Abstract
Background
Atrial fibrillation, a progressively rising global health problem, is also rising in Hemophiliacs due to an increase in life expectancy in them. While treating Hemophiliacs with AF, deciding eligibility, choosing the anticoagulant based on risk-benefit ratio are tough decisions for physicians to make. This review paper aims to explore and compare existing studies, reviews and consensus papers to assess the safety of different Novel Oral Anticoagulants (NOACS) in this population.
Methods
Thorough literature search was conducted on Pubmed using Atrial Fibrillation, Hemophilia A, Oral anticoagulants, stroke prevention, Dabigatran, factor Xa inhibitors as keywords separately and in combinations. Papers in English language only from the past 5 years were selected for review. After removing duplicate results, 80 papers were selected and after applying different exclusion criteria and according to relevance, 40 papers were finalized for review.
Results
The keywords AF, Stroke prevention, oral anticoagulants, Hemophilia a, Factor Xa inhibitors and Dabigatran gave 24899, 13619, 8964, 3503, 2850, 2799 results, respectively. Combination keywords also showed some papers and out of short-listed 80 relevant papers 35 were finalized. Reviewing and analyzing these papers revealed no clinical trials in hemophiliacs with AF in the past 5 years and 5 clinical trials comparing NOACs with Warfarin in general population. Rest were systematic reviews, consensus papers and meta-analyses on management in this group. A few compared these drugs for AF in the general population but not specifically in Hemophiliacs and others. consensus papers developed suggestions for management and showed that NOACs are superior to Warfarin but need individual evaluation in Hemophiliacs with AF.
Conclusions
Patients with Hemophilia can also have thrombo-embolism despite their bleeding tendency and NOACs are a better option in them because of less need for monitoring, no food interactions and fewer drug interactions. This comparative review emphasized the need for more work to develop proper guidelines for thrombo-prophylaxis management in this specific group.
Keywords: Atrial fibrillation, Hemophilia A, Warfarin, NOACs
Introduction
Global prevalence of Atrial Fibrillation (AF) was estimated to be 33.5 million in 2010 making up 0.5 % of the world population and is constantly rising [1]. In the United States, the estimates are around 2.7 to 6.1 million and are expected to rise to 12.1 million by 2030 [2] and in Europe, the expected rise is 17.9 million by 2060 [3]. AF is more common in adults more than 65 years of age but can occur in young patients as well. In the US 9% of people older than 65 have AF and 2% of people less than 65 are affected by it [4]. Such prevalence rate and the need for long term management of stroke and the complications related to it pose a huge burden on the healthcare system. United States spends approximately 26 billion dollars annually on managing AF and its related complications [2,4] and has approximately 750,000 hospitalizations each year and estimated mortality of 130,000 deaths per year [5].
AF is one the most commonly diagnosed and persistent arrhythmia globally which predisposes patients to unexpected, sudden and often fatal thrombo-embolic neurological events, increasing the risk of ischemic stroke 5-fold [6]. Preventing these complications is important to decrease the overall disease burden and so anticoagulants are considered after risk stratification through CHADS 2 scoring [7]. Oral anticoagulants also have a risk of unexpected bleeding including severe episodes [8]. Warfarin, a Vit. K antagonist, remained the gold standard anticoagulant to prevent embolic stroke [9] but needed strict monitoring of INR to keep it in the therapeutic range (2-3) and failed to do so may lead to increased bleeding risk [9]. Dabigatran, a direct thrombin inhibitor was the first direct oral anticoagulant which needed less monitoring as compared to Warfarin. Later newer anticoagulants factor Xa inhibitors were added which also needed less monitoring as compared to Warfarin.
Several trials compared the efficacy and the safety of the new oral anticoagulants with Warfarin and proved the newer drugs to be as effective as Warfarin and superior in decreasing the intracranial bleeding episodes and needing less frequent monitoring [10]. Non-K inhibitor anti-coagulants are being compared against each other for efficacy and safety to prevent complications in AF and not much data is available about challenging scenario about the choice of an anticoagulant when the patient has a predisposition to bleeding because of hereditary and acquired bleeding disorders yet needing anticoagulation based on CHADS 2 scoring. Attaining a balance in anticoagulation and bleeding episodes is a tough target and hence safety profile of the anticoagulants is important in order to prevent the patient from an ischemic stroke while avoiding hemorrhagic stroke and other major bleeding episodes. Hemophilia A is one such hereditary condition having limited information about safety of newer anticoagulants. It is an X-linked recessive condition with low levels of clotting factor VIII predisposing a person to excessive bleeding [11]. Owing to recent advances like CFC (Coagulation Factor Concentrates), life expectancy is increased but so are the complications which arise as a person ages like AF. The prevalence of AF was found to be as high as 0.84% in a cross-sectional survey from 14 Hemophilia centers in Europe [12].This value is similar to the prevalence of AF in general population [13] and increases with increasing age as it does in general population with 0.2 % in less than 60 years old hemophilia patients and reaches up to 3.4% in hemophiliacs more than 60 years of age [12].
Comparison of efficacy and safety profile of these two groups of non-Vit K anticoagulants can help in the better assessment of the scenario and in deciding the anticoagulant to be used in patients with bleeding tendencies without disturbing the delicate balance between preventing ischemic stroke and a chance of causing hemorrhagic stroke. Dabigatran had been in use already in hemophiliacs with AF, considering antidote was available and now with FDA approving the antidote for Riavroxaban, this provides clinicians with more options of anticoagulants and this review article aims to assess their safety in the scenario.
Methods
Research Strategy
Research was conducted to identify studies analyzing and assessing safety profile of newer anticoagulants in setting of AF with inherited bleeding disorders, specifically Hemophilia. PubMed was used as our main database to find the relevant articles. Keywords which were used for the search were Atrial fibrillation, Oral anticoagulants, Hemophilia A, Stroke prevention, Dabigatran, and factor Xa inhibitors. MeSH keywords Atrial fibrillation, Hemophilia and Dabigatran were also used for search.
Search results
Atrial fibrillation yielded 10146 research articles, Using the keyword Hemophilia A yielded 2850 research papers, Oral anticoagulants yielded research papers and Factor Xa inhibitors yielded total number of 3503. A combination of keywords Atrial fibrillation and Oral anticoagulants gave a total of 3953 research papers, Atrial fibrillation and stroke prevention yielded 3847 papers, Atrial fibrillation and Hemophilia a yielded 17 research papers. Atrial fibrillation, anti coagulation and Hemophilia a gave 10 articles and Stroke prevention with Hemophilia a gave 4 research papers. Out of these results a total of 80 articles relevant to the research question were selected. After applying inclusion and exclusion criteria, duplicate papers were removed and finally a total of 35 articles were selected for review. A few relevant research papers about mechanism of actions, published before past 5 years from references of selected papers were also included.
Inclusion/Exclusion criteria
Peer-reviewed, full-text research papers from past 5 years were included in the review. All selected articles were in English language and no global or geographical considerations were given. Any non peer- reviewed and duplicate papers were excluded from finally selected articles.
