Abstract
Distal clavicle fractures are less common than mid-shaft fractures in adults and there is no consensus on the best classification system or the ideal treatment approach considering that high nonunion rates have been reported. Although there are numerous treatment options for distal clavicle fractures, a gold standard treatment has not yet been established. Each surgical technique has its pros and cons. In this review article, we provide an overview of classification systems and treatment methods for distal clavicle fractures.
Keywords: Distal clavicle, Fracture, Classification, Treatment
The management of distal (lateral third) clavicle fractures can be challenging because of difficulty in distinguishing subtle variations in the fracture pattern, which may be suggestive of potential fracture instability.1) An analysis of the frequency of distal clavicle fractures by age and sex has revealed that they occur most often in men between 30 and 50 years of age and secondarily in individuals (both men and women) over 70 years of age.2) Distal clavicle fractures are less common than clavicle midshaft fractures and account for 10%–30% of all clavicle fractures. Roughly 30%–45% of all clavicle nonunion fractures occur distally.3,4,5,6,7,8) Distal clavicle fractures may be treated conservatively or surgically, and there is no gold standard or consensus in the field. Importantly, however, conservative treatment of distal clavicle fractures may result in nonunion or pseudoarthrosis; therefore, surgical treatment is recommended when these fractures are unstable. Various strategies for surgical treatment of distal clavicle fractures have been reported, including precontoured locking plate fixation, hook plate fixation, coracoclavicular (CC) fixation (using a suture anchor, suture button device, or screw), tension band wiring fixation, transacromial Kirschner (K)-wire fixation, and arthroscopically assisted techniques. Although appropriate treatment is needed to help ensure fracture healing and a rapid return to preinjury activities of daily living, definitive treatment strategies have not been established and a variety of techniques are used. In this article, we provide an overview of classification systems and treatment methods for distal clavicle fractures and discuss proper treatment strategies for distal clavicle fractures.
CLASSIFICATION
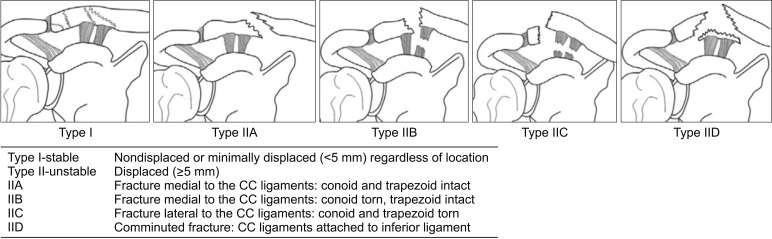
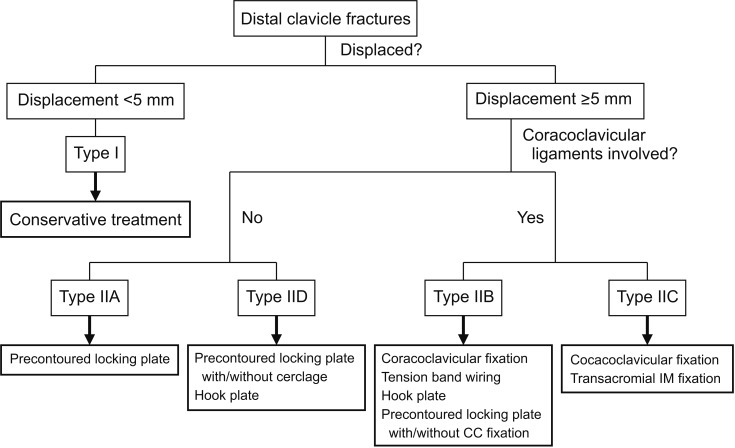
Several classification systems for distal clavicle fractures have been introduced.7,9,10,11) In 1967, Allman11) suggested classification of clavicle fractures based on anatomic location, an approach that does not consider treatment approaches and/or prognosis. In 1994, Nordqvist et al.7) further classified clavicle fractures based on displacement and comminution of the fracture. Robinson9) proposed a more detailed classification system based on the fracture type (i.e., lateral fifth, medial fifth, and diaphyseal) and further divided each type of fracture based on displacement, angulation, intra-articular extension, and comminution in 1998; however, this approach is limited in that it does not have a specific category for distal clavicle fractures. The Neer classification system is based on the fracture location in relation to the CC ligament on simple anteroposterior radiographs and its involvement. It has been widely used since the 1960s.3,4) In 1990, Craig10) introduced a modified version of the Neer classification, which is more detailed and helpful in determining a treatment and prognosis. According to this revised classification system, (1) type 1 fractures occur lateral to the CC ligament with minimal displacement and no involvement of the acromioclavicular (AC) joint; (2) type 2 fractures occur medial to the CC ligament and are divided into two subtypes, subtype 2A (medial to the conoid ligament) and subtype 2B (between the conoid and trapezoid ligaments with a rupture of the conoid ligament); (3) type 3 fractures are similar to type 1 (i.e., also lie lateral to the CC ligament), but they have intra-articular extension; (4) type 4 