Abstract
Catheter ablation is increasingly performed for treatment of atrial fibrillation (AF). Balloon based procedures have been developed aiming at safer, easier and more effective treatment as compared to point to point ablation. In the present review article, we aimed to discuss acute procedural complications of cryoballoon ablation.
Keywords: Atrial fibrillation, Atrio-oesophageal fistula, Bronchial injury, Catheter ablation, Cryoablation, Cryoballoon, Phrenic nerve injury
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained arrhythmia in Europe and U.S [1,2]. Despite promising improvements in the management of patients with AF, this arrhythmia remains one of the leading causes of stroke, heart failure, sudden death, and cardiovascular morbidity [3]. Once the demonstration of that the pulmonary veins (PVs) and also non-PV triggers initiates AF, catheter ablation has developed as gold standard method in selected population of patients for AF treatment [4]. CABANA trial tested whether primary catheter ablation for the elimination of AF was superior to state-of-the-art drug therapy and demonstrated that ablation is a safe and effective therapy for AF and, in some cases, is superior to drug therapy [5]. Pulmonary vein isolation (PVI) is now widely accepted as the cornerstone of AF ablation procedures. Radiofrequency based ablation techniques try to achieve this goal by "point by point" ablation; however, in the last years, the use of novel alternative ablation strategies such as cryoballoon (CB) or laserballoon is growing rapidly [6-8]. As expected, CB ablation is related to a significantly had a shorter procedure time and a non-significantly shorter fluoroscopy time compared with radiofrequency catheter ablation because the single or just a couple bonus applications are adequate for durable and complete lesions [6,7,9]. Cryoballoon ablation technique as a single shot deviece also provides acceptable success rates in complex AF substrates such as; persistent AF, elderly patients, patients with PV abnormalities and even in patients with heart failure [10-14]. With its relatively short learning curve, use of CB has been increased. And the possible concern about the efficacy and safety of the procedure in relatively low-volume centers may be raising. Good news is that, experience does not influence long-term outcome and peri-procedural complications after cryoballoon ablation of paroxysmal AF patients [15]. In the present article, we try to comprehensively review acute procedural complications associated with CB ablation.
DEFINITION AND CLASSIFICATION
By definition, peri-procedural complications and complications occurring within the first 24 hours denote as acute complications. Ablation-related complications can be classified into following 4 groups according to their severity: (1) life-threatening complications; (2) severe complications; (3) moderate or minor complications; and (4) complications with unknown significance [3]. Simply, potentially fatal complications such as esophageal injury, cardiac tamponade, and periprocedural stroke are classified as life-threatening complications. Although the definition of serious complication is unclear, when life-threatening complications are removed, it seems to state the same as the definition of major complication used in previous studies. According to this classification, PV stenosis, persistent phrenic nerve palsy (PNP), vascular complications requiring transfusion or surgical intervention, and other rare complications such as mitral valve damage, cardiac conduction system damage requiring pacemaker implantation, and myocardial infarction are called as severe complications. However, there are some limitations related to this classification method. A moderate or minor complication such as femoral hematoma may convert a major complication during the course of the illnes, when it requires transfusion or surgical intervention. Contrary, most patients with significant PV stenosis and persistent PNP remain asymptomatic or have few symptoms [16,17].
In the rest of the article, acute procedural complications of CB ablation will discuss according to place of occurrence.
COMPLICATIONS RELATED TO VASCULAR ACCESS SITE
Peripheral vascular complications are the most common complications of AF ablation regardles of used energy type [18]. The complications consist of bleeding, groin or retroperitoneal hematomas, pseudoaneurysms, arteriovenous fistulas, arterial thromboembolism, and arterial air embolism which are cumulatively reported in about 1-2% of cases [19,20]. Theoratically, the risk of access site bleeding should be more during ablation of AF than other cardiac arrhythmias due to peri-procedural anticoagulation requirement. Fortunately, the study results did not confirm this assumption and periprocedural uninterrupted oral anticoagulation therapy was found to be associated with more effective for preventing thromboembolism without any increase in incidence of bleeding complications [20,21]. Furthermore, under uninterrupted warfarine regimen with a therapeutic INR was associated with lower minor bleeding complications than bridging with heparin or LMWH [22]. During CB application, use of a special calibre delivery sheath (FlexCath Advance® Steerable Sheath, Medtronic Inc. ) is needed. The sheath has a wide 12F inner and 15F outer diameters, respectively. This may be accepted as a potentially enhancing factor for the risk of vascular complications. However, larger size of the sheath does not seem to cause a serious problem in that case because the sheath is advanced via venous system. In the relevant literature, the similar vascular complication rates between CB and radiofrequency ablation confirms this reasoning [18,19].
The studies for radiofrequency ablation demonstrated that risk of vascular complications may be increased with female gender, older age, and less experienced operators [24,25]. Although similar factors were studied for CB, only female gender was found related to higher vascular complications [25,27]. Theoretically, a higher proportion of vascular access site complication in women might be associated with more, increased body mass index, more sensitive connective tissue and vascular wall or variable femoral veincourse in this population. In a Russian pilot survey, Mikhaylov et al [25] compared AF ablation results between high- and low-volume AF ablation centres. Surprisingly, a higher proportion of vascular access-site complications occured in high-volume AF ablation centres. As a potential explanation, they speculated that, in the lower-volume AF ablation centres, venous access was performed by well experienced vascular puncture operators whereas the higher-volume centres were mainly academic teaching centres, where preparations for ablation procedures were carried out by younger fellow physicians. Therefore, it should be kept in mind that operator experience is more important than volume of center to predict periferic vascular complications.
Arterial pseudoaneurysms are related to inadvertent punctures of the neighboring femoral artery during puncture of femoral vein. Mugnai et al [28] reported incidence of complications in those patients who underwent CBA for AF and the impact of novel oral anticoagulants on adverse events compared with vitamin K antagonists. The incidence of femoral pseudoaneurysms was 1.3%; 1 patient required surgical repair; 1 patient underwent percutaneous thrombin injection due to a false aneurysm; and the other 3 patients were successfully treated conservatively by compression only. Although there is no data related to CBA, ultrasound guidance during femoral puncture may be suggested to reduce this complications [29].
The great majority of bleeding and hematomas resolve spontaneously and are classified as minor complication. Any bleeding severe enough to require a blood transfusion or hematomas requiring surgical intervention is called as major bleeding and encountered in up to 1.5% of cases [30]. Arteriovenous fistula is a rare complication and should be treated surgically.
Despite various precautions to achieve complete hemostasis in a safe and effective manner, no standard approach or technique is available yet. Device-based invasive vascular closure techniques have significant cost with a risk of device failure and specific vascular complications [31]. Despite, modified figure-of-eight suture for femoral venous hemostasis has been found to be safe and time saving hemostasis method for CB procedures [32], manual compression is the most commonly used technique to achieve access site hemostasis after CB procedure. Protamine reversal of anticoagulation may be an option for veinous hemostasis during manual compression. Gurses et al.[33] studied safety and efficacy of protamine administration for reversal of heparin with manuel compression following CBA. Hospital stay was significantly shorter in patients who were administered protamine. Furthermore, all hematoma, pseudoaneurysm and arteriovenous fistula requiring surgical or interventional repair in the femoral access site were lower in patients who received protamine (1.1 %) than patients who did not (6.3%) (p = 0.011). In our clinic we routinely use manual compression without heparine reversal and major hematoma requiring intervention was detected in one case (2.1%) [34].
COMPLICATIONS RELATED TO TRANSSEPTAL PUNCTURE
AF ablation procedure requires transseptal puncture (TSP). In routine approach, Brockenbrough needles are used with a wide variety of sheaths to access the left atrium (LA). To understand complications related to TSP, it should be kept in mind that interatrial septum (IAS) is bordered by the ostia of the inferior vena cava, superior vena cava, coronary sinus, tricuspid septal leaflet, right atrial appendage and posterior wall folds. Therefore, only 20% of total septal area is suitable to be crossed without exiting the heart [35].
Cardiac perforation with or without tamponade is the most common acute procedural life threatening complication of TSP. The main cause is inadvertent penetration of the posterior segments. Less commonly, left atrial lateral wall, left atrial roof or left atrial appendage (LAA) may be damaged due to sudden jumping of needle across the IAS [36]. TSP guided only by fluoroscopy is complicated by tamponade in 0.1–3.2% of cases [37]. ICE or TEE provided direct visualization of the septum may offer a safer TSP, especially in atypical anatomy, a resistant/elastic septum and inexperienced operators [38-40]. As demonstrated in our recently published article, a simple deep inspiration maneuver during TSP may be a reliable and safe method after failed conventional attempts in some of these cases [41]. However, it should be kept in mind that the need for multiple punctures and intraprocedural systemic/ongoing oral anticoagulation may increase the risk or aggravate the consequences of complications. In the presence of hypotension, diaphoresis, sinus tachycardia or asystole, cardiac tamponade should be taken into account, immediately. Although the diagnosis is easily confirmed by transthoracic echocardiography, fluoroscopic reduction in the excursion of cardiac silhouette on fluoroscopy is an early diagnostic sign of cardiac tamponade during the procedure and may be used to detect impending pericardial tamponade before hemodynamic collapse [42]. Once perforation or tamponade is detected, the effect of anticoagulants (heparin or oral anticoagulant) should be reversed by using proper reversal agent such as protamine, four-factor prothrombin complex concentrate rather than fresh frozen plasma, idarucizumab, andexanet alpha or recombinant factor VIIa in addition to fluid administration [43,44]. If tamponade does not resolve with these precautions, the patient should prepare for immediate pericardiocenthesis with autologous transfusion without wasting time. Urgent cardiac surgery should be attempted in case of continuos bleeding [45].
Due to large outer diameter of the FlexCath catheter the rate of iatrogenic atrial septal defect (ASD) may be high up to 38% at 6 months, with a mean size of 5.5 mm [46]. The incidence of iatrogenic ASD has been found significantly higher in CBA compared to double transseptal conventional radiofrequency ablation.[47]. Despite hemodinamically significant iatrogenic ASD has been reported previously [48], in the majority of the cases this complication is not clinically relevant and mostly does not cause any adverse events not only in acute period but also during the follow-up. Transient inferior ST-segment elevation accompanied by profound hypotension and bradycardia has been reported in 0.3% of cases [49]. The most plausible mechanism of this phenomenon is Bezold-Jarisch–like vasovagal responsedue to the mechanical effects of puncture on the vagal network located close to the puncture site. This vagal network usually innervates the right coronary artery and leaves it vulnerable to cholinergic vasospasm [50]. However coronary embolism should be kept in mind as an alternative diagnosis in all cases. If the cause is vagal hyperactivity, it usually resolves spontaneously. In rare situations, dopamine or fast saline drip can resolve the problem without sequelae or other complications [49].
Peripheral or central embolism including silent microemboli, transient ischemic attack and stroke is usually caused by thrombus formation in the space between the needle and the dilator, if proper anticoagulation is not administered prior to or immediately following TSP. Once the TSP system reaches the LA, ACT of at least 300-350 seconds with intravenous heparin should be achieved and maintained until all the catheters are removed from the LA. According to the latest expert consensus statement on catheter and surgical ablation of AF, uninterrupted oral anticoagulation regimen is recommended with VKAs or NOACs in addition to intraprocedural heparin infusion [4].
