |
| Alive at discharge | 3801 (98.6) |
| Deceased | 55 (1.4) |
| Classification of trauma by External-Cause-of-Injury Coding, n (%) | |
| Motor vehicle traffic accidents | 1486 (38.5) |
| Motor vehicle non-traffic accidents | 151 (3.9) |
| Other road vehicle accidents | 307 (8.0) |
| Vehicle accidents not elsewhere classifiable | 34 (0.9) |
| Accidental falls | 1078 (28.0) |
| Accidents related to natural and environmental factors | 24 (0.6) |
| Submersion, suffocation, and foreign bodies | 80 (2.1) |
| Suicide and self-inflicted injury | 12 (0.3) |
| Homicide and injury purposely inflicted by other persons | 295 (7.7) |
| Other injuries | 389 (10.1) |
| Timing of event, n (%) | |
| Morning 05:51–11:50 | 291 (7.5) |
| Afternoon 11:51–17:50 | 1434 (37.2) |
| Night 17:51–23:50 | 1916 (48.7) |
| Overnight 23:51–05:50 | 215 (5.6) |
| Time of year, n (%) | |
| Winter (January 1–March 31) | 673 (17.5) |
| Spring (April 1–June 30) | 1141 (29.6) |
| Summer (July 1–September 30) | 1245 (32.3) |
| Fall (October 1–December 31) | 797 (20.7) |
| Day of week, n (%) | |
| Weekend | 1273 (33.0) |
| Weekday | 2583 (67.0) |
Fig. 2.
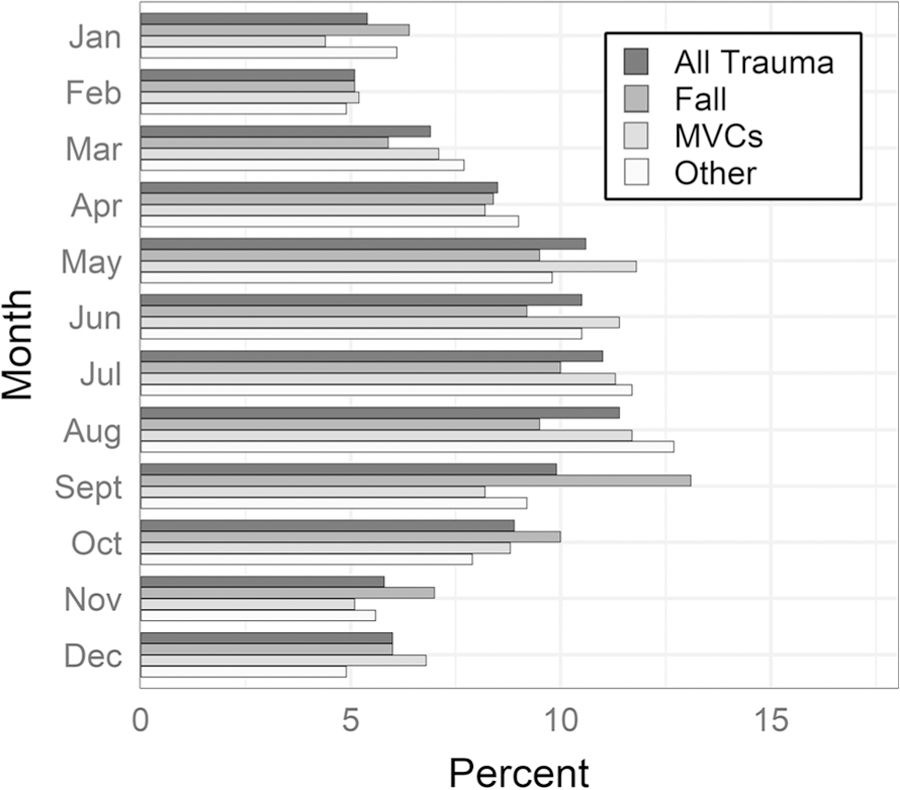
Percentages of trauma admissions by month, in totality (n = 3856) and by subgroups of motor vehicle collisions (MVC) (n = 1642), falls (n = 1092), and others (n = 1122)
Univariate analysis (Table 2)
Table 2.