Results
Out of 35 finalized papers, there were no controlled clinical trials in Hemophiliacs population with AF but a few case studies showed up. A total of 5 clinical trials comparing the newer anticoagulants in general population with AF were included for review of their findings and indirect comparisons of these drugs, most of which showed superiority of NOACS over Warfarin. One retrospective cross-sectional study evaluating prevalence of AF in Hemophiliacs was included which showed increase in AF with increasing age. Anticoagulation is under-prescribed in these patients. two meta-analyses were included which indirectly compared clinical trials comparing NOACS with Warfarin. One of them had compared 3 clinical trials with 42,411 patients on NOACs and 29,272 patients on Warfarin and showed that NOACs are superior in efficacy in preventing stroke and safety in terms of prevention of major bleed specially Intracranial bleed, Rivaroxaban showed increased GI bleeding. Rest were review articles and consensus papers about managing thrombo-embolism in hemophiliacs with AF and other conditions needing anticoagulation. Results of these systematic reviews and consensus papers showed that depending on severity of Hemophilia and risk-benefit assessment, anti-coagulation can be started and NOACs were a preferable choice although final choice of anticoagulant depends on patient's individual evaluation.
Table 1. No. of research articles for the searched Keywords.
| Keywords / Combination of keywords | Database | No. of results |
|---|---|---|
| Atrial Fibrillation | PubMed | 24899 |
| Stroke prevention | PubMed | 13619 |
| Oral anticoagulants | PubMed | 8964 |
| Factor Xa inhibitors | PubMed | 3503 |
| Hemophilia a | PubMed | 2850 |
| Dabigatran | PubMed | 2794 |
| Atrial fibrillation AND Hemophilia a | PubMed | 17 |
| Hemophilia a AND anticoagulation | PubMed | 10 |
| Stroke prevention AND Hemophilia a | PubMed | 4 |
Table 2. Some of the studies/papers included in review.
| Author/Year | Country | Treatment | Focus of study | Type of study | Findings | Summary |
|---|---|---|---|---|---|---|
| De Koning et al, 2017 | Utrecht, The Netherlands | Oral anticoagulants | Thrombin generation in Hemophiliacs | Cross-sectional study | They concluded that patients with severe hemophilia had similar haemostatic ability as compared to patients who had a normal range INR and approximately one third of mild to moderate hemophilia had even better haemostatic ability than patients using Warfarin with normal INR. | Anti coagulation therapy needs to be an option for patients who have non-severe hemophilia with AF and need more research in this field which may help in the near future where treatment option can be guided by ETP. |
| Murray et al, 2018 | Santiago, Chile | Oral anticoagulants | Atrial fibrillation in Hemophiliacs | Case report | Factor VIII levels can alter with the changing time and can keep changing the risk-benefit assessment. | This case study suggests and sheds light on importance of individual risk-benefit assessment in hemophiliac patients with AF as risk factors and benefits of oral anticoagulants may vary especially in hemophilia A carriers where change in FVIII levels alters bleeding risk. |
| Martin and Key, 2016 | North Carolina, USA | Oral anticoagulants | Anti coagulation in patients with inherited bleeding disorders | Case-review series | Evidence based Management guidelines aren't available for this specific population. | Anticoagulation in hemophiliacs needed to be considered based on the individual risk of bleeding in these patients if the risk of thrombotic events is high. Strategies to used oral anticoagulants were discussed to manage venous thrombotic disease, atrial fibrillation in inherited bleeding disorders and atherothrombotic disease were discussed. |
| Lip et al, 2014 | UK/Denmark | Oral anticoagulants | Indirect comparison between Rivaroxaban, apixaban and dabigatran | Systemetic review | Dabigatran 110 mg and Apixaban were found to be equally safe as no significant differences were found. In comparison of Dabigatran 110 mg and Rivaroxaban, Dabigatran was associated with less major bleeding and intra cranial bleeding episodes. | In this indirect comparison between apixaban, Rivaroxaban and two doses of Dabigatran, they were found to be equally efficacious in preventing thrombotic stroke, although Dabigatran 110 mg was slightly more superior in preventing stroke. Dabigatran at lower dose of 110 mg and apixaban were safer as they had less episodes of major intracranial bleed. More accurate results will be obtained only when direct comparison is done between both groups of newer OACs. |
| Schutgens et al, 2016 | North Carolina, USA | Oral anticoagulants | Suggestions for anticoagulation in inherited bleeding disorders | Letter to the editor | Not enough clinical data was found and whatever work is available has smaller sample size. | Owing to the lack of clinical trials on larger cohorts giving us not enough examples from clinical settings, anticoagulation in hemophiliacs is a complex matter. Suggestions are made to serve as a guide to manage these patients and more clinical data is needed about safety and efficacy of anticoagulants and need implementation of certain measures. |
| Shutgens et al, 2014 ADVANCE working group | Europe (14 hemophilia centers) | Oral anticoagulation in Hemophilia | To review anticoagulant prescribing practices in hemophiliacs | Cross-sectional study | Atrial fibrillation (AF) is a common health problem in the general population, but data on prevalence or management in patients with haemophilia (PWH) are lacking. The aims of this study were to analyse the prevalence of AF and risk factors for stroke using a cross‐sectional pan‐European design and to document current anticoagulation practice. The ADVANCE Working Group consists of members from 14 European haemophilia centres. | Hemophilia's prevalence increases as the patient ages and is fairly common in mild Hemophilia. And the percentage of patients receiving any type of anticoagulation is only 33 %. CHADS2 VAS2 scoring may overestimate the stroke risk in this population and HAS BLED score may underestimate the risk of bleeding so both are not reliable enough in Hemophiliacs with AF. Oral anticoagulation with any oral anticoagulant may be considered in patients with high risk of stroke if FVII levels are adequate. |