fractures involve disruption of the periosteal sleeve and the medial fragment gets displaced upwards in children; and (5) type 5 fractures are similar to type 2 (involve a small inferior fragment attached to the CC ligament) and are comminuted. Many surgeons use the modified Neer classification system in the treatment decision-making process. Types 1 and 3 are classified as stable fractures and may be managed conservatively. Types 2 and 5 are classified as unstable fractures, and patients suffering from these fractures complain of pain and functional limitations if treated only conservatively, leading to controversy about how they can be best managed or treated.3,4) In 2018, Cho et al.12) suggested a new classification system for distal clavicle fractures because several studies reported that other classification systems had low interobserver and intraobserver reliability and provided limited treatment-related information.13,14) The new classification system considers fracture displacement and stability, as well as fracture location, to provide more information for diagnosis and associated treatment options including fixation methods. It is based on simple anteroposterior and oblique views of the AC joint and an axial view in shoulder radiography. This classification system proposed that type I fractures are stable, involve no or minimal displacement (<5 mm), and can occur in any location, while type II fractures are unstable and have more significant displacement (≥5 mm). As shown in Fig. 1, type II fractures are subcategorized into four subtypes: (1) type IIA (occur medial to the CC ligament and both the conoid and trapezoid ligaments remain attached to the distal fragment); (2) type IIB (occur medial to the CC ligament and the conoid ligament is detached from the distal fragment); (3) type IIC (occur lateral to the CC ligament and both the conoid and trapezoid ligaments are detached from the medial fragment); and (4) type IID (involve comminution with the inferior fragment that remains attached to the CC ligament). This classification system showed moderate interobserver (κ = 0.434) and substantial intraobserver (κ = 0.644) reliability and was designed to help surgeons choose the most appropriate treatment option and implant type for each type of fracture (Fig. 2).12)
Fig. 1. Cho's classification system of distal clavicle fractures. CC: coracoclavicular. Reprinted from Cho et al.12) according to the Elsevier user license.
Fig. 2. Treatment algorithm based on Cho's classification system. CC: coracoclavicular, IM: intramedullary fixation. Reprinted from Cho et al.12) according to the Elsevier user license.
TREATMENT OPTIONS
Distal clavicle fractures can be treated conservatively or surgically. Results of the management depend on several key factors (e.g., fracture displacement and involvement of CC ligament, which lead to unstable fractures.) Most nondisplaced or minimally displaced fractures can be successfully treated by conservative treatment. In contrast, type II fractures (Neer or Cho's classification) are unstable and may have poor outcomes with conservative management.3,12) Rokito et al.15) reported similar results of the conservative treatment group and surgical treatment group with Neer type 2 fractures regarding pain, function, and strength. However, they observed high nonunion rates (44%), cosmetic problems, or prolonged sling wearing in the conservative group while all in the surgical group had bony union after surgery. Nonunion rates following conservative management of Neer type 2 fractures range from 28% to 44%.3,4,6,15,16,17,18) Therefore, the best approach to the management of Neer type 2 fractures remains controversial. Modified Neer type 5 fractures are similar to type 2 fractures; therefore, they can be considered together. Usually, surgical indications for distal clavicle fractures are as follows: (1) unstable fractures without bony contact and (2) all open fractures with skin compromise and associated neurovascular injury.4,19) As the nonunion rate is so high, displaced and unstable distal clavicle fractures should be treated surgically.