Results from univariate and multivariable analysis
| Variable | Univariate analysis |
Multivariable analysis |
||
|---|---|---|---|---|
| IRR (95% CI) | p | IRR (95% CI) | p | |
| Season | ||||
| Fall | Ref | – | Ref | – |
| Winter | 0.68 (0.62–0.75) | <0.001 | 1.10 (0.97–1.25) | 0.316 |
| Spring | 1.05 (0.96–1.15) | 0.281 | 1.09 (0.99–1.19) | 0.066 |
| Summer | 1.33 (1.22–1.45) | <0.001 | 0.95 (0.86–1.05) | 0.316 |
| Precipitation | ||||
| Neither rain nor frozen precipitation | Ref | – | Ref | – |
| Frozen precipitation only | 0.58 (0.49–0.69) | <0.001 | 1.09 (0.91–1.31) | 0.369 |
| Rain only | 0.84 (0.77–0.91) | <0.001 | 0.82 (0.75–0.90) | <0.001 |
| Rain and frozen precipitation | 0.43 (0.28–0.68) | <0.001 | 0.71 (0.45–1.13) | 0.151 |
| Total precipitation (centimeters) | 0.89 (0.78–1.02) | 0.093 | ||
| Time of day | ||||
| Morning 05:51–11:50 | Ref | – | Ref | – |
| Afternoon 11:51–17:50 | 4.79 (4.23–5.44) | <0.001 | 4.05 (3.57–4.61) | <0.001 |
| Night 17:51–23:50 | 6.41 (5.67–7.25) | <0.001 | 5.59 (4.94–6.33) | <0.001 |
| Overnight 23:51–05:50 | 0.69 (0.58–0.83) | <0.001 | 0.69 (0.58–0.82) | <0.001 |
| Day of week | ||||
| Weekday | Ref | – | Ref | – |
| Weekend | 1.23 (1.15–1.32) | <0.001 | 1.24 (1.15–1.32) | <0.001 |
| 6 h mean temperature (°C) | 1.05 (1.05–1.05) | <0.001 | 1.04 (1.03–1.04) | <0.001 |
| 6 h mean visibility (kilometers) | 1.07 (1.06–1.08) | <0.001 | ||
IRR incidence rate ratio, CI confidence interval
Bold values indicate statistical significance (p < 0.05)
Univariate negative binomial models identified increased trauma admission rates (IRR, 95% CI) in summer (1.33, 1.22–1.45) compared to fall; afternoon (4.79, 4.23–5.44) and night (6.41, 5.67–7.25) as compared to morning; weekend days (1.23, 1.15–1.32); in each additional 1 °C increase in temperature (1.05, 1.05–1.05), and in each additional kilometer of visibility (1.07, 1.06–1.08). A decreased IRR was seen in the winter season (0.68, 0.62–0.75), presence of frozen precipitation (0.58, 0.49–0.69), rain (0.84, 0.77–0.91), rain or frozen precipitation (0.43, 0.28–0.68), and in the overnight hours (0.69, 0.58–0.83). Linearity assumptions were assessed and confirmed by visual inspection of associations with categorical variables of 5 °C increments.
Multivariable analysis (Table 2)
In the final model, IRR of trauma increased during the afternoon (4.05, 3.57–4.61) and night periods (5.59, 4.94–6.33), weekends (1.24, 1.15–1.32), and with every 1 °C increase in temperature (1.04, 1.03–1.04). The presence of rain had a decreased IRR of admission (0.82, 0.75–0.90), as did the presence of overnight hours (0.69, 0.58–0.82) when compared to morning. While season was a significant contributor to model fit, no single season was independently predictive of trauma admission after accounting for other variables. In the alternative multivariable model including only seasons and temporal variables, a higher odds of trauma admission was noted in the summer (1.32, 1.22–1.45) compared to fall, afternoon (4.79, 4.22–5.43) and night (6.40, 5.66–7.23) compared to morning, and weekend (1.23, 1.15–1.32) compared to weekday. A lower odds of trauma admission was noted during the winter (0.68, 0.62–0.76) compared to fall and during the overnight (0.69, 0.58–0.83) period compared to morning (Online Resource). The Akaike Information Criterion (AIC) for the primary model including weather variables was 32,705, which demonstrated better model fit compared to that from an alternative model using only season and temporal variables (AIC 32,946).