| Lee et al, 2018 | Japan/ Taiwan | Rivaroxaban and Warfarin | Safety of low dose Rivaroxaban compared to Warfarin in Asian population. | Cohort study | In Asian population, Rivaroxaban had lower risk of thrombo-embolism than Warfarin. | Both low doses of Rivaroxaban were associated with a lower risk of ischemic stroke/systemic embolism, intracranial hemorrhage, gastrointestinal bleeding, all major bleeding, and all-cause mortality compared with Warfarin in Asian NVAF patients. The 15 mg Rivaroxaban dose was associated with a lower risk of acute myocardial infarction compared to Warfarin. |
| Ruff et al, 2014 | Boston, USA | Oral anticoagulants | Comparison of oral anticoagulant NOACs with Warfarin | Meta-analysis of RE-LY, ROCKET AF, ARISTOTLE, and ENGAGE AF-TIMI | A total of 42,411 participants received a NOAC and 29,272 participants received Warfarin. NOACs significantly reduced stroke or systemic embolic events by 19% compared with Vit K inhibitor, Warfarin. New oral anticoagulants also significantly reduced intracranial hemorrhage but Rivaroxaban was associated with increased gastrointestinal bleeding. | This was the first meta analysis which included phase 3 clinical trials about stroke prevention in AF by of all four new oral anticoagulants. Newer anticoagulants have better efficacy in terms of stroke prevention and safety in terms of less intracranial hemorrhage and mortality and better risk-benefit profile than Warfarin. Only type of systemic bleeding which occurred more than Warfarin was Gastrointestinal bleeding. |
| Villines et al, 2019 | USA (Department of Military health system) | Oral anticoagulants | Atrial fibrillation | Retrospective cohort study | Patients using Dabigatran demonstrated similar risk of ischemic stroke but less risk of hemorrhagic stroke compared to the patients using Rivaroxaban and for other major bleeding episodes in individual component sites, Dabigatran comparatively had lower risk of major intracranial bleed but risk was similar for major bleed at extra cranial sites. For comparison of Apixaban and Dabigatran both had similar risk of ischemic stroke but the risk of major intra cranial bleed could not be assessed due to low number of events but risk was same for extra cranial sites. | In the cohorts comparing Dabigatran and Rivaroxaban , Dabigatran had less bleeding risk but similar efficacy in stroke prevention. While comparison between Dabigatran and Apixaban no statistically significant conclusions were drawn because of small sample size. |
| Gremmal et al, 2018 | Austria | Use of oral anticoagulants in high risk population | To review use of NOACs in high risk population | Consensus paper | This consensus reviewed properties and use in a number of high risk populations like Chronic kidney disease, old age patients. | NOACs have a superior safety profile than Vit K inhibitors but it's important to consider dose reduction criteria and their contraindications to have proper risk-benefit assessment and outcome |
Discussion
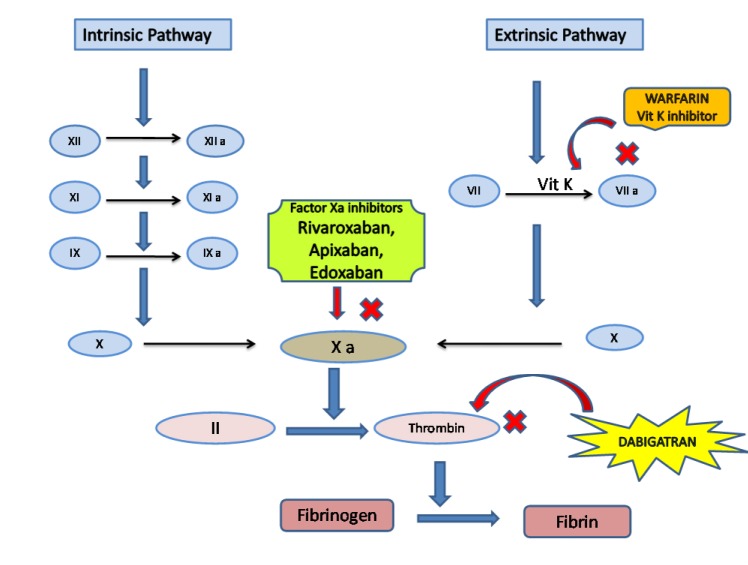
Both Intrinsic and extrinsic pathways of normal coagulation cascade involve a number of different clotting factors and have different triggers to get activated but later converge and have a common pathway. Intrinsic pathway is triggered by direct damage to the blood vessels and activates a series of coagulation factors whereas extrinsic is triggered by damage to the tissue which in turn activates Factor VII. Both pathways converge at a point where Factor X is activated which leads to the formation of Thrombin or activated Factor II and at the end fibrinogen is converted to fibrin. Certain co-factors are mandatory for the process to complete like Vit. K, Ca++, etc. Deficiency in some of these factors may be the cause of different inherited bleeding disorders making the person more prone to the bleeding episodes, and some risk factors may increase the chances of thrombo-embolism and may have serious consequences of its own therefore needing prophylaxis with anticoagulants. When these both conditions co-exist using anticoagulation needs more vigilant and conscious approach.
Mechanism of action and pharmacological properties of oral anticoagulants
Warfarin had been the main oral anticoagulant for around 50 years since 1945 and had been effective. It acts as Vit K inhibitor, so inhibits all the steps which are catalyzed by Vit. K. While using Warfarin it was very important to keep in mind the delicate balance which had to be maintained to avoid any bleeding episodes for which purpose INR monitoring was necessary and needed to be in between 2-3. INR can easily be affected by dietary and drug interactions so needed frequent monitoring. Dabigatran was introduced long after Warfarin in 2010 and has a different mechanism of action. It acted at the later stage of the coagulation cascade, as a thrombin inhibitor as shown in [Figure 2], so it affected both intrinsic and extrinsic pathway. It had an advantage of less need for monitoring of INR as compared to Warfarin. It was first among the NOAC's, the latest oral anticoagulants added to treat pro-thrombotic conditions are Factor Xa inhibitors inhibiting the activated Factor Xa both in free form and attached to the pro-thrombin complex. Considering its important site of action in the coagulation cascade it also affected both intrinsic and extrinsic pathways. It is a group of medications out of which frequently used drugs include Rivaroxaban, Apixaban etc. Rivaroxaban was approved in 2011. The problem remained that in case of any need of urgent or immediate reversal, they had no antidotes available, until an antidote for Dabigatran, Idarucizumab was approved and recently in 2018 an antidote for Rivaroxaban and Apixaban has been approved. Pharmacological properties of fXa inhibitors differed in many ways from earlier anti-coagulants as they targeted a specific factor instead of multiple factors and have a rapid onset of action and their bioavailability is also better in comparison to Warfarin [13]. Owing to this mechanism of action there is no effect of dietary intake on Vit.K inhibitors as it is on Warfarin and so a fixed dose is a convenience which a patient gets with them and along with these, they have fewer drug interactions [14]. Because their pharmacokinetics and pharmacodynamic properties depend on the dose given, they have a predictable response after a fixed dose is administered and so need lesser monitoring [15].
Figure 2. Site of action of Warfarin, Dabigatran and Factor Xa inhibitors.
Figure 1. PRISMA FLOW diagram showing the process of selection of research papers.
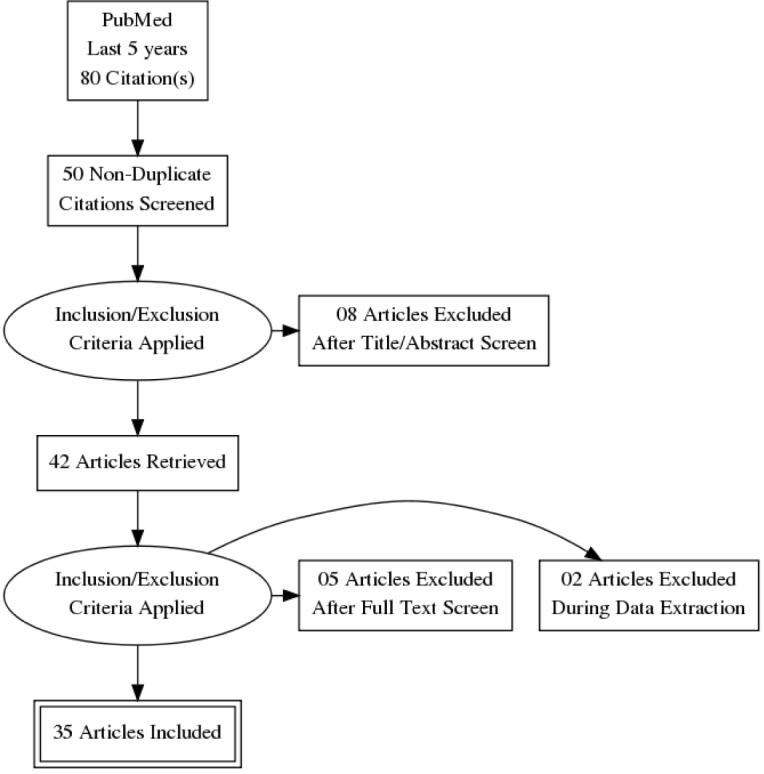
Table 3. Comparison of Pharmacological Properties of thrombin inhibitors and Factor Xa inhibitors.