Conservative Treatment
Conservative treatment of distal clavicle fractures includes immobilization with an arm sling or a figure-of-eight bandage. Recently, arm slings have become more commonly used because of patient comfort. Figure-of-eight bandages are not known to have better outcomes and are associated with several problems (e.g., temporary neurovascular dysfunction and pseudoarthrosis.)20) Banerjee et al.1) recommended sling immobilization for 2 weeks and shoulder motion as soon as the initial pain improves. Robinson and Cairns17) reported that conservative management of displaced distal clavicle fractures in 101 patients resulted in good mid-term functional results. Except for seven patients who underwent immediate internal fixation, all patients with a displaced distal clavicle fracture were treated conservatively. There were 57 Neer type 2A fractures, 33 Neer type 2B fractures, and 11 Neer type 3 fractures. The mean Constant-Murley score (CMS) in the conservatively treated group was 93 points. However, 21 of 101 patients had asymptomatic nonunion, 11 had a symptomatic nonunion, and three developed AC joint arthritis; a delayed reconstructive procedure was required at a later follow-up in these 14 patients with nonunion.
Precontoured Locking Plate Fixation with or without CC Fixation
Precontoured locking plates provide firm fixation of the fracture site and allow for early motion of the affected arm. They are precontoured for anatomical fit with the distal clavicle and facilitate multi-planar fixation of the distal fragment and better stability of the small fragment.21) In addition, this type of plate is not associated with impingement of the subacromial space because it allows for fixation of the fracture site without crossing the AC joint.
Several studies have reported outcomes of precontoured locking plate fixation for the treatment of distal clavicle fractures. Lee et al.22) reported on 35 patients with Neer type 2 distal clavicle fractures who had been treated with a precontoured locking plate and an interfragmentary screw (if necessary) without CC stabilization. Bony union was achieved in all patients without major complications (e.g., nonunion, implant failure, and deep infection) and good functional outcomes were obtained (e.g., no significant difference in CMS and the University of California Los Angeles [UCLA] shoulder score compared to the contralateral shoulder). Tiren and Vroemen23) prospectively evaluated the results of fixation with locking plates. Seven patients with displaced Neer type 2 distal clavicle fractures were treated and all achieved bony union without complications and excellent functional scores (CMS, 98; Disabilities of the Arm, Shoulder, and Hand [DASH] score, 3.6; and Self-Reporting Questionnaire, 97). Vaishya et al.21) reported 32 patients with Neer type 2 distal clavicle fractures treated by precontoured locking plate fixation without CC stabilization. They obtained bony union in 31 out of 32 cases with one case suffering from asymptomatic malunion. Shin et al.24) treated 25 patients with unstable distal clavicle fractures by using precontoured locking plates without CC ligament augmentation and achieved bony union in all patients and satisfactory clinical outcomes (CMS, 92; UCLA score, 4.6).
Although several studies have reported satisfactory clinical outcomes, instability caused by CC ligament injury is a main potential challenge when treating displaced Neer type 2 fractures. Therefore, there have been some studies where patients were treated with a combination of locking plate and additional CC fixation using suture anchors or buttons to augment and repair the CC ligaments.25,26,27) Johnston et al.25) introduced a surgical technique designed to treat unstable Neer type 2 distal clavicle fractures by using a precontoured locking plate and CC fixation with a suture button. Six patients underwent treatment using this technique and all achieved a bony union and good clinical outcomes. Seyhan et al.28) evaluated 36 patients with Neer type 2B fractures and divided them into three groups according to the surgical option: (1) tension band and CC fixation with a suture and K-wire (group 1); (2) a precontoured locking plate and CC fixation with a screw (group 2); and (3) a precontoured locking plate and CC fixation with TightRope (Arthrex, Naples, FL, USA; group 3). At 3, 6, and 12 months of follow-ups, the mean CMS was statistically significantly better in group 3 than in the other two groups (95.0 ± 5.1 in group 1, 95.33 ± 3 in group 2, and 99.1 ± 1 in group 3). Han et al.27) treated 12 patients with Neer type 2B distal clavicle fractures with precontoured locking plates combined with suture anchor augmentation of the CC ligament. All 12 patients achieved bony union within 12 weeks without major complications and satisfactory functional outcome.