Air embolism to the systemic circulation is another important complication during TSP. Recurrent catheter exchanges and rapid removal of catheters or dilators, deep sedation and prolonged apnea periods with deep breaths during general anesthesia, and incomplete hemostasis valves are the most commonly reported causes of air embolism [51]. All these causes inadvertent negative pressure in catheter lumen or in the LA and air passage into the left hear chamber. To avoid this devastating complication, usage of a continuous flush through a closed system is mandatory. Also, the wire and dilators should be withdrawn from the catheter gradually. Also, the syringe should be held upright during hand injections. Once the complication is happening, the target should be to prevent further air entry, reduce the volume of the air embolus, and provide haemodynamic support. Administration of high-flow oxygen therapy is usually suggested to accelerate reabsorption of the air and minimize the size of the air bubble [52]. In a recently published article, Cay et al [53] presented a case of massive coronary air embolism and discussed its acute management. Excange of large diameter FlexCath with thinner transseptal sheath, aspiration of the air through coronary artery by an aspiration catheter solved the problem in their case. Then, full patency of the vessel and complete resolution of ST segment elevations was achieved after multiple rapid suctions through the catheter. Aortic root injury is a rare complication of TSP due to penetration of the anterior segments. Proper usage of fluoroscopy, transesophageal or intracardiac echocardiography is mandatory to avoid inadvertent aortic root needle puncture. Also, contrast injection and pressure recording after the needle has been passed septum may facilitate to recognize aortic puncture before advancing the sheath. In case of aortic puncture with needle, withdrawing of the needle slowly is reported to be safe and effective strategy [54]. If the sheath entered the aorta, the sheath should be pulled back with a wire left in the aorta in the presence of surgical standby. Once ensuring hemodynamic stabilization, the wire may also be pulled back. Careful haemodynamic and echocardiographic observation is mandatory during all these steps. Gerbode defect is a rare congenital anomaly that permits shunting from the left ventricle to the right atrium [55]. Preprocedural evaluation of IAS with echocardiography is important in terms of uncovering existence of this defect because it may cause inadvertent aortic root puncture.
COMPLICATIONS DURING ABLATION
Pericardial effusion is a relatively common complication of CB ablation. In a recently published study, mild and moderate pericardial effusion was detected in 78% of patients undergoing CB ablation [56]. Although the incidence of cardiac tamponade has been reported to be higher with radiofrequency energy, the incidence of pericardial effusion were similar in both energy types [57,58]. Acute pericarditis is another pericardial complication of CB ablation and may occurr in up to 4% of patients [56]. The total number of cryoapplications and the total freeze duration were significantly higher in patients with pericarditis compared with those without. In patients demonstrating altering findings such as low blood pressure, tachycardia, and narrowed pulse pressure, a transthoracic echocardiography should be performed without wasting time. Becasue the approach in cardiac tamponade is described in detail in the above section; it is not mentioned again, here.
Although published complication rates of CB2 based-PVI are relatively low and several safety algorithms have been implemented in the protocols the most frequent complication is right-sided phrenic nerve injury (PNI). PNI develops due to the close proximity to the PNs with the PVs. Although the incidence of PNI has decreased over the years due to advanced balloon and improved techniques for early detection, PNI was noted in 3.2%-7% of patients [59,60]. High incidence of PNI after CB ablation is related to close anatomical relationship between the PNs and PV anatomy. The right PN descends posteriorly in between the right PVs and the superior vena cava–right atrial junction. Sánchez-Quintana et al [61] studied by gross dissection the courses of the right and left PNs in 6 cadavers and demonstrated that the distance between the right PN and the anterior wall of the right superior PV may be as few as 2.1±0.4 mm whereas the distance with the right inferior PV is higher (7.8 mm±1.2). As an expected result of this close proximity, the risk of PNI is highest during ablation of the right superior PV [62] however, it is not clear why PNI appears to be more common with CB compared with radiofrequency ablation [63]. One suggested mechanism implicates anatomic distortion of the PV orifice/PN relationship, through increasing contact or shortening the relative distance between the ablation site and the PN, even without displacement of the balloon into the PV [64].
Although the left PN courses anteriorly across the LAA and is far from the left PVs, there are published cases of left PNI during CB ablation of the left superior PV [65,66]. The risk may be higher during isolation of the LAA by using CB [67]. Despite this general acceptance, the incidence and prognosis of left-sided PNI during CB ablation was recently evaluated by recording the amplitude of the compound motor action potentials during the CB ablation. Premature termination of the freezing was required to avoid PNP in 1.8% of patients [68].
Following pre-operative computed tomography findings have been associated with the development of PNI: (1) shorter distance between the right superior PV and right PN; (2) larger PV dimensions; (3) Larger external angle between the right superior PV and right anterolateral wall of the LA; and (4) smaller eccentricity index (ratio of maximum over minimum ostial diameter). In a recently published study, the prevalence of right common ostium and temperature drop velocity from basal to - 20 °C were found as predictors of PNI in the multivariate analysis [69].
Additionally, type of CB has also an impact on possibility of PNI. Comparison of first and second generation of CB ablation showed significantly larger number of reversible and persistent PNI with the second-generation CB [70,71].
The CB ablation protocol may influence the incidence of PNI. Rottner and coworkers studied to to assess the impact of different ablation protocols on the incidence and characteristics of procedural complications. Time-to effect protocol was found to be safe and effective. The observed difference in the occurrence of procedural complications between the ablation protocols is mainly driven by the higher incidence of PNI in bonus freeze and no-Bonus freeze arm. However, distinctive risk factors for the occurrence of procedural complications could not identified, lower number and shorter length of the applied freeze-cycles in the 'time-to-effect' protocol could possibly explain the low incidence of PNI [72].
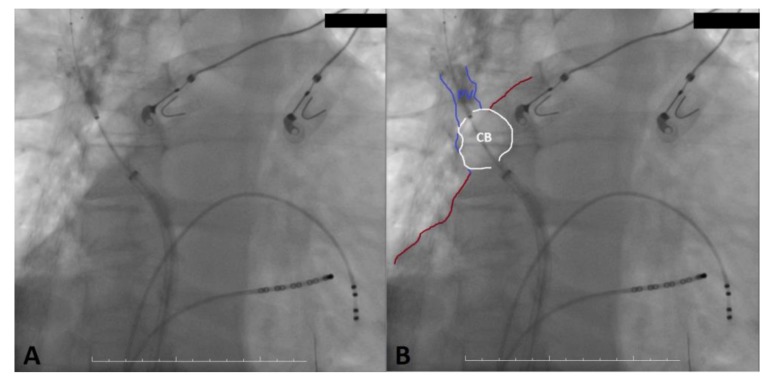
The diagnosis of PNI is usually made with evidence of diaphragmatic elevation at the chest X-ray or a paradox diaphragmatic movement in the fluoroscopy in a patient demonstrating complaints such as dyspnea, cough, or hiccups. To diagnose during CB ablation, anciently, the PN function was evaluated by direct visulation of diaphragmatic motion on fluoroscopy; however, it is the least optimal method as it exposes the patient and operator to additional radiation and may delay the diagnosis ([Figure 1], movie 1-2). As a second method, the PN function may be evaluated by manual palpation of the patient's abdomen to monitor the excursion of the right hemidiaphragm during high amplitude pacing from the superior vena cava (Movie 3). Weakening of the diaphragmatic motion can indicate PNI. This method is easily applicable but the subjectivity associated with the measurement and respiratory variations in the diaphragmatic contraction strength can be mistaken as PNI. To provide earlier warning of PNI, novel techniques utilizing diaphragmatic compound motor action potential (CMAP) has been recently developped [73,74]. During ablation of the right-sided PVs, CMAP recordings were obtained using two leads: a standard surface right arm ECG electrode positioned 5 cm above the xiphoid and a left arm ECG electrode positioned 16 cm along the right costal margin. The PN is paced continuously with high-output during CB application. A decrease in CMAP amplitude by 35% from baseline may predict and prevent PNI [73].
Figure 1. Deep settlement of cryoballoon catheter is seen on fluroscopy. To facilitate demonstration of catheter position and shape borders of cryoballoon, the right superior pulmonary vein, and the left atrium was drawn with White, blue, and red lines, respectively (B).
Once the suspicion of PNI is determined by one of the methods described above, immediate termination of cryoenergy is the cornerstone of the prevention. If the PN function returns immediately, another CB application may attempt with condition more antral position of the balloon to be confirmed. Otherwise, ablation should be continued with radiofrequency energy. Prognosis of PNI after CBA has been investigated in a large YETI registry [74]. a total of 13693 patients received CB2 or CB3 based-PVI in 23 EP centers. A total of 596 (4.4%) of patients experienced PNI during treatment of the right superior (84%) right inferior (15%) right middle (0.3%) (and left superior (0.3%) pulmonary veins. After 1-3 months 18% of patients showed persistent PNI including 13% of patients complaining of dyspnea. After 6-12 months of follow-up including fluoroscopic evaluation PNI was persistent in 1.8% of patients while dyspnea was reported by 1.7% patients. Only 0.08% of the overall population of 13693 patients showed permanent and symptomatic PNI.
Bronchial injury is a less defined but potentially serious complication of CB ablation. While the most obvious finding is haemoptysis, cough or dyspnea may be the only complaint [75-77]. Persistent cough was reported as high as 17% in the STOP-AF Trial, and hemoptysis has been reported in 1% of cases in the cryoballoon STOP-AF Post Approval Study [75,76]. Unfortunately, the exact cause of this complication is uncertain. Although collateral thermal injury of the bronchial tree is the most widely accepted mechanism of haemoptysis, it might be related to pulmonary infarct, pulmonary haemorrhage or PV stenosis [77-79]. Also, direct damage to the tissue surrounding the PN or deeper inside the lung could be caused by catheterizing it with the guide wire or by distal inflation of the balloon. High-resolution computed tomography of the chest should be used to diagnose [Figure 2]. There is no well accepted treatment option for these cases. Although some groups suggest reversal of anticoagulation and urgent bronchoscopy, haemoptysis usually resolves spontaneously and does not reoccur after restarting anticoagulation theraphy [78-81].
Figure 2. A The computed tomography scan of the chest demonstrates the consolidation in the left lower lobe at the superior boundary suggestive of a pulmonary haemorrhage. B Complete resolution of pulmonary haemorrhage is seen in control computed tomography 1 month later.