| Characteristics | Thrombin Inhibitors | Factor Xa Inhibitors | ||
|---|---|---|---|---|
| Dabigatran | Rivaroxaban | Apixaban | Edoxaban | |
| Mechanism of action | Thrombin Inhibition | Factor Xa inhibition | Factor Xa inhibition | Factor Xa inhibition |
| Available doses | 75 mg, 150 mg | 2.5 mg, 10 mg, 15 mg, 20 mg | 2.5 mg, 5 mg | 15 mg, 30 mg, 60 mg |
| Food Interaction | None | None To be taken with food only for higher doses (20 mg) | None | None |
| Route of Elimination | Renal | Renal and Hepatic | Renal and Hepatic | Renal and Hepatic |
| Bioavailability | 6.2 % | 80 % | 50 % | 62 % |
| Half –life (Normal Renal function) | 12-14 hrs | 5-9 hrs Increase with old age | 12hrs | 10-14 hrs |
| Renal impairment with AF Mild ( >50ml/min) Moderate (15-50 ml/min) Severe (<15 ml/min) | No dose adjustment Reduce dose (75 mg/day when below 30ml/min) Avoid use | No dose adjustment 15 mg/day Avoid use | No dose adjustment Reduced dose (2.5 mg/day) Reduced dose (2.5mg) if on dialysis | No dose adjustment Reduced dose (30 mg/day) Avoid use Below |
| Hepatic Impairment Mild Severe | None | None Avoid use | None Not recommended | None Not Recommended |
When to start anticoagulation in Hemophiliacs with AF: Is CHADS2 VAS and HAS-BLED scoring enough?
Atrial fibrillation may cause intra-cardiac thrombus formation due to stasis and can cause thrombo-embolic stroke which may be life- threatening. Atrial fibrillation may be asymptomatic and this complication can be its first presentation, therefore screening and diagnosing it in time is important to prevent stroke. This is done by risk assessment for stroke through CHADS2 or CHADS VAS scoring and then prophylactic treatment is initiated in the form of oral anticoagulant based on the risk stratification and approved guidelines for general population. Hemophilia patients have now increased life expectancy owing to recent advances like the use of Recombinant FVIII in management but so are the conditions which are more prevalent in old age, this makes Atrial fibrillation to rise in hemophiliacs as well [16]. These patients already have a bleeding tendency and whether they need anticoagulation is an important question which is frequently encountered while managing such patients. Despite the defect in clotting in hemophiliacs they still have other risk factors to develop thrombotic cardiovascular diseases [17]. Another study evaluating the risk factors for cardiovascular diseases between hemophiliacs and non hemophiliac controls although showed that controls have slightly higher incidence but as result was not statistically significant so recommended that they should be evaluated on individual basis [18]. Even with the use of recombinant FVIII there is still a risk of thrombosis in mild and moderate hemophilia, severe cases are somewhat protected though may still have a chance of thrombo-embolism [19]. Reducing the risk of stroke in patients with Atrial fibrillation depends on attaining an optimal risk and benefit balance which means estimating the risk of developing stroke due to thrombo-embolism by CHADS 2 OR CHADS2 VAS and then estimating the risk of bleeding secondary to using oral anti-coagulant by HAS-BLED score [20]. But will the same risk-benefit assessment criteria and guidelines give an idea about anticoagulation in Hemophiliacs with AF as they have increased propensity to bleed. There are very few trials addressing anticoagulation for AF in this specific population or group of patients and currently, no proper guidelines for risk assessment and management are developed as yet and only few expert consensuses developed to address this knowledge gap are available and serve as a guide to physicians [21,16]. Since the bleeding risk is high,an approach is devised in the form of an algorithm [16].
Normally patients are stratified for risk according to CHADS2-VAS scoring and HAS-BLED or FVIII levels, and then a score of >3 or equal to 3 is used to start prophylactic anticoagulation. But no cut off value was available for Hemophiliacs with AF and so one such consensus was developed and it was suggested to be >2 or equal to 2 and the level of Factor VIII to be lowered from 30% to 20% [22], and it's recommended not to start anticoagulation if this level is below 20% [22]. However this threshold should still be evaluated according to the particular patient who is under consideration [20].
The case report and literature analysis by Murray et al focused on a female patient, a hemophilia carrier, and highlighted that every case of hemophilia with Atrial fibrillation should be evaluated individually depending on their individual risk-benefit evaluation. They emphasized that as levels of Factor VIII in females may vary with time and can change the risk-benefit balance and assessment so any hemophilia A carrier with low factor VIII levels may have a decreased risk of bleeding [20] so an individual assessment will give a better idea about when to start and what to consider for anticoagulation.
During individual assessment, the primary consideration while making a decision is the bleeding phenotype of the patient, which is whether the patient bleeds spontaneously, whether bleeding occurs due to an initiating stimulus like trauma and how severely a patient bleeds [23]. Developing inhibitory antibodies in Hemophiliac is frequently encountered complication .The hemophilia patients who don't have an inhibitor generally respond well to clotting factor replacement, thus making it easier to control or prevent severe bleeding [23]. On the other hand, patients who have inhibitors have a less predictable response. it was shown by some studies that around 10% to 20% of bleeding episodes with inhibitors were not responsive at all or responded partially to a bypassing agent [24,25]. This evaluation can serve as a guide in assessing the risk-benefit ratio of a hemophiliac patient and whether the patient needs a thrombo-prophylaxis in Atrial fibrillation or not.
Regarding whether to start thrombo-prophylaxis in hemophilia, De Koning and colleagues suggested/concluded in their literature review that approximately one third patients with non-severe hemophilia had a significantly better haemostatic potential than the patients who were on Vit K inhibitors with therapeutic INR whereas patients with severe hemophilia had equally comparable haemostatic potential to the patients with therapeutic INR, which showed that a considerable number of patients with non-severe hemophilia should be considered for thrombo-prophylaxis [26].
MAINTAINING BALANCE BETWEEN ANTICOAGULATION AND BLEEDING RISKS IN BLEEDING PRONE POPULATION/ ISCHEMIC STROKE VS HEMORRHAGIC STROKE
As the main complication of inherited bleeding disorders like Hemophilia is spontaneous or post-traumatic bleeding, they are somewhat protected from thrombosis but both arterial and venous thrombosis do occur occasionally, so they may need anticoagulation as the situation arise and also consideration is needed to start prophylactic anti-coagulants as the need can be comparable to general population like in the presence of AF [23] where the complication can be more serious. But with tendency of increased bleeding and taking oral anti-coagulant can have their own risk of bleeding if INR fluctuates or if medication is affected by dietary intakes or drug-drug interactions as was the case in Warfarin where regular monitoring was needed, but with the new direct oral anticoagulants, there is an increased safety profile, as proven by many studies especially considering intra-cerebral hemorrhage [27].