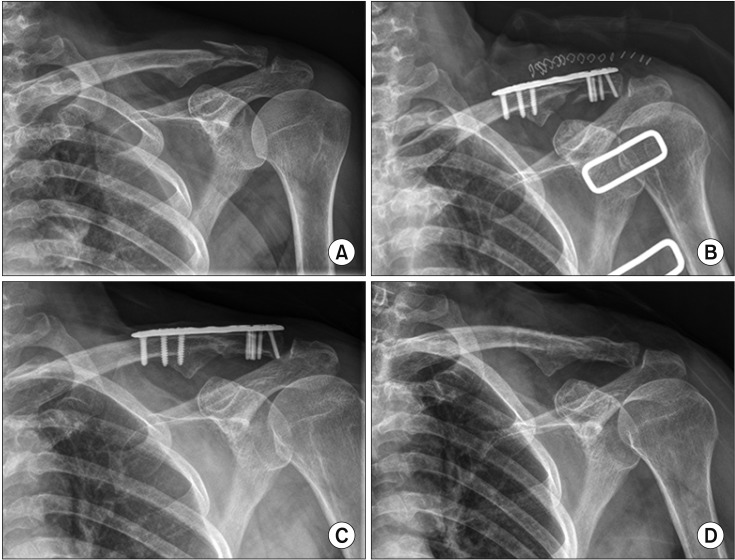
Many authors have reported good to excellent outcomes in patients treated with precontoured locking plates with or without CC fixation; locking plate fixation has recently become a treatment of choice for specific fracture patterns, which have enough large distal fragments to insert screws. However, because the use of precontoured locking plates with or without CC fixation is not ideal for all patterns of distal clavicle fractures, surgeons should consider various treatment options. Nevertheless, it is our belief that precontoured locking plate fixation is one of the best options for unstable distal clavicle fractures including type IIA, B, and D fractures in Cho's classification system (Fig. 3).12)
Fig. 3. A 68-year-old woman with a type IID distal clavicle fracture on the left shoulder was treated by precontoured locking plate fixation without other procedures. (A) Preoperative radiograph. (B) Postoperative radiograph. (C, D) Radiographs obtained at 14 months after surgery showing complete bony union and plate removal.
Hook Plate
The hook plate is a useful fixation device and widely used for Neer type 2 unstable distal clavicle fractures. If the distal fragment is too small to insert screws, a hook plate may be a reliable option.1) The hook is located under the acromion and provides distal leverage that helps maintain reduction of the superiorly displaced medial fragment.29) According to the individual's acromial slope, plates with different hook depths can be used. Numerous studies have reported that hook plate fixation yields satisfactory outcomes (e.g., bony union and shoulder function).30,31,32,33,34,35,36,37,38,39,40) Kashii et al.37) reported on the results of 34 patients with Neer type 2 distal clavicle fractures treated with hook plates. Bony union and good clinical results were achieved in all patients and complications were limited to an acromial fracture (n = 1) and a rotator cuff tear (n = 1). Good et al.41) reviewed 36 patients who underwent fixation with a hook plate and reported a union rate of 95%. Although there were no patients with complications, two patients presented with a peri-implant fracture after another trauma. Therefore, they recommended plate removal within 6 months postoperatively. Lee et al.40) evaluated 35 patients who were treated with hook plates for Neer type 2 distal clavicle fractures. They compared clinical and radiologic outcomes and complications between Neer type 2A and type 2B and reported that all patients had a bony union and satisfactory clinical outcomes (UCLA score, 32.6; the American Shoulder and Elbow Surgeons [ASES] score, 83.5). Additionally, they reported no significant difference in outcomes between type 2A and type 2B fractures.