Discussion
Using a large regional registry derived from a pediatric level 1 trauma center, we identified seasonal, weather, and timing factors associated with pediatric trauma admissions. Via development of a multivariable model, we identified associations between trauma admission rates and time of day and day of the week. The rate of trauma admissions increased by 4% with an increase in each 1 °C averaged over the 6 h prior to presentation at the ED and was decreased with the presence of rain.
After adjusting for direct measures of weather (temperature and precipitation), timing factors (time of day and day of week) appeared to have a strong association with the rate of trauma admissions when compared to seasonal factors. These periods correspond to times when children are more likely to be out of school, thereby increasing the risk of injury. A weekend or holiday was associated with an increased pediatric trauma admission in a study from the UK [10]. Similarly, in a single-center study from South Africa, children were noted to present more frequently with trauma from MVCs on weekends [16]. Similar findings have been reported from trauma centers which primarily serve adults [6, 8]. While the association of pediatric trauma with time of presentation has not been previously reported in the literature, our findings correlate with a review of emergency medical services utilization for trauma in Taiwan, demonstrating an increase in IRR during daytime and evening hours [15]. As the majority of the trauma admissions in our series were children in MVCs in vehicles that were likely driven by adults, it is not surprising that rates of pediatric trauma admission follow these broad trends.
Rain was negatively associated with admissions, and a rise in temperature increased the IRR of admission. These findings parallel reports by previous investigators identifying a positive association between fractures in pediatric patients and warmer weather [15, 17], and a negative association with precipitation [17]. A study from Scotland evaluating injuries presenting to the ED in children over a 3-month period in the summer found that more presentations occurred on sunnier and warmer days as compared to cloudier, cooler days [11]. A rise in maximum daily temperature correlated with the increases in both pediatric and adult trauma admissions in a study from the UK, with a greater effect size in children than in adults [10]. The results of our study correspond with these reports while additionally taking a more granular approach toward each admission by evaluating temperature and the presence of precipitation in the hours proximal to the traumatic event rather than overall temperature measurements for each day. Time and weather-based prediction modeling may be useful from the perspective of emergency preparedness and staffing. Weather forecasts continue to improve over time [18], and a better understanding of factors affecting trauma presentation can facilitate efficient staffing and resource utilization by trauma centers and emergency medical service providers. Notably, if there is a greater risk of trauma admissions on weekends and evening, better efforts should be made to staff trauma centers during these hours. In one single-center study from Australia, for example, poorer outcomes have been noted in some subgroups of trauma patients admitted after staffing decreases in the evening [19]. Additionally, with the overall rise in temperature predicted with climate change [20], these data may provide information regarding changes in the epidemiology of pediatric trauma over time. As global temperatures slowly rise, there may be an associated increase in rates of pediatric trauma admissions.
Findings from this study are subject to limitations from retrospective chart review. This study relied on previously collected data from a trauma registry in order to construct a multivariable model. In order to improve the accuracy and interpretability of the results, a large fraction of patients with minor trauma or those transferred from outlying facilities were excluded. Findings from this study are from patients local to a single center, which may limit the generalizability of results. However, despite these limitations, the overall trends with respect to the timing and weather-related prediction of pediatric trauma are broadly applicable to regions with temperate climates in the Northern Hemisphere.
Conclusion
Rates of local pediatric trauma admissions are most strongly associated with timing. However, even after taking temporal variables into account, climatologic factors were independently associated with trauma; the presence of rain lowered the rate of trauma, while each degree increase in temperature led to a rise in the rate of trauma admission by 4%. The findings from this study provide useful information for resource management by pediatric trauma centers and also shed light on the epidemiology of pediatric trauma.
Supplementary Material
Acknowledgments
Funding This project was supported in part by the National Institutes of Health through Grant No. UL1-TR-001857.
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00268–019-05029–4) contains supplementary material, which is available to authorized users.