Table 1. Complications of CBA.
| Complication | Mechanism | Incidence | Management | How to avoid |
|---|---|---|---|---|
| Vascular Access site: Inguinal bleeding, hematoma, pseudoaneurism, atriovenous fistula, arterial thromboembolism, arterial air embolism | Vascular damage, inadequate hemostasis, inadvertent puncture, inadequate anticoagulation | 1-2% More common in women, elderly pts, less experienced operators, high volume centers | Conservative compression, thrombin injection, surgery for pseudoaneurism, Most hematomas resolve spontaneously Surgery for AV fistula | USG guidance during puncture, Protamine reversal, figure of eight suture for hemostasis |
| Cardiac perforation | During TSP inadvertent posterior segment penetration, LAA, LA lateral wall injury, Aortic root injury | 0.1%-3.2% | Heparine reversal, fluids, pericardiocentesis, surgery, if the sheath advanced to aorta surgery is generally needed. | ICE/TEE guidance, Deep inspiration maneuver |
| Iatrogenic ASD | Thick transseptal sheath | 38% at 6 months | Mostly clinical nonrelevant | - |
| Transient ST elevation | Mostly Besold Jarich like reflex, Coronary embolism | 0.3% | Coronary angiogram, Dopamine, fast saline drip | Proper anticoagulation, 300-500 ACT, uninterrupted anticoagulation |
| Air embolism | Recurrent catheter change, rapid catheter removal, deep sedation, deep breathing, incomplete hemostatic valves | Recurrent catheter change, rapid catheter removal, deep sedation, deep breathing, incomplete hemostatic valves | Positioning, high pressure O2, hemodynamic support, air aspiration | Proper anticoagulation, 300-500 ACT, uninterrupted anticoagulation, removal of air bubbles from catheter |
| TIA, Stroke | Mostly due to air embolism | Silent cerebral lesions common, clinical TIA/Stroke less than %1 | Anticoagulation, consider neurology consultation | Proper anticoagulation, 300-500 ACT, uninterrupted anticoagulation, removal of air bubbles from catheter |
| PNI | Anatomical relationship between right sided veins and right PN Anatomical relationship between LAA and left PN | 3.2-7% | Diagnosed by fluoroscopic evaluation 1-3 days 35% recovery 1-3 months 18% recovery 0.018% persistent and symptomatic | Operator hand control CMAP |
| Bronchial injury hemoptisis | Thermal trauma, Catheter injury | rare | Reverse anticoagulation, mostly recurs | Avoid lower freezing temperature |
| Gastroparesis, esophageal injury | Periesophageal plexus or esophageal thermal injury | Gastroparesis mostly during inferior sided vein application with large balloon in small LA | Use temperature probe | |
| PV stenosis | Large PV ostia, low freezing temperature | rare | PV angioplasty, surgery | Avoid low freezing temperature |
| AV block | Very rare | Careful rhythm control | - | |
| Cx arterial vasosplasm | During LAA isolation | Very rare | ECG ST elevation | - |
| Achieve catheter breakage | Mechanical | Very rare |
Atrioesophageal fistula due to direct esophageal injury has been reported as anecdotal case reports after CB ablation [82,83]. Thus, knowledge about the clinical findings and the clinical course of the disease is derived from ablation studies using radiofrequency energy. It usually occurs within 1-4 weeks following ablation procedure with non-specific signs and symptoms such as fever, fatigue, malaise, chest discomfort, nausea, vomiting, dysphagia, odynophagia, hematemesis, melena, and dyspnea. Because the current article is dedicated to inform about acute complications of CB ablation, atrioesophageal fistula will not discuss in detail. But, in patients presenting with infection findings without a clear focus, retrosternal pain, and cerebrovascular findings, the diagnosis should be considered. The esophageal effects of CB have been studied by different groups by using endoscopy. Lower freezing temparature and lower average minimal luminal esophageal temperature was found related to higher esophageal effects and gastrointestinal complaints [84-89].
Although efficacy real-time luminal esophageal temperature monitoring by placing a temperature probe into the esophagus has not been investigated for CB ablation, the data from radiofrequency ablation suggests that it may be successful to detect a decrease in luminal esophageal temperature. There is no other well defined prevention strategy for this complication.
Gastroparesis is a relatively common but little known complications of CB ablation. The most possible mechanism of gastroparesis related with AF ablation is collateral periesophageal vagal nevre injury. Gastroparesis has been reported mostly occurring during CBA in inferior PVs with relatively larger balloon in small LA [90].
The diagnosis should be considered in the present of following symptoms: epigastric discomfort, abdominal pain, heartburn, bloating, nausea, or vomiting during the procedure. As it demonstrated in our report, all symptomatic patients may be evaluated by fluoroscopy for an air-filled stomach or air fluid level in the fundus of an enlarged fluid-filled stomach [Figure 3] [90]. The patients showing these scopical findings should evaluated by gastric emptying scintigraphy (GES) to confirm the diagnosis. Although the FIRE AND ICE trial reported no instance of gastroparesis, the ratio of patients reporting symptoms that are shared with gastroparesis (abdominal pain, diabetic gastroparesis, epigastric discomfort, gastritis, impaired gastric emptying, nausea, and vomiting) was 3.2% for CB ablation and 2.1% radiofrequency ablation, respectively [91]. However, in our study gastroparesis was higher with CB ablation. Fortunately, gastroparesis had a good prognosis and resolving in all patients who received CB ablation [90].
Figure 3. Fluoroscopy demonstrates the stomach which is completely full of air.
Pulmonary vein stenosis (PVS) is a well defined and serious complication of point by point radiofrequency ablation. Evolving of ablation from osteal and segmental to wide area circumferential caused a decrease in the incidence of PVS from 20%-%30 to approximately 1% [92-95]. The incidence of PVS by CB ablation is approximately 3.1% after cryoablation with the first generation balloon [96]. The diagnosis should be considered in the patients demonstrating symptoms such as cough, dyspnea, chest pain, and hemoptysis. The severity of PV stenosis is generally defined as mild (<50%), moderate (50–70%) or severe (>70%), according to the percentage reduction of the luminal diameter and it determines the severity of the clinical presentation [97].
In recently published studies, a larger PV ostium, lower minimum freezing temperature, and an increased number of applications per vein during CB ablation were found as independent predictors of PVS [98,99]. Although cardiac computed tomography and magnetic resonance imaging are well defined imaging modalities to diagnose, acute edema and dissection-like changes on intravascular ultrasonography might be used for early diagnosis during the procedure [100]. Although there is no an effective treatment strategy, percutaneous balloon angioplasty alone or in conjuction with stent implantation might be a potential alternative in the acute setting. However, high restenosis rish should be kept in mind in long-term follow-up [101].
Peripheral or central embolism is one of the most devastating complications of CB ablation. Theoratically, cryoenergy should be related to lower incidence of thrombus formation because it causes lower platelet and fibrin activation by preserving the endothelial layer during ablation [102,103] whereas recent studies reported similar levels of platelet activity and coagulation activation by cryoenergy and radiofrequency energy [102]. Besides symptomatic cerebral events such as transient ischemic attack or stroke, AF ablation also carries a risk of silent cerebral embolic lesions. By using pre and post-procedural cerebral magnetic resonance imaging, different groups demonstrated that new embolic lesions might be detected in up to 10% of cases after radiofrequency ablation [104,105]. A similar finding was recently demonstrated for CB ablation by using real-time transcranial doppler monitoring [106]. To reduce the incidence of asymptomatic cerebral embolism during cryoablation, the removal of air bubbles from CB in heparinized saline water with extracorporeal balloon inflation before utilization was suggested by Tokuda et al [107].
Despite high rate of silent cerebral embolic lesions, the incidence of TIA or stroke has been reported lower than 1% [108]. To decrease thromboembolic complications of ablation, uninterrupted anticoagulation strategy should be preferred compared with bridging strategies using heparin or enoxaparin regardles of used anticoagulant agent [109,110]. To reveal the presence of thrombus formation in the LAA, routine usage of transesophageal echocardiography is recommended by some authors. Although the incidence of LAA thrombus before AF ablation is low (0.6% to 2%) in patients using uniterrupted anticoagulation or bridging with low-molecular-weight heparin, it should be kept in mind that it is not 0% [111,112]. In a recently published study, dual-source cardiac-computed tomography was succesfully used to exclude thrombus formation. As a main advantage of this new modality, it may deliver additional anatomic details of PVs and LA anatomy with an acceptable radiation exposure [113]. The diagnosis of acute brain lesion can be detected by high-resolution diffusion-weighted magnetic resonance imaging [Figure 4]. Once the diagnosis is confirmed, treatment of the disease should be maintained under the supervision of a neurologist.
Figure 4. Acute cortical infarcts within the left parietal lobe is seen on diffusion weighted cranial magnetic resonance imaging.
Transient ST-segment elevation during cryoballoon application due to coronary slow flow during CB application was firstly reported by our group [114]. During the first freezing attempt in the left superior PV, at 188 seconds and -48°C, an ST-segment elevation was observed in the V1 and V6 leads, without any complaint. Coronary artery angiography was performed less than 5 minutes after balloon deflation and revealed coronary slow flow without any significant flow-limiting lesion, coronary vasospasm, thromboembolus, or air embolus. The ST-segment elevation started to decrease within 3 minutes and returned to baseline in 14 minutes, without any intervention.
Breakage of the achieve circular mapping catheter in a the right PV was recently reported by Makimoto et al [115]. As a main cause of this unique complication, authors accused the wedged position of the catheter in PV, although they had felt no grating or resistance during catheter advencement. The circular part of catheter was remained and followed-up in the right PV without any complaint.
Canpolat et al [116] recently published a case with vasospasm at the proximal segment of the circumflex artery after CB application in the LAA due to close relationship between the LAA and the the circumflex artery. After administration of intracoronary nitrate, vasospasm was rapidly relieved.
Atrioventricular block is a rare complication of CB ablation [117,118]. Atrioventricular node ischemia is hypothesized as the most probable mechanism because coronary angiography performed 30 min after atrioventricular block demonstrated a patent atrioventricular node artery originating from the right coronary artery. In the case of Fedida et al, a short distance between the RIPV ostium and aortic annulus at proximity of the AV node region showed by CT-scan reconstruction could explain mechanical AV bock during manipulation of the 28 mm cryoballoon catheter. This could be due to mechanical bump of the IAS and crux cordis, but also to left sided pathway of the AV-node. Data for comparison with CT-scan reconstruction are needed to confirm this hypothesis.
Conclusion
Cryoablation has become a commonly used tool for the management of AF due to require less experience than radiofrequency ablation without affecting effectivity. However, it can lead to some significant and even fatal acute complications. Although the ratio of these complications are rare, operators should know how to detect and manage the complications, quickly.