However, surgeons should consider several key hook-related complications (e.g., subacromial space inflammation, rotator cuff impingement, hook cut-out, acromion osteolysis, and fractures.)31,37,42) Many authors recommend removal of the hook plate within 3 and 6 months after surgery. Oh et al.31) reviewed a total of 425 patients from 21 articles: 60 were treated conservatively and 365, surgically. Among the 365 patients who were treated surgically, 162 were managed by the hook plate and the others, by CC fixation, intramedullary fixation, tension band wiring, or interfragmentary fixation. The nonunion rate was not significantly different among the fixation methods; however, the complication rate was significantly higher in patients treated with a hook plate (40.7%). Zhang et al.43) compared the clinical outcomes of 66 patients who underwent surgical fixation with precontoured locking plates (n = 36) and hook plates (n = 30) and noted no significant differences in union rate and CMS; however, the group treated with hook plates had a significantly higher rate of complications (5.6% vs. 23.3%) and lower ability to return to their work in 3 months (94.4% vs. 73.3%). In a recent meta-analysis, Asadollahi and Bucknill29) evaluated 11 studies including 634 patients to compare the outcomes of hook plates with those of other fixation methods. Hook plate fixation groups had a higher rate of complications than those treated with CC fixation or locking plates; however, there was no significant difference between functional outcomes and union rates among the groups treated with hook plates, CC fixation, and locking plates. They reported that subacromial osteolysis and erosion were the most common complications followed by AC joint arthrosis and peri-implant fractures.
Although hook plate fixation is a reliable option for distal clavicle fractures with very small distal fragments, fractures with severe comminution or an osteoporotic bone are associated with high complication rates related to impingement, implant design, and wounds; plate removal can decrease these risks, but increase medical costs and the risk of comorbidities. Thus, hook plate fixation could be a useful option for type IIB or IID fractures according to Cho's classification.12)
Isolated CC Fixation Using Screws or Flexible Methods
CC screw fixation has been a popular method for the treatment of distal clavicle fractures since it was first introduced by Bosworth in 1941. Several authors reported results of the CC fixation method using screws.44,45,46,47) Fazal et al.44) published a 30 patient case series of temporary CC screw fixation. All patients achieved bony union and returned to their previous activity level by 1 year postoperatively, and screws were removed after bony union. However, CC screw fixation is associated with some key complications (e.g., screw loosening [backing out], limitations of shoulder motion before union, and incorrect screw position). Therefore, screw fixation has been substituted by flexible CC fixation using sutures, suture anchors, tape, or suture button devices.
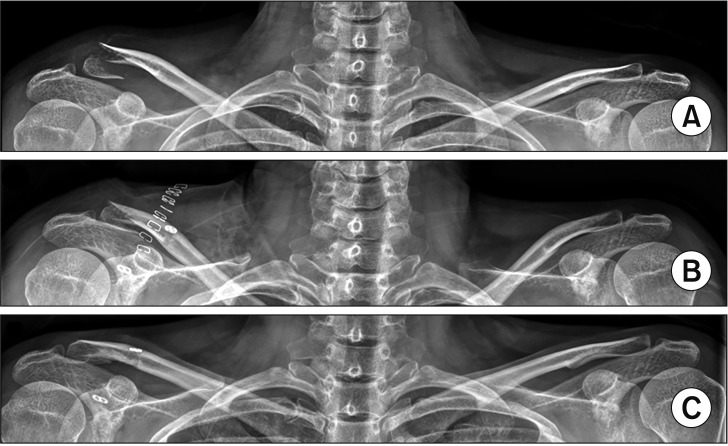
Yang et al.48) treated 29 patients with unstable distal clavicle fractures with single CC suture fixation using Mersilene tape (Ethicon, Somerville, NJ, USA) without CC reconstruction or hardware fixation. They were able to follow 28 patients and bony union was achieved in all. They reported no major complications and good to excellent clinical results. Mirbolook et al.49) evaluated 43 patients with distal clavicle fractures fixed by two pins on the AC joint and one suture anchor for CC fixation. All patients had bony union at a mean of 4.5 months without major complications. Mean CMS was 92.3 ± 4.06 at 12 months postoperatively. Kanchanatawan and Wongthongsalee50) evaluated 39 patients with unstable distal clavicle fractures managed by CC fixation using the bidirectional CC loop technique. All patients achieved bony union without major complications and had good functional outcomes and CMS (92.33). However, enlargement of the clavicle drill hole was observed in nine patients at 30 months or later; therefore, a second operation was needed to remove the buttons and suture loops. Cho et al.51) also reported satisfactory radiological and clinical outcomes following CC fixation using a TightRope in 18 patients with Neer type 2B fractures (Fig. 4). They highlighted that the primary advantage of CC fixation is that implant removal is not required.