In general population, all DOACS were considered safer than Warfarin and as effective as it is but there isn't much evidence as not many trials have been done specifically in hemophiliacs so a literature review and review of different consensus done earlier can help us in analyzing and comparing the effectiveness and safety of DOACS in hemophiliacs. Although Rivaroxaban and Apixaban are proven to be superior and safer to Warfarin in patients with AF, they still do have a chance of increased bleeding as in all anti-coagulants [28]. It was suggested that instead of using Warfarin, it will be safer in order to prevent a major bleeding episode by prescribing Rivaroxaban, a factor Xa inhibitor at a lower dose of 10 mg daily [22] but in such patients, anti-coagulation is to be considered if a factor VIII level is more than 20%.
In hemophiliacs, if oral anti-coagulants have to be used it is comfortable to use them when trough FVII/FIX and vWF activity levels are >30% and are maintained on that but still a final decision has to be taken after a thorough individual evaluation but in patients with severe hemophilia where the factor activity level is at times even <1%, anti-thrombotic therapy is avoided as bleeding tendency is already very high especially if no clotting factor therapy is ongoing [23]. A multicenter study involving 33 hemophilia patients from 20 European hemophilia centers showed that bleeding occurred in 1 out of 3 hemophilia patients on oral anticoagulant who was not taking prophylactic treatment with clotting factors alongside to maintain factor 8 trough level above 0.2 IU L -1, and this questions the safety of the drugs in this group despite being safe in general population and may need detailed assessment and prophylactic clotting factors before starting their use [12].
Lower doses of Rivaroxaban were proven to be safer than Warfarin as they were associated with lower risk of ischemic stroke and systemic embolism in one of the studies conducted in Asian NVAF patients [29]. Newer anti-coagulant agents reduced the risk of Intra-cranial hemorrhage by half approximately having a risk ratio of 0.44, 95% CI in a study [30].
BEST DRUG IN MAINTAINING OPTIMAL BALANCE
While choosing an anticoagulant for patients who have a high risk of bleeding and inherited bleeding disorders, among all available oral anticoagulant options, considerations should be given to the bleeding risk with each medicine, its reversibility and half-life. Agents with shorter half-life are preferred in patients with bleeding disorders as they are easy to reverse. Warfarin and Dabigatran were frequently used because of the availability of available antidotes [23]. Factor Xa inhibitors were not used in this category of patients as they had no available antidote but recently with approval of antidote of Rivaroxaban and increased safety of FXa inhibitors as compared to Warfarin, they also should be an agent of choice. The issue which arises here now is which agent to choose among Dabigatran and Factor Xa inhibitors.
Considering the high-risk Warfarin has, NOACs are definitely a safer option; Vit K antagonists have more adverse events because of their narrow therapeutic margin and many drug and food interactions. It is considered a leading cause of ER presentations/hospitalizations in the elderly due to its adverse effects [31]. Not many clinical trials are done to assess the safety and efficacy in hemophiliacs with AF, so by comparing the clinical trials in other high risk population and assessing which medications are safer than Warfarin and relative to each other and comparing reviews, consensus and meta-analysis about such scenario, we can indirectly compare the safety and efficacy of such medication. Rivaroxaban was found to be superior to Warfarin in many high risk populations in a review by Diener et al, by comparing the results of ROCKET_AF trial and were found to be consistent in these populations [32]. The EXPAND study conducted in Japan showed low dose of Rivaroxaban in non valvular Atrial fibrillation to have lesser incidence of stroke, and serious bleeding than it's higher dose and Warfarin [33].
The elderly population is a high risk population, whose thrombo-embolic risk is higher than general population using CHADS VASc score which makes age an important factor in scoring, but anticoagulation is not commonly used as needed and anti-platelet agents without anticoagulants are not of much benefit in the elderly but are more prone to cause major bleeding episode [34]. This high-risk group tests the ability of the medication's safety considering the different co-morbidities, the poly-pharmacy in them and the interactions those medications may have as AF is common in the ageing population. With the increased life expectancy in hemophiliacs and the increasing AF in this population, consideration of the medicine which is safe in the ageing population can be considered in this population as well. NOAC's are considered a safer option in the elderly population because of their short half-life and predictable pharmacokinetics and less need for monitoring as Warfarin and the trials showing the decreased chances of intracranial hemorrhage. A meta-analysis by Ruff et al showed these results about their safety and efficacy in 29000 patients over the age 75 [35].
Renal impairment is a condition which is not uncommon in patients with AF, in ageing population and patients with hemophilia. NOAC's have renal route of excretion and so is one of the main limitations when they need to be prescribed to CRF population. Consideration of GFR is important while deciding the oral anticoagulant which needs to be greater than 30 ml/min for prescribing NOACs. An expert Consensus document preferred using Anti Xa inhibitors instead of Vit K Inhibitors with GFR rate ranging from 15-30 ml/min, they were found to have an upper hand in terms of safety in patients with renal impairment as compared to Vit K inhibitors [36]. 20 mg rivaroxaban is superior in efficacy to Warfarin but even low dose of Rivaroxaban at 15 mg was also proven equally efficacious in another study done in Japanese population [29] which can be used in patients with compromised renal functions or even in Hemophiliacs or with both.
In a retrospective study by Villines et al, patients with Dabigatran were compared to Rivaroxaban and to Apixaban separately but the sample size of Apixaban was not statistically significant but for comparison of Dabigatran and Rivaroxaban showed that Dabigatran was associated with less major bleeding events than Rivaroxaban although the rates of thrombo-embolic rate were not different in both of them. So in terms of efficacy both were comparable but in safety from a major bleed Rivaroxaban was found to be superior in this study [37].
The results of one of the studies in which patients with NVAF of >65 years were selected which were recently started on these medications, showed that there was no difference in thrombo-embolic stroke in patients on Rivaroxaban or Dabigatran but an increase in Intra cranial hemorrhage and major bleeding episode risk in the cohort taking Rivaroxaban compared to the one taking Dabigatran [38]. The results of both of these studies were somewhat similar to the results of a few other recent studies like a meta-analysis of different studies by Li et al which also showed that Rivaroxaban, a thrombin inhibitor and Apixaban, a factor Xa inhibitor were comparable in efficacy with Rivaroxaban, another factor Xa inhibitor, but both were better in safety as they were associated with lesser episodes of major bleeding than Rivroxaban [39]. A meta-analyses of 7 studies by Providencia et al concluded that none among both groups Factor Xa and thrombin inhibitors are better in all parameters, one group may be better than other in one thing and may be inferior in other one [40] and hence decision should be taken on individual patient's risk-benefit ratio which is even more important in Hemophiliacs. In those cases where Vit K inhibitors cannot be prescribed, Apixaban was found to be safer alternative [34]. A Consensus report by Gremmel et al also recommended to assess each patient individually for the need of anticoagulation, as except for severe Hemophilia, others may not be protected enough against thrombo-embolism [41], so the decision of specific drug also needs to take in account the specific conditions and co-morbidities of patient. Considering all these limitations, the option of Left Atrial Appendage closure can also be considered and needs to be studied in this group as it may help us to avoid the oral anticoagulants altogether in this group while still preventing thrombosis. A meta-analysis of PROTECT AF and Prevail trial showed similar chances of having ischemic stroke but decreased chances of hemorrhagic stroke as compared to Warfarin [42].