References
- 1.Heeringa Jan, van der Kuip Deirdre A M, Hofman Albert, Kors Jan A, van Herpen Gerard, Stricker Bruno H Ch, Stijnen Theo, Lip Gregory Y H, Witteman Jacqueline C M. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur. Heart J. 2006 Apr;27 (8):949–53. doi: 10.1093/eurheartj/ehi825. [DOI] [PubMed] [Google Scholar]
- 2.Colilla Susan, Crow Ann, Petkun William, Singer Daniel E, Simon Teresa, Liu Xianchen. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am. J. Cardiol. 2013 Oct 15;112 (8):1142–7. doi: 10.1016/j.amjcard.2013.05.063. [DOI] [PubMed] [Google Scholar]
- 3.Kirchhof Paulus, Benussi Stefano, Kotecha Dipak, Ahlsson Anders, Atar Dan, Casadei Barbara, Castella Manuel, Diener Hans-Christoph, Heidbuchel Hein, Hendriks Jeroen, Hindricks Gerhard, Manolis Antonis S, Oldgren Jonas, Popescu Bogdan Alexandru, Schotten Ulrich, Van Putte Bart, Vardas Panagiotis, Agewall Stefan, Camm John, Baron Esquivias Gonzalo, Budts Werner, Carerj Scipione, Casselman Filip, Coca Antonio, De Caterina Raffaele, Deftereos Spiridon, Dobrev Dobromir, Ferro José M, Filippatos Gerasimos, Fitzsimons Donna, Gorenek Bulent, Guenoun Maxine, Hohnloser Stefan H, Kolh Philippe, Lip Gregory Y H, Manolis Athanasios, McMurray John, Ponikowski Piotr, Rosenhek Raphael, Ruschitzka Frank, Savelieva Irina, Sharma Sanjay, Suwalski Piotr, Tamargo Juan Luis, Taylor Clare J, Van Gelder Isabelle C, Voors Adriaan A, Windecker Stephan, Zamorano Jose Luis, Zeppenfeld Katja. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016 Nov;18 (11):1609–1678. doi: 10.1093/europace/euw295. [DOI] [PubMed] [Google Scholar]
- 4.Calkins Hugh, Hindricks Gerhard, Cappato Riccardo, Kim Young-Hoon, Saad Eduardo B, Aguinaga Luis, Akar Joseph G, Badhwar Vinay, Brugada Josep, Camm John, Chen Peng-Sheng, Chen Shih-Ann, Chung Mina K, Nielsen Jens Cosedis, Curtis Anne B, Davies D Wyn, Day John D, d'Avila André, de Groot N M S Natasja, Di Biase Luigi, Duytschaever Mattias, Edgerton James R, Ellenbogen Kenneth A, Ellinor Patrick T, Ernst Sabine, Fenelon Guilherme, Gerstenfeld Edward P, Haines David E, Haissaguerre Michel, Helm Robert H, Hylek Elaine, Jackman Warren M, Jalife Jose, Kalman Jonathan M, Kautzner Josef, Kottkamp Hans, Kuck Karl Heinz, Kumagai Koichiro, Lee Richard, Lewalter Thorsten, Lindsay Bruce D, Macle Laurent, Mansour Moussa, Marchlinski Francis E, Michaud Gregory F, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Okumura Ken, Packer Douglas, Pokushalov Evgeny, Reynolds Matthew R, Sanders Prashanthan, Scanavacca Mauricio, Schilling Richard, Tondo Claudio, Tsao Hsuan-Ming, Verma Atul, Wilber David J, Yamane Teiichi. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017 Oct;14 (10):e275–e444. doi: 10.1016/j.hrthm.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Packer Douglas L, Mark Daniel B, Robb Richard A, Monahan Kristi H, Bahnson Tristram D, Poole Jeanne E, Noseworthy Peter A, Rosenberg Yves D, Jeffries Neal, Mitchell L Brent, Flaker Greg C, Pokushalov Evgeny, Romanov Alexander, Bunch T Jared, Noelker Georg, Ardashev Andrey, Revishvili Amiran, Wilber David J, Cappato Riccardo, Kuck Karl-Heinz, Hindricks Gerhard, Davies D Wyn, Kowey Peter R, Naccarelli Gerald V, Reiffel James A, Piccini Jonathan P, Silverstein Adam P, Al-Khalidi Hussein R, Lee Kerry L. Effect of Catheter Ablation vs Antiarrhythmic Drug Therapy on Mortality, Stroke, Bleeding, and Cardiac Arrest Among Patients With Atrial Fibrillation: The CABANA Randomized Clinical Trial. JAMA. 2019 Apr 02;321 (13):1261–1274. doi: 10.1001/jama.2019.0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guillomot M, Fléchon J E, Wintenberger-Torres S. Cytochemical studies of uterine and trophoblastic surface coats during blastocyst attachment in the ewe. J. Reprod. Fertil. 1982 May;65 (1):1–8. doi: 10.1530/jrf.0.0650001. [DOI] [PubMed] [Google Scholar]
- 7.Luik Armin, Radzewitz Andrea, Kieser Meinhard, Walter Marlene, Bramlage Peter, Hörmann Patrick, Schmidt Kerstin, Horn Nicolas, Brinkmeier-Theofanopoulou Maria, Kunzmann Kevin, Riexinger Tobias, Schymik Gerhard, Merkel Matthias, Schmitt Claus. Cryoballoon Versus Open Irrigated Radiofrequency Ablation in Patients With Paroxysmal Atrial Fibrillation: The Prospective, Randomized, Controlled, Noninferiority FreezeAF Study. Circulation. 2015 Oct 06;132 (14):1311–9. doi: 10.1161/CIRCULATIONAHA.115.016871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reynolds Matthew R, Zheng Qi, Doros Gheorghe. Laser balloon ablation for AF: A systematic review and meta-analysis. J. Cardiovasc. Electrophysiol. 2018 Oct;29 (10):1363–1370. doi: 10.1111/jce.13698. [DOI] [PubMed] [Google Scholar]
- 9.Ma Honglan, Sun Dongdong, Luan Hui, Feng Wei, Zhou Yaqiong, Wu Jine, He Caiyun, Sun Chaofeng. Efficacy and safety of cryoballoon ablation versus radiofrequency catheter ablation in atrial fibrillation: an updated meta-analysis. Postepy Kardiol Interwencyjnej. 2017;13 (3):240–249. doi: 10.5114/aic.2017.70196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guler Tümer Erdem, Aksu Tolga, Yalin Kivanc, Golcuk Sukriye Ebru, Mutluer Ferit Onur, Bozyel Serdar. Combined Cryoballoon and Radiofrequency Ablation Versus Radiofrequency Ablation Alone for Long-Standing Persistent Atrial Fibrillation. Am. J. Med. Sci. 2017 Dec;354 (6):586–596. doi: 10.1016/j.amjms.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 11.Yalin Kivanc, Abdin Amr, Lyan Evgeny, Sawan Noureddin, Liosis Spyridon, Elsner Christian, Jobs Alexander, Brüggemann Ben, Koester Jelena, Eitel Ingo, Eitel Charlotte, Tilz Roland Richard. Safety and efficacy of persistent atrial fibrillation ablation using the second-generation cryoballoon. Clin Res Cardiol. 2018 Jul;107 (7):570–577. doi: 10.1007/s00392-018-1219-1. [DOI] [PubMed] [Google Scholar]
- 12.Abdin Amr, Yalin Kivanc, Lyan Evgeny, Sawan Noureddin, Liosis Sypridon, Meyer-Saraei Roza, Elsner Christian, Lange Stefan A, Heeger Christian-Hendrik, Eitel Charlotte, Eitel Ingo, Tilz Roland Richard. Safety and efficacy of cryoballoon ablation for the treatment of atrial fibrillation in elderly patients. Clin Res Cardiol. 2019 Feb;108 (2):167–174. doi: 10.1007/s00392-018-1336-x. [DOI] [PubMed] [Google Scholar]
- 13.Yalin Kivanc, Lyan Evgeny, Abdin Amr, Heeger Christian-Hendrik, Vogler Julia, Liosis Spyridon, Eitel Ingo, Meyer-Saraei Roza, Elsner Christian, Eitel Charlotte, Tilz Roland Richard. Second-generation cryoballoon for pulmonary vein isolation in patients with pulmonary vein abnormality: Safety, efficacy and lessons from re-ablation procedures. Int. J. Cardiol. 2018 Dec 01;272 ():142–148. doi: 10.1016/j.ijcard.2018.07.033. [DOI] [PubMed] [Google Scholar]
- 14.Heeger Christian-Hendrik, Abdin Amr, Mathew Shibu, Reissmann Bruno, Yalin Kivanc, Liosis Spyridon, Fink Thomas, Proietti Riccardo, Eitel Charlotte, Vogler Julia, Lemeš Christine, Maurer Tilman, Rillig Andreas, Meyer-Saraei Roza, Graf Tobias, Wohlmuth Peter, Goldmann Britta, Ouyang Feifan, Kuck Karl-Heinz, Metzner Andreas, Tilz Roland Richard. Efficacy and Safety of Cryoballoon Ablation in Patients With Heart Failure and Reduced Left Ventricular Ejection Fraction - A Multicenter Study. Circ. J. 2019 Jul 25;83 (8):1653–1659. doi: 10.1253/circj.CJ-19-0151. [DOI] [PubMed] [Google Scholar]
- 15.Landolina Maurizio, Arena Giuseppe, Iacopino Saverio, Verlato Roberto, Pieragnoli Paolo, Curnis Antonio, Lunati Maurizio, Rauhe Werner, Senatore Gaetano, Sciarra Luigi, Molon Giulio, Agricola Pietro Maria G, Padeletti Luigi, Tondo Claudio. Center experience does not influence long-term outcome and peri-procedural complications after cryoballoon ablation of paroxysmal atrial fibrillation: Data on 860 patients from the real-world multicenter observational project. Int. J. Cardiol. 2018 Dec 01;272 ():130–136. doi: 10.1016/j.ijcard.2018.07.051. [DOI] [PubMed] [Google Scholar]
- 16.Saitoh Yukio, Irfan Ghazala, Ciconte Giuseppe, Mugnai Giacomo, Sieira Juan, Di Giovanni Giacomo, Baltogiannis Giannis, Conte Giulio, Hünük Burak, Ströker Erwin, Velagić Vedran, Overeinder Ingrid, De Asmundis Carlo, Chierchia Gian-Battista, Brugada Pedro. Persistence of Phrenic Nerve Palsy Following 28-mm Cryoballoon Ablation: A Four-Year Single Center Experience. Pacing Clin Electrophysiol. 2015 Jul;38 (7):807–14. doi: 10.1111/pace.12636. [DOI] [PubMed] [Google Scholar]
- 17.Edriss Hawa, Denega Tatiana, Test Victor, Nugent Kenneth. Pulmonary vein stenosis complicating radiofrequency catheter ablation for atrial fibrillation: A literature review. Respir Med. 2016 Aug;117 ():215–22. doi: 10.1016/j.rmed.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Voskoboinik Aleksandr, Moskovitch Jeremy T, Harel Nadav, Sanders Prashanthan, Kistler Peter M, Kalman Jonathan M. Revisiting pulmonary vein isolation alone for persistent atrial fibrillation: A systematic review and meta-analysis. Heart Rhythm. 2017 May;14 (5):661–667. doi: 10.1016/j.hrthm.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Cardoso Rhanderson, Mendirichaga Rodrigo, Fernandes Gilson, Healy Chris, Lambrakos Litsa K, Viles-Gonzalez Juan F, Goldberger Jeffrey J, Mitrani Raul D. Cryoballoon versus Radiofrequency Catheter Ablation in Atrial Fibrillation: A Meta-Analysis. J. Cardiovasc. Electrophysiol. 2016 Oct;27 (10):1151–1159. doi: 10.1111/jce.13047. [DOI] [PubMed] [Google Scholar]