Fig. 4. A 44-year-old woman with a type IIC distal clavicle fracture on the left shoulder was treated by TightRope (Arthrex, Naples, FL, USA) fixation with additional circumferential suture. (A) Preoperative radiograph. (B) Postoperative radiograph. (C) Radiograph obtained at 12 months after surgery showing complete bony union with subsidence of the clavicular button.
In several comparative studies, CC flexible fixation has been reported as providing satisfactory results. Yan et al.52) compared the clinical results of CC ligament reconstruction using suture anchors with those using an autologous gracilis tendon (21 patients) and a hook plate (21 patients) in a total of 42 patients. All patients in both groups achieved bony union without major complications and satisfactory clinical outcome at the last follow-up. However, the mean CMS in the CC reconstruction group was significantly higher than that in the hook plate group in the early postoperative period. Hsu et al.53) reported better outcomes and lower complication rates of CC loop technique fixation using Mersilene tape (Ethicon, Somerville, NJ, USA) than those of hook plate fixation. The mean CMS was significantly higher in the CC loop group (95 vs. 87) and the complication rate was significantly lower in the CC loop group (0% vs. 24.5%); the nonunion rates and UCLA scores were not significantly different between the groups.
Arthroscopic Technique
Since arthroscopic techniques were reported to manage AC joint problems successfully, some authors have proposed arthroscopic surgery or arthroscopically assisted surgery for the treatment of distal clavicle fractures.54,55,56,57,58) Most studies performed CC fixation with arthroscopic reduction of displaced fractures to obtain several key advantages: minimal invasiveness, early rehabilitation, decreased postoperative pain, reduced wound problems, and ability to handle concurrent shoulder joint problems such as impingement, rotator cuff tear, or superior labrum anterior and posterior lesions. On the other hand, arthroscopic surgery is technically demanding, requires a high level of skill that can be developed over many years, and is associated with additional time and costs.2,58) Pujol et al.58) introduced an arthroscopic reduction and CC fixation technique using TightRope for the treatment of distal clavicle fractures. They treated four patients with distal clavicle fractures and reported good clinical outcomes. Kraus et al.55) evaluated 23 patients who underwent arthroscopic CC fixation using TightRope with interfragmentary cerclage. At the time of the final follow-up, the union rate was 90% (18 of 20 patients); there were two cases of asymptomatic nonunion. These patients achieved good clinical scores (i.e., mean subject shoulder value was 95.1, and mean CMS was 88.7). Loriaut et al.54) reported on outcomes of 21 patients with Neer type 2B distal clavicle fractures who were treated with an arthroscopically assisted CC fixation using a TightRope. Bony union was achieved in all patients but one who experienced an implant failure at 6 weeks. However, this patient had no symptoms at the final follow-up and did not need additional treatment. Sautet et al.59) introduced an original fixation technique for Neer type 2B distal clavicle fractures, in which arthroscopically assisted subcoracoid suture with Dog Bone clavicular buttons (Arthrex) were used. They performed this surgery on 14 patients and obtained bony union within 3 months in all patients except one patient who experienced delayed union. Recently, Mochizuki et al.60) reported on the treatment of 45 patients with Neer type 2B distal clavicle fractures with the following procedures: (1) an arthroscopically assisted procedure with a synthetic conoid ligament reconstruction using ZipTight (Zimmer Biomet, Warsaw, USA) and (2) fracture site fixation with K-wires. Bony union was achieved in all patients and there were no cases of nonunion or major complications. They obtained highly satisfactory clinical outcomes (Quick DASH, 3.8 ± 2.8; ASES, 92.3 ± 3.2; and CMS, 94.1 ± 3.0) at 1-year follow-up. Although these studies reported good radiologic and clinical results, there are several limitations of the arthroscopic techniques: e.g., level IV study with a small number of cases, technical report, and no unified fixation materials.