Limitations
While searching for the literature, there were not many clinical trials or studies which were conducted in the Hemophiliacs with AF, the ones which were available were in general population. Most of the papers specifically in the concerned population were the consensus recommendations based on clinical cases or indirect comparisons of different studies. There were no literature/guidelines found about risk assessment in this population group and the risk assessment criteria like CHADs and HAS-BLED score cannot be applied to this population group, making the decision of prophylactic anticoagulation more difficult. Actual comparison between these drugs in this specific population was difficult and conclusions were drawn based on literature available and their properties in general population or clinical case reviews. More clinical trials are needed to study these drugs in hemophiliacs with AF.
Conclusions
NOAC's although considered a better option in general public have not been studied for efficacy and safety in Hemophiliacs with AF. Hemophilia patients despite having a bleeding risk and decreased tendency for thrombosis may still have thrombosis in pro-thrombotic conditions like Atrial fibrillation. This makes it clear that these patients also have the need for prophylactic anticoagulation as the complication is more serious, but the unreliability of risk assessment scores in this group of patients also needs to be considered. Warfarin was in use for decades for prophylaxis and had been effective in preventing thrombo-embolic stroke but needed frequent monitoring of INR and had frequent drug and food interactions which may make it difficult for these patients. NOACs having different site of action are not dependant on food intake, and the need of less monitoring of INR make it a better option in hemophiliacs with AF having a predictable response, but they may still need clotting factors alongside to prevent major bleeding event, depending on individual assessment. As these conclusions are drawn from research about thrombo-prophylaxis on various other vulnerable groups, more studies are needed to extrapolate these effects in this group. Among NOACs, as shown in different trials / meta-analysis, Dabigatran and Apixaban were shown to be better than Rivaroxaban in having fewer episodes of major intra-cranial bleeding episodes but have the same efficacy in preventing strokes. In case of co-existing CRF since all NOACs have renal route of excretion as well need dose adjustment and need to be decided based on eGFR. Apixaban was the one which could be prescribed in GFR even between 15- 30. There still is a huge gap in knowledge and there is need for more clinical trials in this specific population as not much is available and there is a need to develop proper guidelines about using oral anti-coagulants in Atrial fibrillation with Hemophilia and Inherited coagulation disorders. Considering all these limitations, options like Left Atrial Appendage (LAA) occlusion device therapy may be considered and studied further in this group as a treatment option to avoid long term anti-coagulation in this vulnerable population having high risk of bleeding.
References
- 1.Chugh Sumeet S, Havmoeller Rasmus, Narayanan Kumar, Singh David, Rienstra Michiel, Benjamin Emelia J, Gillum Richard F, Kim Young-Hoon, McAnulty John H, Zheng Zhi-Jie, Forouzanfar Mohammad H, Naghavi Mohsen, Mensah George A, Ezzati Majid, Murray Christopher J L. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129 (8):837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian Dariush, Benjamin Emelia J, Go Alan S, Arnett Donna K, Blaha Michael J, Cushman Mary, de Ferranti Sarah, Després Jean-Pierre, Fullerton Heather J, Howard Virginia J, Huffman Mark D, Judd Suzanne E, Kissela Brett M, Lackland Daniel T, Lichtman Judith H, Lisabeth Lynda D, Liu Simin, Mackey Rachel H, Matchar David B, McGuire Darren K, Mohler Emile R, Moy Claudia S, Muntner Paul, Mussolino Michael E, Nasir Khurram, Neumar Robert W, Nichol Graham, Palaniappan Latha, Pandey Dilip K, Reeves Mathew J, Rodriguez Carlos J, Sorlie Paul D, Stein Joel, Towfighi Amytis, Turan Tanya N, Virani Salim S, Willey Joshua Z, Woo Daniel, Yeh Robert W, Turner Melanie B. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015 Jan 27;131 (4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Krijthe Bouwe P, Kunst Anton, Benjamin Emelia J, Lip Gregory Y H, Franco Oscar H, Hofman Albert, Witteman Jacqueline C M, Stricker Bruno H, Heeringa Jan. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 2013 Sep;34 (35):2746–51. doi: 10.1093/eurheartj/eht280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 02;130 (23):2071–104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Atrial Fibrillation Fact Sheet|Data Statistics|DHDSP|CDC [Internet]. [cited 2019 Mar 23]. 2001;0:0–0. [Google Scholar]
- 6.Kimura K, Minematsu K, Yamaguchi T. Atrial fibrillation as a predictive factor for severe stroke and early death in 15,831 patients with acute ischaemic stroke. J. Neurol. Neurosurg. Psychiatry. 2005 May;76 (5):679–83. doi: 10.1136/jnnp.2004.048827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Voukalis C, Shantsila E, Lip G Y. Clinical Stroke prevention in atrial fibrillation. J R Coll Physicians Edinb. 2017 Mar;47 (1):13–23. doi: 10.4997/JRCPE.2017.105. [DOI] [PubMed] [Google Scholar]
- 8.Kirchhof Paulus, Lip Gregory Y H, Van Gelder Isabelle C, Bax Jeroen, Hylek Elaine, Kaab Stefan, Schotten Ulrich, Wegscheider Karl, Boriani Giuseppe, Brandes Axel, Ezekowitz Michael, Diener Hans, Haegeli Laurent, Heidbuchel Hein, Lane Deirdre, Mont Luis, Willems Stephan, Dorian Paul, Aunes-Jansson Maria, Blomstrom-Lundqvist Carina, Borentain Maria, Breitenstein Stefanie, Brueckmann Martina, Cater Nilo, Clemens Andreas, Dobrev Dobromir, Dubner Sergio, Edvardsson Nils G, Friberg Leif, Goette Andreas, Gulizia Michele, Hatala Robert, Horwood Jenny, Szumowski Lukas, Kappenberger Lukas, Kautzner Josef, Leute Angelika, Lobban Trudie, Meyer Ralf, Millerhagen Jay, Morgan John, Muenzel Felix, Nabauer Michael, Baertels Christoph, Oeff Michael, Paar Dieter, Polifka Juergen, Ravens Ursula, Rosin Ludger, Stegink W, Steinbeck Gerhard, Vardas Panos, Vincent Alphons, Walter Maureen, Breithardt Günter, Camm A John. Comprehensive risk reduction in patients with atrial fibrillation: emerging diagnostic and therapeutic options--a report from the 3rd Atrial Fibrillation Competence NETwork/European Heart Rhythm Association consensus conference. Europace. 2012 Jan;14 (1):8–27. doi: 10.1093/europace/eur241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Caterina Raffaele, Husted Steen, Wallentin Lars, Andreotti Felicita, Arnesen Harald, Bachmann Fedor, Baigent Colin, Huber Kurt, Jespersen Jørgen, Kristensen Steen Dalby, Lip Gregory Y H, Morais João, Rasmussen Lars Hvilsted, Siegbahn Agneta, Verheugt Freek W A, Weitz Jeffrey I. Vitamin K antagonists in heart disease: current status and perspectives (Section III). Position paper of the ESC Working Group on Thrombosis--Task Force on Anticoagulants in Heart Disease. Thromb. Haemost. 2013 Dec;110 (6):1087–107. doi: 10.1160/TH13-06-0443. [DOI] [PubMed] [Google Scholar]