- 20.Di Biase Luigi, Burkhardt J David, Santangeli Pasquale, Mohanty Prasant, Sanchez Javier E, Horton Rodney, Gallinghouse G Joseph, Themistoclakis Sakis, Rossillo Antonio, Lakkireddy Dhanunjaya, Reddy Madhu, Hao Steven, Hongo Richard, Beheiry Salwa, Zagrodzky Jason, Rong Bai, Mohanty Sanghamitra, Elayi Claude S, Forleo Giovanni, Pelargonio Gemma, Narducci Maria Lucia, Dello Russo Antonio, Casella Michela, Fassini Gaetano, Tondo Claudio, Schweikert Robert A, Natale Andrea. Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation. 2014 Jun 24;129 (25):2638–44. doi: 10.1161/CIRCULATIONAHA.113.006426. [DOI] [PubMed] [Google Scholar]
- 21.Zhao Yue, Yang Yuan, Tang Xuejiao, Yu Xiang, Zhang Lei, Xiao Hua. New oral anticoagulants compared to warfarin for perioperative anticoagulation in patients undergoing atrial fibrillation catheter ablation: a meta-analysis of continuous or interrupted new oral anticoagulants during ablation compared to interrupted or continuous warfarin. J Interv Card Electrophysiol. 2017 Apr;48 (3):267–282. doi: 10.1007/s10840-016-0221-7. [DOI] [PubMed] [Google Scholar]
- 22.Di Biase Luigi, Burkhardt J David, Mohanty Prasant, Sanchez Javier, Horton Rodney, Gallinghouse G Joseph, Lakkireddy Dhanunjay, Verma Atul, Khaykin Yaariv, Hongo Richard, Hao Steven, Beheiry Salwa, Pelargonio Gemma, Dello Russo Antonio, Casella Michela, Santarelli Pietro, Santangeli Pasquale, Wang Paul, Al-Ahmad Amin, Patel Dimpi, Themistoclakis Sakis, Bonso Aldo, Rossillo Antonio, Corrado Andrea, Raviele Antonio, Cummings Jennifer E, Schweikert Robert A, Lewis William R, Natale Andrea. Periprocedural stroke and management of major bleeding complications in patients undergoing catheter ablation of atrial fibrillation: the impact of periprocedural therapeutic international normalized ratio. Circulation. 2010 Jun 15;121 (23):2550–6. doi: 10.1161/CIRCULATIONAHA.109.921320. [DOI] [PubMed] [Google Scholar]
- 23.Baman Timir S, Jongnarangsin Krit, Chugh Aman, Suwanagool Arisara, Guiot Aurelie, Madenci Arin, Walsh Spencer, Ilg Karl J, Gupta Sanjaya K, Latchamsetty Rakesh, Bagwe Suveer, Myles James D, Crawford Thomas, Good Eric, Bogun Frank, Pelosi Frank, Morady Fred, Oral Hakan. Prevalence and predictors of complications of radiofrequency catheter ablation for atrial fibrillation. J. Cardiovasc. Electrophysiol. 2011 Jun;22 (6):626–31. doi: 10.1111/j.1540-8167.2010.01995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spragg David D, Dalal Darshan, Cheema Aamir, Scherr Daniel, Chilukuri Karuna, Cheng Alan, Henrikson Charles A, Marine Joseph E, Berger Ronald D, Dong Jun, Calkins Hugh. Complications of catheter ablation for atrial fibrillation: incidence and predictors. J. Cardiovasc. Electrophysiol. 2008 Jun;19 (6):627–31. doi: 10.1111/j.1540-8167.2008.01181.x. [DOI] [PubMed] [Google Scholar]
- 25.Mikhaylov Evgeny N, Lebedev Dmitry S, Pokushalov Evgeny A, Davtyan Karapet V, Ivanitskii Eduard A, Nechepurenko Anatoly A, Kosonogov Alexey Ya, Kolunin Grigory V, Morozov Igor A, Termosesov Sergey A, Maykov Evgeny B, Khomutinin Dmitry N, Eremin Sergey A, Mayorov Igor M, Romanov Alexander B, Shabanov Vitaliy V, Shatakhtsyan Victoria, Tsivkovskii Viktor, Revishvili Amiran Sh, Shlyakhto Evgeny V. Outcomes of Cryoballoon Ablation in High- and Low-Volume Atrial Fibrillation Ablation Centres: A Russian Pilot Survey. Biomed Res Int. 2015;2015 () doi: 10.1155/2015/591603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moran Darragh, De Regibus Valentina, de Asmundis Carlo, Takarada Ken, Mugnai Giacomo, Ströker Erwin, Aryana Arash, Iacopino Saverio, Ruggiero Diego, Coutiño-Moreno Hugo Enrique, Choudhury Rajin, Abugattas Juan-Pablo, Hacioglu Ebru, Paparella Gaetano, Brugada Pedro, Chierchia Gian-Battista. Second generation cryoballoon ablation for atrial fibrillation in young adults: midterm outcome in patients under 40 years of age. Europace. 2018 Feb 01;20 (2):295–300. doi: 10.1093/europace/euw395. [DOI] [PubMed] [Google Scholar]
- 27.Abugattas Juan-Pablo, Iacopino Saverio, Moran Darragh, De Regibus Valentina, Takarada Ken, Mugnai Giacomo, Ströker Erwin, Coutiño-Moreno Hugo Enrique, Choudhury Rajin, Storti Cesare, De Greef Yves, Paparella Gaetano, Brugada Pedro, de Asmundis Carlo, Chierchia Gian-Battista. Efficacy and safety of the second generation cryoballoon ablation for the treatment of paroxysmal atrial fibrillation in patients over 75 years: a comparison with a younger cohort. Europace. 2017 Nov 01;19 (11):1798–1803. doi: 10.1093/europace/eux023. [DOI] [PubMed] [Google Scholar]
- 28.Mugnai Giacomo, de Asmundis Carlo, Iacopino Saverio, Stroker Erwin, Longobardi Massimo, De Regibus Valentina, Coutino-Moreno Hugo Enrique, Takarada Ken, Choudhury Rajin, Abugattas de Torres Juan Pablo, Storti Cesare, Brugada Pedro, Chierchia Gian-Battista. Comparison of the Incidences of Complications After Second-Generation Cryoballoon Ablation of Atrial Fibrillation Using Vitamin K Antagonists Versus Novel Oral Anticoagulants. Am. J. Cardiol. 2017 Jul 15;120 (2):223–229. doi: 10.1016/j.amjcard.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Kalish Jeffrey, Eslami Mohammad, Gillespie David, Schermerhorn Marc, Rybin Denis, Doros Gheorghe, Farber Alik. Routine use of ultrasound guidance in femoral arterial access for peripheral vascular intervention decreases groin hematoma rates. J. Vasc. Surg. 2015 May;61 (5):1231–8. doi: 10.1016/j.jvs.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Okishige Kaoru, Nakamura Tomofumi, Aoyagi Hideshi, Kawaguchi Naohiko, Yamashita Mitsumi, Kurabayashi Manabu, Suzuki Hidetoshi, Asano Mitsutoshi, Shimura Tsukasa, Yamauchi Yasuteru, Sasano Tetsuo, Hirao Kenzo. Comparative study of hemorrhagic and ischemic complications among anticoagulants in patients undergoing cryoballoon ablation for atrial fibrillation. J Cardiol. 2017 Jan;69 (1):11–15. doi: 10.1016/j.jjcc.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 31. VS Mahadevan , , , , S Jimeno, LN Benson , PR McLaughlin , EM Horlick . Pre-closure of femoral venous access sites used for large-sized sheath insertion with the Perclose device in adults undergoing cardiac inter- vention. Heart. 2008;94:571–572. doi: 10.1136/hrt.2006.095935. [DOI] [PubMed] [Google Scholar]
- 32.Yorgun Hikmet, Canpolat Uğur, Ates Ahmet Hakan, Oksul Metin, Sener Yusuf Ziya, Akkaya Fatih, Aytemir Kudret. Comparison of standard vs modified "figure-of-eight" suture to achieve femoral venous hemostasis after cryoballoon based atrial fibrillation ablation. Pacing Clin Electrophysiol. 2019 Sep;42 (9):1175–1182. doi: 10.1111/pace.13764. [DOI] [PubMed] [Google Scholar]
- 33.Gurses Kadri Murat, Kocyigit Duygu, Yalcin Muhammed Ulvi, Evranos Banu, Yorgun Hikmet, Sahiner Mehmet Levent, Kaya Ergun Baris, Oto Mehmet Ali, Ozer Necla, Aytemir Kudret. Safety and efficacy outcomes of protamine administration for heparin reversal following cryoballoon-based pulmonary vein isolation. J Interv Card Electrophysiol. 2015 Aug;43 (2):161–7. doi: 10.1007/s10840-015-9989-0. [DOI] [PubMed] [Google Scholar]
- 34.Aksu Tolga, Baysal Erkan, Guler Tümer Erdem, Golcuk Sukriye Ebru, Erden İsmail, Ozcan Kazim Serhan. Predictors of atrial fibrillation recurrence after cryoballoon ablation. J Blood Med. 2015;6 ():211–7. doi: 10.2147/JBM.S81551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klimek-Piotrowska Wiesława, Hołda Mateusz K, Koziej Mateusz, Piątek Katarzyna, Hołda Jakub. Anatomy of the true interatrial septum for transseptal access to the left atrium. Ann. Anat. 2016 May;205 ():60–4. doi: 10.1016/j.aanat.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 36.O'Brien Barry, Zafar Haroon, De Freitas Simon, Sharif Faisal. Transseptal puncture - Review of anatomy, techniques, complications and challenges. Int. J. Cardiol. 2017 Apr 15;233 ():12–22. doi: 10.1016/j.ijcard.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 37.De Ponti Roberto, Cappato Riccardo, Curnis Antonio, Della Bella Paolo, Padeletti Luigi, Raviele Antonio, Santini Massimo, Salerno-Uriarte Jorge A. Trans-septal catheterization in the electrophysiology laboratory: data from a multicenter survey spanning 12 years. J. Am. Coll. Cardiol. 2006 Mar 07;47 (5):1037–42. doi: 10.1016/j.jacc.2005.10.046. [DOI] [PubMed] [Google Scholar]
- 38.Bayrak Fatih, Chierchia Gian-Battista, Namdar Mehdi, Yazaki Yoshinao, Sarkozy Andrea, de Asmundis Carlo, Muller-Burri Stephan Andreas, Rao Jayakeerthi, Ricciardi Danilo, Sorgente Antonio, Brugada Pedro. Added value of transoesophageal echocardiography during transseptal puncture performed by inexperienced operators. Europace. 2012 May;14 (5):661–5. doi: 10.1093/europace/eur366. [DOI] [PubMed] [Google Scholar]
- 39.Saliba Walid, Thomas James. Intracardiac echocardiography during catheter ablation of atrial fibrillation. Europace. 2008 Nov;10 Suppl 3 ():iii42–7. doi: 10.1093/europace/eun233. [DOI] [PubMed] [Google Scholar]
- 40.Erden İsmail, Erden Emine Çakcak, Golcuk Ebru, Aksu Tolga, Yalin Kıvanç, Güler Tümer Erdem, Özcan Kazım Serhan, Turan Burak. Impact of transesophageal echocardiography during transseptal puncture on atrial fibrillation ablation. J Arrhythm. 2016 Jun;32 (3):170–5. doi: 10.1016/j.joa.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aksu Tolga, Guler Tumer Erdem, Yalin Kivanc, Golcuk Sukriye Ebru, Ozcan Kazim Serhan, Guler Niyazi. A Novel Deep Inspiration Maneuver for Difficult Transseptal Puncture. Am. J. Cardiol. 2017 Feb 01;119 (3):428–433. doi: 10.1016/j.amjcard.2016.10.023. [DOI] [PubMed] [Google Scholar]