K-Wire Fixation and Tension Band Wiring
In 1963, Neer3) recommended the classification system of lateral clavicle fractures and introduced transacromial K-wire fixation. Eskola et al.61) described good or satisfactory results in 22 of 23 patients; however, 26% experienced at least one complication or nonunion. In particular, migration of the K-wires into internal organs was a serious complication.62,63,64) Transacromial K-wire fixation may not be the most appropriate treatment option for patients with type 2 distal clavicle fractures. Although several studies65,66,67) reported that Knowles pin fixation provided better outcomes and lower complication rates than K-wire fixation did, threaded wires could also migrate to other internal structures.68) Therefore, the K-wire fixation method is no longer commonly used. However, Kwak et al.69) recently described a modified Neer's technique using multiple Steinmann pins and reported satisfactory results. They used multiple transacromial Steinmann pins (2.0 mm) and transcortical fixation rather than intramedullary fixation with or without interfragmentary fixation using 2.7 mm screws.
Tension band wiring has been known as a reliable method for the management of distal clavicle fractures. Several studies reported that tension band wiring could achieve good union rates and excellent clinical scores without complications.70,71) Recently, Choi et al.72) reported outcomes of 13 patients who underwent modified tension band fixation and CC fixation for Neer type 2B distal clavicle fractures. Bony union was achieved in all patients at a mean of 12.6 weeks. One patient experienced a new fracture around the holes drilled for CC fixation. Because tension band wiring is also associated with complications similar to those of transacromial K-wire fixation (K-wire migration and wire breakage), it is of paramount importance to select optimal patients and apply proper surgical techniques.
CONCLUSIONS
Distal clavicle fractures account for roughly 10%–30% of all clavicle fractures and some may be treated by conservative management. It is widely accepted, however, that unstable distal clavicle fractures require surgical treatment to obtain superior clinical outcomes (i.e., lower nonunion rates) compared to those of conservative treatment. There are many fixation options for the treatment of distal clavicle fractures, such as precontoured locking plate, hook plate, CC fixation with a screw or flexible material, arthroscopic technique, tension band wiring, and transacromial fixation. Several systematic review articles have highlighted that precontoured locking plate fixation provides better clinical scores and lower risks of complications than other fixation methods.2,73) However, to date, consensus has not been reached on which fixation method is the gold standard. Furthermore, there are no prospective randomized studies enabling a comparison of these different approaches. Therefore, surgeons should be skilled with various fixation methods and decide with their patient which approach is most appropriate for them. Further studies with high levels of evidence are needed to determine the best treatment approach for distal clavicle fractures.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19(7):392–401. doi: 10.5435/00124635-201107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Ockert B, Wiedemann E, Haasters F. Distal clavicle fractures: classifications and management. Unfallchirurg. 2015;118(5):397–406. doi: 10.1007/s00113-015-0003-1. [DOI] [PubMed] [Google Scholar]
- 3.NEER CS., 2nd Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. doi: 10.1097/00005373-196303000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 5.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23(1):44–46. doi: 10.1016/0020-1383(92)90125-c. [DOI] [PubMed] [Google Scholar]
- 6.Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture. 15 (11-21) year follow-up of 110 cases. Acta Orthop Scand. 1993;64(1):87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 7.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;(300):127–132. [PubMed] [Google Scholar]
- 8.Tsuei YC, Au MK, Chu W. Comparison of clinical results of surgical treatment for unstable distal clavicle fractures by transacromial pins with and without tension band wire. J Chin Med Assoc. 2010;73(12):638–643. doi: 10.1016/S1726-4901(10)70139-8. [DOI] [PubMed] [Google Scholar]
- 9.Robinson CM. Fractures of the clavicle in the adult: epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476–484. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 10.Craig EV. Fractures of the clavicle. In: Rockwood CA, Matsen FA, editors. The shoulder. Philadelphia: WB Saunders; 1990. pp. 1109–1193. [Google Scholar]