- 10.Kirchhof Paulus, Benussi Stefano, Kotecha Dipak, Ahlsson Anders, Atar Dan, Casadei Barbara, Castella Manuel, Diener Hans-Christoph, Heidbuchel Hein, Hendriks Jeroen, Hindricks Gerhard, Manolis Antonis S, Oldgren Jonas, Popescu Bogdan Alexandru, Schotten Ulrich, Van Putte Bart, Vardas Panagiotis. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016 Oct 07;37 (38):2893–2962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 11.Patel Devin N, Felder Seth I, Luu Michael, Daskivich Timothy J, N Zaghiyan Karen, Fleshner Phillip. Early Urinary Catheter Removal Following Pelvic Colorectal Surgery: A Prospective, Randomized, Noninferiority Trial. Dis. Colon Rectum. 2018 Oct;61 (10):1180–1186. doi: 10.1097/DCR.0000000000001206. [DOI] [PubMed] [Google Scholar]
- 12.Schutgens Roger E G, Klamroth R, Pabinger I, Malerba M, Dolan G. Atrial fibrillation in patients with haemophilia: a cross-sectional evaluation in Europe. Haemophilia. 2014 Sep;20 (5):682–6. doi: 10.1111/hae.12445. [DOI] [PubMed] [Google Scholar]
- 13.Kubitza Dagmar, Becka Michael, Wensing Georg, Voith Barbara, Zuehlsdorf Michael. Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939--an oral, direct Factor Xa inhibitor--after multiple dosing in healthy male subjects. Eur. J. Clin. Pharmacol. 2005 Dec;61 (12):873–80. doi: 10.1007/s00228-005-0043-5. [DOI] [PubMed] [Google Scholar]
- 14.Kubitza Dagmar, Becka Michael, Zuehlsdorf Michael, Mueck Wolfgang. Effect of food, an antacid, and the H2 antagonist ranitidine on the absorption of BAY 59-7939 (rivaroxaban), an oral, direct factor Xa inhibitor, in healthy subjects. J Clin Pharmacol. 2006 May;46 (5):549–58. doi: 10.1177/0091270006286904. [DOI] [PubMed] [Google Scholar]
- 15.Kubitza Dagmar, Becka Michael, Roth Angelika, Mueck Wolfgang. Dose-escalation study of the pharmacokinetics and pharmacodynamics of rivaroxaban in healthy elderly subjects. Curr Med Res Opin. 2008 Oct;24 (10):2757–65. doi: 10.1185/03007990802361499. [DOI] [PubMed] [Google Scholar]
- 16.Mannucci Pier M, Schutgens Roger E G, Santagostino Elena, Mauser-Bunschoten Evelien P. How I treat age-related morbidities in elderly persons with hemophilia. Blood. 2009 Dec 17;114 (26):5256–63. doi: 10.1182/blood-2009-07-215665. [DOI] [PubMed] [Google Scholar]
- 17.Zimmermann Rainer, Staritz Peter, Huth-Kühne Angela. Challenges in treating elderly patients with haemophilia: a focus on cardiology. Thromb. Res. 2014 Nov;134 Suppl 1 ():S48–52. doi: 10.1016/j.thromres.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 18.Humphries Thomas J, Rule Brittny, Ogbonnaya Augustina, Eaddy Michael, Lunacsek Orsolya, Lamerato Lois, Pocoski Jennifer. Cardiovascular comorbidities in a United States patient population with hemophilia A: A comprehensive chart review. Adv Med Sci. 2018 Sep;63 (2):329–333. doi: 10.1016/j.advms.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 19.de Raucourt Emmanuelle, Roussel-Robert Valérie, Zetterberg Eva. Prevention and treatment of atherosclerosis in haemophilia - how to balance risk of bleeding with risk of ischaemic events. Eur. J. Haematol. 2015 Feb;94 Suppl 77 ():23–9. doi: 10.1111/ejh.12498. [DOI] [PubMed] [Google Scholar]
- 20.Murray Nigel P, Muñoz Lorena, Minzer Simona, Lopez Marco Antonio. Management of Thrombosis Risk in a Carrier of Hemophilia A with Low Factor VIII Levels with Atrial Fibrillation: A Clinical Case and Literature Review. Case Rep Hematol. 2018;2018 () doi: 10.1155/2018/2615838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferraris Victor A, Boral Leonard I, Cohen Alice J, Smyth Susan S, White Gilbert C. Consensus review of the treatment of cardiovascular disease in people with hemophilia A and B. Cardiol Rev. 2014 Dec 2;23 (2):53–68. doi: 10.1097/CRD.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schutgens Roger E G, van der Heijden Jeroen F, Mauser-Bunschoten Eveline P, Mannucci Pier M. New concepts for anticoagulant therapy in persons with hemophilia. Blood. 2016 Nov 17;128 (20):2471–2474. doi: 10.1182/blood-2016-07-727032. [DOI] [PubMed] [Google Scholar]
- 23.Martin Karlyn, Key Nigel S. How I treat patients with inherited bleeding disorders who need anticoagulant therapy. Blood. 2016 Jul 14;128 (2):178–84. doi: 10.1182/blood-2015-12-635094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dimichele D, Négrier C. A retrospective postlicensure survey of FEIBA efficacy and safety. Haemophilia. 2006 Jul;12 (4):352–62. doi: 10.1111/j.1365-2516.2006.01284.x. [DOI] [PubMed] [Google Scholar]
- 25.Astermark Jan, Donfield Sharyne M, DiMichele Donna M, Gringeri Alessandro, Gilbert Steven A, Waters Jennifer, Berntorp Erik. A randomized comparison of bypassing agents in hemophilia complicated by an inhibitor: the FEIBA NovoSeven Comparative (FENOC) Study. Blood. 2007 Jan 15;109 (2):546–51. doi: 10.1182/blood-2006-04-017988. [DOI] [PubMed] [Google Scholar]
- 26.de Koning M L Y, Fischer K, de Laat B, Huisman A, Ninivaggi M, Schutgens R E G. Comparing thrombin generation in patients with hemophilia A and patients on vitamin K antagonists. J. Thromb. Haemost. 2017 May;15 (5):868–875. doi: 10.1111/jth.13674. [DOI] [PubMed] [Google Scholar]