- 42.Fisher John D, Krumerman Andrew K. Tamponade detection: did you look at the heart borders (redux)? Pacing Clin Electrophysiol. 2011 Jan;34 (1) doi: 10.1111/j.1540-8159.2010.02937.x. [DOI] [PubMed] [Google Scholar]
- 43.Holbrook Anne, Schulman Sam, Witt Daniel M, Vandvik Per Olav, Fish Jason, Kovacs Michael J, Svensson Peter J, Veenstra David L, Crowther Mark, Guyatt Gordon H. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141 (2 Suppl):e152S–e184S. doi: 10.1378/chest.11-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ruff Christian T, Giugliano Robert P, Antman Elliott M. Management of Bleeding With Non-Vitamin K Antagonist Oral Anticoagulants in the Era of Specific Reversal Agents. Circulation. 2016 Jul 19;134 (3):248–61. doi: 10.1161/CIRCULATIONAHA.116.021831. [DOI] [PubMed] [Google Scholar]
- 45.Mujović Nebojša, Marinković Milan, Marković Nebojša, Kocijančić Aleksandar, Kovačević Vladan, Simić Dragan, Ristić Arsen, Stanković Goran, Miličić Biljana, Putnik Svetozar, Vujisić-Tešić Bosiljka, Potpara Tatjana S. Management and Outcome of Periprocedural Cardiac Perforation and Tamponade with Radiofrequency Catheter Ablation of Cardiac Arrhythmias: A Single Medium-Volume Center Experience. Adv Ther. 2016 Oct;33 (10):1782–1796. doi: 10.1007/s12325-016-0402-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chan Ngai-Yin, Choy Chi-Chung, Lau Chun-Leung, Lo Ying-Keung, Chu Pui-Shan, Yuen Ho-Chuen, Mok Ngai-Shing, Tsui Ping-Tim, Lau Suet-Ting. Persistent iatrogenic atrial septal defect after pulmonary vein isolation by cryoballoon: an under-recognized complication. Europace. 2011 Oct;13 (10):1406–10. doi: 10.1093/europace/eur138. [DOI] [PubMed] [Google Scholar]
- 47.Mugnai Giacomo, Sieira Juan, Ciconte Giuseppe, Hervas Marta Soriano, Irfan Ghazala, Saitoh Yukio, Hünük Burak, Ströker Erwin, Velagic Vedran, Wauters Kristel, Tondo Claudio, Molon Giulio, De Asmundis Carlo, Brugada Pedro, Chierchia Gian-Battista. One Year Incidence of Atrial Septal Defect after PV Isolation: A Comparison Between Conventional Radiofrequency and Cryoballoon Ablation. Pacing Clin Electrophysiol. 2015 Sep;38 (9):1049–57. doi: 10.1111/pace.12663. [DOI] [PubMed] [Google Scholar]
- 48.Eshcol Jayasheel, Wimmer Alan P. Hemodynamically significant iatrogenic atrial septal defects after cryoballoon ablation. HeartRhythm Case Rep. 2019 Jan;5 (1):17–21. doi: 10.1016/j.hrcr.2018.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tang Ri-Bo, Dong Jian-Zeng, Long De-Yong, Yu Rong-Hui, Liu Xing-Peng, Cheng Yan-Li, Sang Cai-Hua, Ning Man, Jiang Chen-Xi, Avula Uma Mahesh R, Bai Rong, Liu Nian, Ruan Yan-Fei, Du Xin, Ma Chang-Sheng. Incidence and clinical characteristics of transient ST-T elevation during transseptal catheterization for atrial fibrillation ablation. Europace. 2015 Apr;17 (4):579–83. doi: 10.1093/europace/euu278. [DOI] [PubMed] [Google Scholar]
- 50.Arita Takeshi, Kubota Satoko, Okamoto Kazuhiko, Kuma Fumiaki, Nakasuga Kazuta, Koga Hideyuki, Ito Hiroyuki, Maruyama Toru, Kaji Yoshikazu, Harada Mine. Bezold-Jarisch-like reflex during Brockenbrough's procedure for radiofrequency catheter ablation of focal left atrial fibrillation: report of two cases. J Interv Card Electrophysiol. 2003 Jun;8 (3):195–202. doi: 10.1023/a:1023917221763. [DOI] [PubMed] [Google Scholar]
- 51.Kuwahara Taishi, Takahashi Atsushi, Takahashi Yoshihide, Kobori Atsushi, Miyazaki Shinsuke, Takei Asumi, Fujii Akira, Kusa Shigeki, Yagishita Atsuhiko, Okubo Kenji, Fujino Tadashi, Nozato Toshihiro, Hikita Hiroyuki, Sato Akira, Aonuma Kazutaka. Clinical characteristics of massive air embolism complicating left atrial ablation of atrial fibrillation: lessons from five cases. Europace. 2012 Feb;14 (2):204–8. doi: 10.1093/europace/eur314. [DOI] [PubMed] [Google Scholar]
- 52.Malik Neera, Claus Paul L, Illman Jeffery E, Kligerman Seth J, Moynagh Michael R, Levin David L, Woodrum David A, Arani Arvin, Arunachalam Shivaram P, Araoz Philip A. Air embolism: diagnosis and management. Future Cardiol. 2017 Jul;13 (4):365–378. doi: 10.2217/fca-2017-0015. [DOI] [PubMed] [Google Scholar]
- 53.Cay Serkan, Ozeke Ozcan, Ozcan Firat, Topaloglu Serkan, Aras Dursun. Coronary Air Embolism during Cryoablation of Atrial Fibrillation: A Catastrophic Complication and Its Management. J Atr Fibrillation. 2017 Dec 19;10 (3) doi: 10.4022/jafib.1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wasmer Kristina, Zellerhoff Stephan, Köbe Julia, Mönnig Gerold, Pott Christian, Dechering Dirk G, Lange Philipp S, Frommeyer Gerrit, Eckardt Lars. Incidence and management of inadvertent puncture and sheath placement in the aorta during attempted transseptal puncture. Europace. 2017 Mar 01;19 (3):447–457. doi: 10.1093/europace/euw037. [DOI] [PubMed] [Google Scholar]
- 55.GERBODE F, HULTGREN H, MELROSE D, OSBORN J. Syndrome of left ventricular-right atrial shunt; successful surgical repair of defect in five cases, with observation of bradycardia on closure. Ann. Surg. 1958 Sep;148 (3):433–46. doi: 10.1097/00000658-195809000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mugnai Giacomo, de Asmundis Carlo, Iacopino Saverio, Ströker Erwin, Longobardi Massimo, Negro Maria Claudia, De Regibus Valentina, Coutino-Moreno Hugo Enrique, Takarada Ken, Choudhury Rajin, de Torres Juan Pablo Abugattas, Storti Cesare, Brugada Pedro, Chierchia Gian-Battista. Acute pericarditis following second-generation cryoballoon ablation for atrial fibrillation. J Interv Card Electrophysiol. 2018 Apr;51 (3):279–284. doi: 10.1007/s10840-018-0329-z. [DOI] [PubMed] [Google Scholar]
- 57.Chierchia Gian Battista, Capulzini Lucio, Droogmans Steven, Sorgente Antonio, Sarkozy Andrea, Müller-Burri Andreas, Paparella Gaetano, de Asmundis Carlo, Yazaki Yoshinao, Kerkhove Dirk, Van Camp Guy, Brugada Pedro. Pericardial effusion in atrial fibrillation ablation: a comparison between cryoballoon and radiofrequency pulmonary vein isolation. Europace. 2010 Mar;12 (3):337–41. doi: 10.1093/europace/eup422. [DOI] [PubMed] [Google Scholar]
- 58.Chun K R Julian, Perrotta Laura, Bordignon Stefano, Khalil Jan, Dugo Daniela, Konstantinou Athanasios, Fürnkranz Alexander, Schmidt Boris. Complications in Catheter Ablation of Atrial Fibrillation in 3,000 Consecutive Procedures: Balloon Versus Radiofrequency Current Ablation. JACC Clin Electrophysiol. 2017 Feb;3 (2):154–161. doi: 10.1016/j.jacep.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 59.Kuck Karl-Heinz, Brugada Josep, Fürnkranz Alexander, Metzner Andreas, Ouyang Feifan, Chun K R Julian, Elvan Arif, Arentz Thomas, Bestehorn Kurt, Pocock Stuart J, Albenque Jean-Paul, Tondo Claudio. Cryoballoon or Radiofrequency Ablation for Paroxysmal Atrial Fibrillation. N. Engl. J. Med. 2016 Jun 09;374 (23):2235–45. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 60.Aksu Tolga, Golcuk Sukriye Ebru, Guler Tümer Erdem, Yalin Kivanç, Erden Ismail. Prediction of mid-term outcome after cryo-balloon ablation of atrial fibrillation using post-procedure high-sensitivity troponin level. Cardiovasc J Afr. 2015 Mar 19;26 (4):165–70. doi: 10.5830/CVJA-2015-027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sánchez-Quintana Damian, Cabrera José Angel, Climent Vicente, Farré Jerónimo, Weiglein Andreas, Ho Siew Yen. How close are the phrenic nerves to cardiac structures? Implications for cardiac interventionalists. J. Cardiovasc. Electrophysiol. 2005 Mar;16 (3):309–13. doi: 10.1046/j.1540-8167.2005.40759.x. [DOI] [PubMed] [Google Scholar]
- 62.Neumann Thomas, Vogt Jürgen, Schumacher Burghard, Dorszewski Anja, Kuniss Malte, Neuser Hans, Kurzidim Klaus, Berkowitsch Alexander, Koller Marcus, Heintze Johannes, Scholz Ursula, Wetzel Ulrike, Schneider Michael A E, Horstkotte Dieter, Hamm Christian W, Pitschner Heinz-Friedrich. Circumferential pulmonary vein isolation with the cryoballoon technique results from a prospective 3-center study. J. Am. Coll. Cardiol. 2008 Jul 22;52 (4):273–8. doi: 10.1016/j.jacc.2008.04.021. [DOI] [PubMed] [Google Scholar]
- 63.Ma Honglan, Sun Dongdong, Luan Hui, Feng Wei, Zhou Yaqiong, Wu Jine, He Caiyun, Sun Chaofeng. Efficacy and safety of cryoballoon ablation versus radiofrequency catheter ablation in atrial fibrillation: an updated meta-analysis. Postepy Kardiol Interwencyjnej. 2017;13 (3):240–249. doi: 10.5114/aic.2017.70196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Okumura Yasuo, Henz Benhur D, Bunch T Jared, Dalegrave Charles, Johnson Susan B, Packer Douglas L. Distortion of right superior pulmonary vein anatomy by balloon catheters as a contributor to phrenic nerve injury. J. Cardiovasc. Electrophysiol. 2009 Oct;20 (10):1151–7. doi: 10.1111/j.1540-8167.2009.01495.x. [DOI] [PubMed] [Google Scholar]
- 65.Andrié René P, Schrickel Jan W, Nickenig Georg, Lickfett Lars. Left phrenic nerve injury during cryoballoon ablation of the left superior pulmonary vein. Pacing Clin Electrophysiol. 2012 Nov;35 (11):e334–6. doi: 10.1111/j.1540-8159.2012.03470.x. [DOI] [PubMed] [Google Scholar]
- 66.Hermida Jean-Sylvain, Traullé Sarah, Kubala Maciej. Left phrenic nerve injury after cryoballoon ablation of the pulmonary veins. Europace. 2013 Apr;15 (4) doi: 10.1093/europace/eus296. [DOI] [PubMed] [Google Scholar]
- 67.Yorgun Hikmet, Canpolat Ugur, Kocyigit Duygu, Çöteli Cem, Evranos Banu, Aytemir Kudret. Left atrial appendage isolation in addition to pulmonary vein isolation in persistent atrial fibrillation: one-year clinical outcome after cryoballoon-based ablation. Europace. 2017 May 01;19 (5):758–768. doi: 10.1093/europace/eux005. [DOI] [PubMed] [Google Scholar]