Compliance with ethical standards
Conflict of interest The authors have no conflicts of interest relevant to this article to disclose.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention: National Center for Injury Prevention and Control Web-based Injury Statistics Query and Reporting System (WISQARS) https://www.cdc.gov/injury/wisqars/fatal.html. Accessed 28 June 2018
- 2.Wier LM, Yu H, Owens PL, Washington R (2010) Overview of children in the emergency department, 2010: Statistical Brief #157 https://www.ncbi.nlm.nih.gov/books/NBK154386. Accessed 27 Apr 2018 [PubMed]
- 3.Avraham JB, Bhandari M, Frangos SG et al. (2017) Epidemiology of paediatric trauma presenting to US emergency departments: 2006–2012. Inj Prev 25(2):136–143. 10.1136/injuryprev-2017-042435 [DOI] [PubMed] [Google Scholar]
- 4.Qiu L, Nixon WA (2008) Effects of adverse weather on traffic crashes. Transp Res Rec J Transp Res Board 2055:139–146. 10.3141/2055-16 [DOI] [Google Scholar]
- 5.Eisenberg D, Warner KE (2005) Effects of snowfalls on motor vehicle collisions, injuries, and fatalities. Am J Public Health 95:120–124. 10.2105/AJPH.2004.048926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhattacharyya T, Millham FH (2001) Relationship between weather and seasonal factors and trauma admission volume at a Level I trauma center. J Trauma 51:118–122 [DOI] [PubMed] [Google Scholar]
- 7.Nahmias J, Poola S, Doben A et al. (2017) Seasonal variation of trauma in western Massachusetts: fact or folklore? Trauma Surg Acute Care Open 2:e000120 10.1136/tsaco-2017-000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ho VP, Towe CW, Chan J, Barie PS (2015) How’s the weather? Relationship between weather and trauma admissions at a Level I Trauma Center. World J Surg 39:934–939. 10.1007/s00268-014-2881-8 [DOI] [PubMed] [Google Scholar]
- 9.Atherton WG, Harper WM, Abrams KR (2005) A year’s trauma admissions and the effect of the weather. Injury 36:40–46. 10.1016/j.injury.2003.10.027 [DOI] [PubMed] [Google Scholar]
- 10.Parsons N, Odumenya M, Edwards A et al. (2011) Modelling the effects of the weather on admissions to UK trauma units: a cross-sectional study. Emerg Med J 28:851–855. 10.1136/emj.2010.091058 [DOI] [PubMed] [Google Scholar]
- 11.Macgregor DM (2003) Effect of weather on attendance with injury at a paediatric emergency department. Emerg Med J 20:204–205. 10.1136/EMJ.20.2.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Census Bureau QuickFacts: Allegheny County, Pennsylvania https://www.census.gov/quickfacts/fact/table/alleghenycountypennsylvania/PST045216. Accessed 27 Apr 2018
- 13.National Weather Service National Weather Service Annual Climate Reports http://w2.weather.gov/climate/index.php?wfo=pbz. Accessed 28 June 2018
- 14.U.S. Department of Commerce National Oceanic and Atmospheric Administration http://www.noaa.gov/. Accessed 4 May 2018
- 15.Lin L-W, Lin H-Y, Hsu C-Y et al. (2015) Effect of weather and time on trauma events determined using emergency medical service registry data. Injury 46:1814–1820. 10.1016/j.injury.2015.02.026 [DOI] [PubMed] [Google Scholar]
- 16.Burstein B, Fauteux-Lamarre E, van As AB (2016) Increased morbidity associated with weekend paediatric road traffic injuries: 10-year analysis of trauma registry data. Injury 47:1236–1241. 10.1016/j.injury.2016.02.021 [DOI] [PubMed] [Google Scholar]
- 17.Livingston KS, Miller PE, Lierhaus A et al. (2016) Does weather matter? The effect of weather patterns and temporal factors on pediatric orthopedic trauma volume. Open Orthop J 10:550–558. 10.2174/1874325001610010550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose B, Floehr E (2005) Analysis of high temperature forecast accuracy of consumer weather forecasts from 2005–2016 https://www.forecastwatch.com/wp-content/uploads/High_Temperature_Accuracy_Study_12_Years.pdf. Accessed 30 June 2018
- 19.Mitra B, Cameron PA, Fitzgerald MCB et al. (2014) ‘‘After-hours’’ staffing of trauma centres and outcomes among patients presenting with acute traumatic coagulopathy. Med J Aust 201:588–591 [DOI] [PubMed] [Google Scholar]
- 20.Brown PT, Caldeira K (2017) Greater future global warming inferred from Earth’s recent energy budget. Nature 552:45–50. 10.1038/nature24672 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