- 27.Lip Gregory Y H, Larsen Torben Bjerregaard, Skjøth Flemming, Rasmussen Lars Hvilsted. Indirect comparisons of new oral anticoagulant drugs for efficacy and safety when used for stroke prevention in atrial fibrillation. J. Am. Coll. Cardiol. 2012 Aug 21;60 (8):738–46. doi: 10.1016/j.jacc.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 28.Milling Truman J, Kaatz Scott. Preclinical and Clinical Data for Factor Xa and "Universal" Reversal Agents. Am. J. Med. 2016 Nov;129 (11S):S80–S88. doi: 10.1016/j.amjmed.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee Hsin-Fu, Chan Yi-Hsin, Tu Hui-Tzu, Kuo Chi-Tai, Yeh Yung-Hsin, Chang Shang-Hung, Wu Lung-Sheng, See Lai-Chu. The effectiveness and safety of low-dose rivaroxaban in Asians with non-valvular atrial fibrillation. Int. J. Cardiol. 2018 Jun 15;261 ():78–83. doi: 10.1016/j.ijcard.2018.03.063. [DOI] [PubMed] [Google Scholar]
- 30.Hankey Graeme J. Intracranial hemorrhage and novel anticoagulants for atrial fibrillation: what have we learned? Curr Cardiol Rep. 2014 May;16 (5) doi: 10.1007/s11886-014-0480-9. [DOI] [PubMed] [Google Scholar]
- 31.Budnitz Daniel S, Lovegrove Maribeth C, Shehab Nadine, Richards Chesley L. Emergency hospitalizations for adverse drug events in older Americans. N. Engl. J. Med. 2011 Nov 24;365 (21):2002–12. doi: 10.1056/NEJMsa1103053. [DOI] [PubMed] [Google Scholar]
- 32.Diener H-C, Halperin J L, Fox K, Hankey G J. Stroke prevention with rivaroxaban in higher-risk populations with atrial fibrillation. Int. J. Clin. Pract. 2015 Jul;69 (7):743–56. doi: 10.1111/ijcp.12631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ikeda Takanori, Atarashi Hirotsugu, Inoue Hiroshi, Uchiyama Shinichiro, Kitazono Takanari, Yamashita Takeshi, Shimizu Wataru, Kamouchi Masahiro, Kaikita Koichi, Fukuda Koji, Origasa Hideki, Sakuma Ichiro, Saku Keijiro, Okumura Yasuo, Nakamura Yuichiro, Morimoto Hideo, Matsumoto Naoki, Tsuchida Akihito, Ako Junya, Sugishita Nobuyoshi, Shimizu Shogo, Shimokawa Hiroaki. Study Design and Baseline Characteristics of the EXPAND Study: Evaluation of Effectiveness and Safety of Xa Inhibitor, Rivaroxaban for the Prevention of Stroke and Systemic Embolism in a Nationwide Cohort of Japanese Patients Diagnosed as Non-Valvular Atrial Fibrillation. Tohoku J. Exp. Med. 2016 Dec;240 (4):259–268. doi: 10.1620/tjem.240.259. [DOI] [PubMed] [Google Scholar]
- 34.Connolly Stuart J, Eikelboom John, Joyner Campbell, Diener Hans-Christoph, Hart Robert, Golitsyn Sergey, Flaker Greg, Avezum Alvaro, Hohnloser Stefan H, Diaz Rafael, Talajic Mario, Zhu Jun, Pais Prem, Budaj Andrzej, Parkhomenko Alexander, Jansky Petr, Commerford Patrick, Tan Ru San, Sim Kui-Hian, Lewis Basil S, Van Mieghem Walter, Lip Gregory Y H, Kim Jae Hyung, Lanas-Zanetti Fernando, Gonzalez-Hermosillo Antonio, Dans Antonio L, Munawar Muhammad, O'Donnell Martin, Lawrence John, Lewis Gayle, Afzal Rizwan, Yusuf Salim. Apixaban in patients with atrial fibrillation. N. Engl. J. Med. 2011 Mar 03;364 (9):806–17. doi: 10.1056/NEJMoa1007432. [DOI] [PubMed] [Google Scholar]
- 35.Ruff Christian T, Giugliano Robert P, Braunwald Eugene, Hoffman Elaine B, Deenadayalu Naveen, Ezekowitz Michael D, Camm A John, Weitz Jeffrey I, Lewis Basil S, Parkhomenko Alexander, Yamashita Takeshi, Antman Elliott M. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014 Mar 15;383 (9921):955–62. doi: 10.1016/S0140-6736(13)62343-0. [DOI] [PubMed] [Google Scholar]
- 36.Andreotti Felicita, Rocca Bianca, Husted Steen, Ajjan Ramzi A, ten Berg Jurrien, Cattaneo Marco, Collet Jean-Philippe, De Caterina Raffaele, Fox Keith A A, Halvorsen Sigrun, Huber Kurt, Hylek Elaine M, Lip Gregory Y H, Montalescot Gilles, Morais Joao, Patrono Carlo, Verheugt Freek W A, Wallentin Lars, Weiss Thomas W, Storey Robert F. Antithrombotic therapy in the elderly: expert position paper of the European Society of Cardiology Working Group on Thrombosis. Eur. Heart J. 2015 Dec 07;36 (46):3238–49. doi: 10.1093/eurheartj/ehv304. [DOI] [PubMed] [Google Scholar]
- 37.Villines Todd C, Ahmad Azhar, Petrini Michaela, Tang Wenbo, Evans Amber, Rush Toni, Thompson David, Oh Kelly, Schwartzman Eric. Comparative safety and effectiveness of dabigatran vs. rivaroxaban and apixaban in patients with non-valvular atrial fibrillation: a retrospective study from a large healthcare system. Eur Heart J Cardiovasc Pharmacother. 2019 Apr 01;5 (2):80–90. doi: 10.1093/ehjcvp/pvy044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graham David J, Reichman Marsha E, Wernecke Michael, Hsueh Ya-Hui, Izem Rima, Southworth Mary Ross, Wei Yuqin, Liao Jiemin, Goulding Margie R, Mott Katrina, Chillarige Yoganand, MaCurdy Thomas E, Worrall Chris, Kelman Jeffrey A. Stroke, Bleeding, and Mortality Risks in Elderly Medicare Beneficiaries Treated With Dabigatran or Rivaroxaban for Nonvalvular Atrial Fibrillation. JAMA Intern Med. 2016 Nov 01;176 (11):1662–1671. doi: 10.1001/jamainternmed.2016.5954. [DOI] [PubMed] [Google Scholar]
- 39.Li Guowei, Lip Gregory Y H, Holbrook Anne, Chang Yaping, Larsen Torben B, Sun Xin, Tang Jie, Mbuagbaw Lawrence, Witt Daniel M, Crowther Mark, Thabane Lehana, Levine Mitchell A H. Direct comparative effectiveness and safety between non-vitamin K antagonist oral anticoagulants for stroke prevention in nonvalvular atrial fibrillation: a systematic review and meta-analysis of observational studies. Eur. J. Epidemiol. 2019 Feb;34 (2):173–190. doi: 10.1007/s10654-018-0415-7. [DOI] [PubMed] [Google Scholar]
- 40.Providência Rui, Grove Erik Lerkevang, Husted Steen, Barra Sérgio, Boveda Serge, Morais João. A meta-analysis of phase III randomized controlled trials with novel oral anticoagulants in atrial fibrillation: comparisons between direct thrombin inhibitors vs. factor Xa inhibitors and different dosing regimens. Thromb. Res. 2014 Dec;134 (6):1253–64. doi: 10.1016/j.thromres.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 41.Gremmel Thomas, Niessner Alexander, Domanovits Hans, Frossard Martin, Sengölge Gürkan, Steinlechner Barbara, Sycha Thomas, Wolzt Michael, Pabinger Ingrid. Non-vitamin K antagonist oral anticoagulants in patients with an increased risk of bleeding. Wien. Klin. Wochenschr. 2018 Dec;130 (23-24):722–734. doi: 10.1007/s00508-018-1381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reddy Vivek Y, Doshi Shephal K, Kar Saibal, Gibson Douglas N, Price Matthew J, Huber Kenneth, Horton Rodney P, Buchbinder Maurice, Neuzil Petr, Gordon Nicole T, Holmes David R. 5-Year Outcomes After Left Atrial Appendage Closure: From the PREVAIL and PROTECT AF Trials. J. Am. Coll. Cardiol. 2017 Dec 19;70 (24):2964–2975. doi: 10.1016/j.jacc.2017.10.021. [DOI] [PubMed] [Google Scholar]