- 68.Okishige Kaoru, Aoyagi Hideshi, Nishimura Takurou, Shigeta Takatoshi, Keida Takehiko, Yamauchi Yasuteru, Sasano Tetsuo, Hirao Kenzo. Left phrenic nerve injury during electrical isolation of left-sided pulmonary veins with the second-generation cryoballoon. Pacing Clin Electrophysiol. 2017 Dec;40 (12):1426–1431. doi: 10.1111/pace.13201. [DOI] [PubMed] [Google Scholar]
- 69.Abugattas Juan-Pablo, de Asmundis Carlo, Iacopino Saverio, Salghetti Francesca, Takarada Ken, Coutiño Hugo-Enrique, Ströker Erwin, De Regibus Valentina, de Greef Yves, Brugada Pedro, Sieira Juan, Chierchia Gian-Battista. Phrenic nerve injury during right inferior pulmonary vein ablation with the second-generation cryoballoon: clinical, procedural, and anatomical characteristics. Europace. 2018 Oct 01;20 (10):e156–e163. doi: 10.1093/europace/eux337. [DOI] [PubMed] [Google Scholar]
- 70.Fürnkranz Alexander, Bordignon Stefano, Schmidt Boris, Gunawardene Melanie, Schulte-Hahn Britta, Urban Verena, Bode Frank, Nowak Bernd, Chun Julian K R. Improved procedural efficacy of pulmonary vein isolation using the novel second-generation cryoballoon. J. Cardiovasc. Electrophysiol. 2013 May;24 (5):492–7. doi: 10.1111/jce.12082. [DOI] [PubMed] [Google Scholar]
- 71.Giovanni Giacomo DI, Wauters Kristel, Chierchia Gian-Battista, Sieira Juan, Levinstein Moises, Conte Giulio, DE Asmundis Carlo, Baltogiannis Giannis, Saitoh Yukio, Ciconte Giuseppe, Julia Justo, Mugnai Giacomo, Irfan Ghazala, Brugada Pedro. One-year follow-up after single procedure Cryoballoon ablation: a comparison between the first and second generation balloon. J. Cardiovasc. Electrophysiol. 2014 Aug;25 (8):834–839. doi: 10.1111/jce.12409. [DOI] [PubMed] [Google Scholar]
- 72.Rottner Laura, Fink Thomas, Heeger Christian-Hendrik, Schlüter Michael, Goldmann Britta, Lemes Christine, Maurer Tilman, Reißmann Bruno, Rexha Enida, Riedl Johannes, Santoro Francesco, Wohlmuth Peter, Mathew Shibu, Sohns Christian, Ouyang Feifan, Kuck Karl-Heinz, Metzner Andreas. Is less more? Impact of different ablation protocols on periprocedural complications in second-generation cryoballoon based pulmonary vein isolation. Europace. 2018 Sep 01;20 (9):1459–1467. doi: 10.1093/europace/eux219. [DOI] [PubMed] [Google Scholar]
- 73.Lakhani Mayur, Saiful Faisul, Parikh Valay, Goyal Nikhil, Bekheit Soad, Kowalski Marcin. Recordings of diaphragmatic electromyograms during cryoballoon ablation for atrial fibrillation accurately predict phrenic nerve injury. Heart Rhythm. 2014 Mar;11 (3):369–74. doi: 10.1016/j.hrthm.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 74.CH Heeger, A Pott , C Sohn , A Rilling , A Metzner , M Kuniss . Phrenic Nerve Injury During Pulmonary Vein Isolation Using the Second-Generation Cryoballoon: Characteristics and Follow-up – First Results of the Worldwide YETI registry. ESC 2019 [Google Scholar]
- 75.Packer Douglas L, Kowal Robert C, Wheelan Kevin R, Irwin James M, Champagne Jean, Guerra Peter G, Dubuc Marc, Reddy Vivek, Nelson Linda, Holcomb Richard G, Lehmann John W, Ruskin Jeremy N. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J. Am. Coll. Cardiol. 2013 Apr 23;61 (16):1713–23. doi: 10.1016/j.jacc.2012.11.064. [DOI] [PubMed] [Google Scholar]
- 76.Meyers Anthony M. Promotion of kidney care in countries with limited resources: How does the National Kidney Foundation of South Africa fare? Clin. Nephrol. 2016 Jul 30;86 (2016) (13):69–73. doi: 10.5414/CNP86S111. [DOI] [PubMed] [Google Scholar]
- 77.van Opstal J M, Timmermans C, Blaauw Y, Pison L. Bronchial erosion and hemoptysis after pulmonary vein isolation by cryoballoon ablation. Heart Rhythm. 2011 Sep;8 (9) doi: 10.1016/j.hrthm.2010.06.024. [DOI] [PubMed] [Google Scholar]
- 78.Bhagwandien Rohit, Van Belle Yves, de Groot Natasja, Jordaens Luc. Hemoptysis after pulmonary vein isolation with a cryoballoon: an analysis of the potential etiology. J. Cardiovasc. Electrophysiol. 2011 Sep;22 (9):1067–9. doi: 10.1111/j.1540-8167.2011.02031.x. [DOI] [PubMed] [Google Scholar]
- 79.Aksu Tolga, Ebru Golcuk Sukriye, Yalin Kivanc. Haemoptysis and pulmonary haemorrhage associated with cryoballoon ablation. Europace. 2015 Aug;17 (8) doi: 10.1093/europace/euu407. [DOI] [PubMed] [Google Scholar]
- 80.Kasper Łukasz, Gross-Sondej Iwona, Machalica Beata, Soja Jerzy, Pawlik Wiesław, Sładek Krzysztof. Hemoptysis and lung disease as a manifestation of pulmonary vein stenosis after cryoballoon catheter ablation for atrial fibrillation. Pol. Arch. Med. Wewn. 2016;126 (1-2):94–6. [PubMed] [Google Scholar]
- 81.Aryana Arash, Bowers Mark R, Hayatdavoudi Sa Man, Zhang Yanhong, Afify Alaa, D'Avila André, O'Neill Padraig Gearoid. Impact of Pulmonary Vein Cryoballoon Ablation on Bronchial Injury. J. Cardiovasc. Electrophysiol. 2016 Jul;27 (7):861–7. doi: 10.1111/jce.12983. [DOI] [PubMed] [Google Scholar]
- 82.Stöckigt Florian, Schrickel Jan W, Andrié René, Lickfett Lars. Atrioesophageal fistula after cryoballoon pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 2012 Nov;23 (11):1254–7. doi: 10.1111/j.1540-8167.2012.02324.x. [DOI] [PubMed] [Google Scholar]
- 83.Kawasaki Raymond, Gauri Andre, Elmouchi Darryl, Duggal Manoj, Bhan Adarsh. Atrioesophageal fistula complicating cryoballoon pulmonary vein isolation for paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2014 Jul;25 (7):787–92. doi: 10.1111/jce.12426. [DOI] [PubMed] [Google Scholar]
- 84.Ahmed Humera, Neuzil Petr, d'Avila Andre, Cha Yong-Mei, Laragy Margaret, Mares Karel, Brugge William R, Forcione David G, Ruskin Jeremy N, Packer Douglas L, Reddy Vivek Y. The esophageal effects of cryoenergy during cryoablation for atrial fibrillation. Heart Rhythm. 2009 Jul;6 (7):962–9. doi: 10.1016/j.hrthm.2009.03.051. [DOI] [PubMed] [Google Scholar]
- 85.Fürnkranz Alexander, Chun K R Julian, Metzner Andreas, Nuyens Dieter, Schmidt Boris, Burchard Andre, Tilz Roland, Ouyang Feifan, Kuck Karl Heinz. Esophageal endoscopy results after pulmonary vein isolation using the single big cryoballoon technique. J. Cardiovasc. Electrophysiol. 2010 Aug 01;21 (8):869–74. doi: 10.1111/j.1540-8167.2010.01739.x. [DOI] [PubMed] [Google Scholar]
- 86.Guiot Aurélie, Savouré Arnaud, Godin Bénédicte, Anselme Frédéric. Collateral nervous damages after cryoballoon pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 2012 Apr;23 (4):346–51. doi: 10.1111/j.1540-8167.2011.02219.x. [DOI] [PubMed] [Google Scholar]
- 87.Metzner Andreas, Burchard Andre, Wohlmuth Peter, Rausch Peter, Bardyszewski Alexander, Gienapp Christina, Tilz Roland Richard, Rillig Andreas, Mathew Shibu, Deiss Sebastian, Makimoto Hisaki, Ouyang Feifan, Kuck Karl-Heinz, Wissner Erik. Increased incidence of esophageal thermal lesions using the second-generation 28-mm cryoballoon. Circ Arrhythm Electrophysiol. 2013 Aug;6 (4):769–75. doi: 10.1161/CIRCEP.113.000228. [DOI] [PubMed] [Google Scholar]
- 88.Kuwahara Taishi, Takahashi Atsushi, Takahashi Yoshihide, Kobori Atushi, Miyazaki Shinsuke, Takei Asumi, Fujino Tadashi, Okubo Kenji, Takagi Katsumasa, Fujii Akira, Takigawa Masateru, Watari Yuji, Hikita Hiroyuki, Sato Akira, Aonuma Kazutaka. Clinical characteristics and management of periesophageal vagal nerve injury complicating left atrial ablation of atrial fibrillation: lessons from eleven cases. J. Cardiovasc. Electrophysiol. 2013 Aug;24 (8):847–51. doi: 10.1111/jce.12130. [DOI] [PubMed] [Google Scholar]
- 89.Fürnkranz Alexander, Bordignon Stefano, Schmidt Boris, Böhmig Michael, Böhmer Marie-Christine, Bode Frank, Schulte-Hahn Britta, Nowak Bernd, Dignaß Axel U, Chun Julian K R. Luminal esophageal temperature predicts esophageal lesions after second-generation cryoballoon pulmonary vein isolation. Heart Rhythm. 2013 Jun;10 (6):789–93. doi: 10.1016/j.hrthm.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 90.Aksu Tolga, Golcuk Sukriye, Guler Tumer E, Yalin Kıvanç, Erden Ismail. Gastroparesis as a Complication of Atrial Fibrillation Ablation. Am. J. Cardiol. 2015 Jul 01;116 (1):92–7. doi: 10.1016/j.amjcard.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 91.Kuck Karl-Heinz, Brugada Josep, Fürnkranz Alexander, Metzner Andreas, Ouyang Feifan, Chun K R Julian, Elvan Arif, Arentz Thomas, Bestehorn Kurt, Pocock Stuart J, Albenque Jean-Paul, Tondo Claudio. Cryoballoon or Radiofrequency Ablation for Paroxysmal Atrial Fibrillation. N. Engl. J. Med. 2016 Jun 09;374 (23):2235–45. doi: 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 92.Arentz Thomas, Jander Nikolaus, von Rosenthal Jörg, Blum Thomas, Fürmaier Rudolf, Görnandt Lothar, Josef Neumann Franz, Kalusche Dietrich. Incidence of pulmonary vein stenosis 2 years after radiofrequency catheter ablation of refractory atrial fibrillation. Eur. Heart J. 2003 May;24 (10):963–9. doi: 10.1016/s0195-668x(03)00002-2. [DOI] [PubMed] [Google Scholar]
- 93.Chen S A, Hsieh M H, Tai C T, Tsai C F, Prakash V S, Yu W C, Hsu T L, Ding Y A, Chang M S. Initiation of atrial fibrillation by ectopic beats originating from the pulmonary veins: electrophysiological characteristics, pharmacological responses, and effects of radiofrequency ablation. Circulation. 1999 Nov 02;100 (18):1879–86. doi: 10.1161/01.cir.100.18.1879. [DOI] [PubMed] [Google Scholar]
- 94.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Packer Douglas, Skanes Allan. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005 Mar 08;111 (9):1100–5. doi: 10.1161/01.CIR.0000157153.30978.67. [DOI] [PubMed] [Google Scholar]
- 95.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Natale Andrea, Packer Douglas, Skanes Allan, Ambrogi Federico, Biganzoli Elia. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010 Feb;3 (1):32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 96.Packer Douglas L, Kowal Robert C, Wheelan Kevin R, Irwin James M, Champagne Jean, Guerra Peter G, Dubuc Marc, Reddy Vivek, Nelson Linda, Holcomb Richard G, Lehmann John W, Ruskin Jeremy N. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J. Am. Coll. Cardiol. 2013 Apr 23;61 (16):1713–23. doi: 10.1016/j.jacc.2012.11.064. [DOI] [PubMed] [Google Scholar]
- 97.Holmes David R, Monahan Kristi H, Packer Douglas. Pulmonary vein stenosis complicating ablation for atrial fibrillation: clinical spectrum and interventional considerations. JACC Cardiovasc Interv. 2009 Apr;2 (4):267–76. doi: 10.1016/j.jcin.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 98.Coutiño Hugo-Enrique, Takarada Ken, Sieira Juan, Abugattas Juan-Pablo, Salghetti Francesca, De Regibus Valentina, Ströker Erwin, Brugada Pedro, Iacopino Saverio, de Asmundis Carlo, Chierchia Gian-Battista. Anatomical and procedural predictors of pulmonary vein stenosis in the setting of second-generation cryoballoon ablation. J Cardiovasc Med (Hagerstown) 2018 Jun;19 (6):290–296. doi: 10.2459/JCM.0000000000000646. [DOI] [PubMed] [Google Scholar]
- 99.Narui Ryohsuke, Tokuda Michifumi, Matsushima Masato, Isogai Ryota, Tokutake Kenichi, Yokoyama Kenichi, Hioki Mika, Ito Keiichi, Tanigawa Shin-Ichi, Yamashita Seigo, Inada Keiichi, Shibayama Kenri, Matsuo Seiichiro, Miyanaga Satoru, Sugimoto Kenichi, Yoshimura Michihiro, Yamane Teiichi. Incidence and Factors Associated With the Occurrence of Pulmonary Vein Narrowing After Cryoballoon Ablation. Circ Arrhythm Electrophysiol. 2017 Jun;10 (6) doi: 10.1161/CIRCEP.116.004588. [DOI] [PubMed] [Google Scholar]
- 100.Baran Jakub, Lewandowski Paweł, Smarż Krzysztof, Sikorska Agnieszka, Zaborska Beata, Kułakowski Piotr. Acute Hemodynamic and Tissue Effects of Cryoballoon Ablation on Pulmonary Vessels: The IVUS-Cryo Study. J Am Heart Assoc. 2017 Jun 25;6 (6) doi: 10.1161/JAHA.117.005988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fender Erin A, Widmer R Jay, Hodge David O, Packer Douglas L, Holmes David R. Assessment and Management of Pulmonary Vein Occlusion After Atrial Fibrillation Ablation. JACC Cardiovasc Interv. 2018 Aug 27;11 (16):1633–1639. doi: 10.1016/j.jcin.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 102.Tse Hung-Fat, Kwong Yok-Lam, Lau Chu-Pak. Transvenous cryoablation reduces platelet activation during pulmonary vein ablation compared with radiofrequency energy in patients with atrial fibrillation. J. Cardiovasc. Electrophysiol. 2005 Oct;16 (10):1064–70. doi: 10.1111/j.1540-8167.2005.50103.x. [DOI] [PubMed] [Google Scholar]
- 103.Khairy Paul, Chauvet Patrick, Lehmann John, Lambert Jean, Macle Laurent, Tanguay Jean-François, Sirois Martin G, Santoianni Domenic, Dubuc Marc. Lower incidence of thrombus formation with cryoenergy versus radiofrequency catheter ablation. Circulation. 2003 Apr 22;107 (15):2045–50. doi: 10.1161/01.CIR.0000058706.82623.A1. [DOI] [PubMed] [Google Scholar]
- 104.Lickfett Lars, Hackenbroch Matthias, Lewalter Thorsten, Selbach Stephanie, Schwab Jörg O, Yang Alexander, Balta Osman, Schrickel Jan, Bitzen Alexander, Lüderitz Berndt, Sommer Torsten. Cerebral diffusion-weighted magnetic resonance imaging: a tool to monitor the thrombogenicity of left atrial catheter ablation. J. Cardiovasc. Electrophysiol. 2006 Jan;17 (1):1–7. doi: 10.1111/j.1540-8167.2005.00279.x. [DOI] [PubMed] [Google Scholar]
- 105.Gaita Fiorenzo, Caponi Domenico, Pianelli Martina, Scaglione Marco, Toso Elisabetta, Cesarani Federico, Boffano Carlo, Gandini Giovanni, Valentini Maria Consuelo, De Ponti Roberto, Halimi Franck, Leclercq Jean François. Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. Circulation. 2010 Oct 26;122 (17):1667–73. doi: 10.1161/CIRCULATIONAHA.110.937953. [DOI] [PubMed] [Google Scholar]
- 106.Miyazaki Shinsuke, Watanabe Tomonori, Kajiyama Takatsugu, Iwasawa Jin, Ichijo Sadamitsu, Nakamura Hiroaki, Taniguchi Hiroshi, Hirao Kenzo, Iesaka Yoshito. Thromboembolic Risks of the Procedural Process in Second-Generation Cryoballoon Ablation Procedures: Analysis From Real-Time Transcranial Doppler Monitoring. Circ Arrhythm Electrophysiol. 2017 Dec;10 (12) doi: 10.1161/CIRCEP.117.005612. [DOI] [PubMed] [Google Scholar]
- 107.Tokuda Michifumi, Matsuo Seiichiro, Kato Mika, Sato Hidenori, Oseto Hirotsuna, Okajima Eri, Ikewaki Hidetsugu, Isogai Ryota, Tokutake Kenichi, Yokoyama Kenichi, Narui Ryohsuke, Tanigawa Shin-Ichi, Yamashita Seigo, Inada Keiichi, Yoshimura Michihiro, Yamane Teiichi. Effect of air removal with extracorporeal balloon inflation on incidence of asymptomatic cerebral embolism during cryoballoon ablation of atrial fibrillation. Heart Rhythm. 2017 Sep;14 (9):1291–1296. doi: 10.1016/j.hrthm.2017.05.035. [DOI] [PubMed] [Google Scholar]
- 108.Mugnai Giacomo, Irfan Ghazala, de Asmundis Carlo, Ciconte Giuseppe, Saitoh Yukio, Hunuk Burak, Velagic Vedran, Stroker Erwin, Rossi Paolo, Capulzini Lucio, Brugada Pedro, Chierchia Gian-Battista. Complications in the setting of percutaneous atrial fibrillation ablation using radiofrequency and cryoballoon techniques: A single-center study in a large cohort of patients. Int. J. Cardiol. 2015 Oct 01;196 ():42–9. doi: 10.1016/j.ijcard.2015.05.145. [DOI] [PubMed] [Google Scholar]
- 109.Di Biase Luigi, Burkhardt J David, Santangeli Pasquale, Mohanty Prasant, Sanchez Javier E, Horton Rodney, Gallinghouse G Joseph, Themistoclakis Sakis, Rossillo Antonio, Lakkireddy Dhanunjaya, Reddy Madhu, Hao Steven, Hongo Richard, Beheiry Salwa, Zagrodzky Jason, Rong Bai, Mohanty Sanghamitra, Elayi Claude S, Forleo Giovanni, Pelargonio Gemma, Narducci Maria Lucia, Dello Russo Antonio, Casella Michela, Fassini Gaetano, Tondo Claudio, Schweikert Robert A, Natale Andrea. Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation. 2014 Jun 24;129 (25):2638–44. doi: 10.1161/CIRCULATIONAHA.113.006426. [DOI] [PubMed] [Google Scholar]
- 110.Tscholl Verena, Lsharaf Abdullah Khaled-A, Lin Tina, Bellmann Barbara, Nagel Patrick, Lenz Klaus, Landmesser Ulf, Roser Mattias, Rillig Andreas. Apixaban, rivaroxaban, and dabigatran use in patients undergoing catheter ablation for atrial fibrillation using the second-generation cryoballoon. Clin Cardiol. 2017 Nov;40 (11):1095–1099. doi: 10.1002/clc.22782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Calvo N, Mont L, Vidal B, Nadal M, Montserrat S, Andreu D, Tamborero D, Pare C, Azqueta M, Berruezo A, Brugada J, Sitges M. Usefulness of transoesophageal echocardiography before circumferential pulmonary vein ablation in patients with atrial fibrillation: is it really mandatory? Europace. 2011 Apr;13 (4):486–91. doi: 10.1093/europace/euq456. [DOI] [PubMed] [Google Scholar]
- 112.McCready James W, Nunn Laurence, Lambiase Pier D, Ahsan Syed Y, Segal Oliver R, Rowland Edward, Lowe Martin D, Chow Anthony W. Incidence of left atrial thrombus prior to atrial fibrillation ablation: is pre-procedural transoesophageal echocardiography mandatory? Europace. 2010 Jul;12 (7):927–32. doi: 10.1093/europace/euq074. [DOI] [PubMed] [Google Scholar]
- 113.Kottmaier Marc, Jilek Clemens, Berglar Sophie, Reents Tilko, Bourier Felix, Semmler Verena, Telishevska Martha, Koch-Büttner Katharina, Lengauer Sarah, Kornmayer Marielouise, Rousseva Elena, Brooks Stephanie, Hadamitzky Martin, Kolb Christoph, Hessling Gabriele, Deisenhofer Isabel. Exclusion of left atrial thrombus by dual-source cardiac computed tomography prior to catheter ablation for atrial fibrillation. Clin Res Cardiol. 2019 Feb;108 (2):150–156. doi: 10.1007/s00392-018-1333-0. [DOI] [PubMed] [Google Scholar]
- 114.Güler Tümer Erdem, Aksu Tolga, Özcan Kazım Serhan, Bozyel Serdar. Transient ST-segment elevation due to coronary slow flow during cryoballoon application. Turk Kardiyol Dern Ars. 2018 Jul;46 (5):396–400. doi: 10.5543/tkda.2017.95898. [DOI] [PubMed] [Google Scholar]
- 115.Makimoto Hisaki, Kelm Malte, Shin Dong-In, Blockhaus Christian. Breakage of a Circular Catheter Wedged in a Right Pulmonary Vein during Cryoballoon Pulmonary Vein Isolation. Intern. Med. 2017;56 (9):1057–1059. doi: 10.2169/internalmedicine.56.7924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Canpolat Uğur, Kivrak Ahmet, Hazirolan Tuncay, Aytemir Kudret. Coronary Vasospasm After Isolation of Left Atrial Appendage Using a Second-Generation Cryoballoon. JACC Clin Electrophysiol. 2017 Apr;3 (4):417–419. doi: 10.1016/j.jacep.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 117.Fonseca Wallyson Pereira, Pisani Cristiano F, Lara Sissy, Scanavacca Mauricio. Transient complete atrioventricular block during catheter balloon cryoablation of atrial fibrillation: a case report. Europace. 2017 Dec 01;19 (12) doi: 10.1093/europace/eux229. [DOI] [PubMed] [Google Scholar]
- 118.Fedida Joël, Badenco Nicolas, Gandjbakhch Estelle, Waintraub Xavier, Hidden-Lucet Françoise, Duthoit Guillaume. Reversible mechanical atrioventricular block during cryoablation for paroxysmal atrial fibrillation with a 28 mm balloon. HeartRhythm Case Rep. 2019 Jan;5 (1):15–16. doi: 10.1016/j.hrcr.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]