- 11.Allman FL., Jr Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49(4):774–784. [PubMed] [Google Scholar]
- 12.Cho CH, Kim BS, Kim DH, Choi CH, Dan J, Lee H. Distal clavicle fractures: a new classification system. Orthop Traumatol Surg Res. 2018;104(8):1231–1235. doi: 10.1016/j.otsr.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 13.Bishop JY, Jones GL, Lewis B, Pedroza A MOON Shoulder Group. Intra- and interobserver agreement in the classification and treatment of distal third clavicle fractures. Am J Sports Med. 2015;43(4):979–984. doi: 10.1177/0363546514563281. [DOI] [PubMed] [Google Scholar]
- 14.Cho CH, Oh JH, Jung GH, et al. The interrater and intrarater agreement of a modified neer classification system and associated treatment choice for lateral clavicle fractures. Am J Sports Med. 2015;43(10):2431–2436. doi: 10.1177/0363546515593949. [DOI] [PubMed] [Google Scholar]
- 15.Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002–2003;61(1-2):32–39. [PubMed] [Google Scholar]
- 16.Deafenbaugh MK, Dugdale TW, Staeheli JW, Nielsen R. Nonoperative treatment of Neer type II distal clavicle fractures: a prospective study. Contemp Orthop. 1990;20(4):405–413. [PubMed] [Google Scholar]
- 17.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86(4):778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86(7):1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91(2):447–460. doi: 10.2106/JBJS.H.00034. [DOI] [PubMed] [Google Scholar]
- 20.Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures: figure-of-eight bandage versus a simple sling. Acta Orthop Scand. 1987;58(1):71–74. doi: 10.3109/17453678709146346. [DOI] [PubMed] [Google Scholar]
- 21.Vaishya R, Vijay V, Khanna V. Outcome of distal end clavicle fractures treated with locking plates. Chin J Traumatol. 2017;20(1):45–48. doi: 10.1016/j.cjtee.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee SK, Lee JW, Song DG, Choy WS. Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics. 2013;36(6):801–807. doi: 10.3928/01477447-20130523-28. [DOI] [PubMed] [Google Scholar]
- 23.Tiren D, Vroemen JP. Superior clavicle plate with lateral extension for displaced lateral clavicle fractures: a prospective study. J Orthop Traumatol. 2013;14(2):115–120. doi: 10.1007/s10195-013-0228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin SJ, Ko YW, Lee J, Park MG. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg. 2016;25(6):942–948. doi: 10.1016/j.jse.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 25.Johnston PS, Sears BW, Lazarus MR, Frieman BG. Fixation of unstable type II clavicle fractures with distal clavicle plate and suture button. J Orthop Trauma. 2014;28(11):e269–e272. doi: 10.1097/BOT.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 26.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40(3):236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 27.Han L, Hu Y, Quan R, Fang W, Jin B, Huang L. Treatment of neer IIb distal clavicle fractures using anatomical locked plate fixation with coracoclavicular ligament augmentation. J Hand Surg Am. 2017;42(12):1036. doi: 10.1016/j.jhsa.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Seyhan M, Kocaoglu B, Kiyak G, Gereli A, Turkmen M. Anatomic locking plate and coracoclavicular stabilization with suture endo-button technique is superior in the treatment of Neer Type II distal clavicle fractures. Eur J Orthop Surg Traumatol. 2015;25(5):827–832. doi: 10.1007/s00590-015-1617-2. [DOI] [PubMed] [Google Scholar]
- 29.Asadollahi S, Bucknill A. Hook plate fixation for acute unstable distal clavicle fracture: a systematic review and meta-analysis. J Orthop Trauma. 2019;33(8):417–422. doi: 10.1097/BOT.0000000000001481. [DOI] [PubMed] [Google Scholar]
- 30.Tiren D, van Bemmel AJ, Swank DJ, van der Linden FM. Hook plate fixation of acute displaced lateral clavicle fractures: mid-term results and a brief literature overview. J Orthop Surg Res. 2012;7:2. doi: 10.1186/1749-799X-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131(4):525–533. doi: 10.1007/s00402-010-1196-y. [DOI] [PubMed] [Google Scholar]
- 32.Renger RJ, Roukema GR, Reurings JC, Raams PM, Font J, Verleisdonk EJ. The clavicle hook plate for Neer type II lateral clavicle fractures. J Orthop Trauma. 2009;23(8):570–574. doi: 10.1097/BOT.0b013e318193d878. [DOI] [PubMed] [Google Scholar]
- 33.Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33(5):1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127(3):191–194. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- 35.Tambe AD, Motkur P, Qamar A, Drew S, Turner SM. Fractures of the distal third of the clavicle treated by hook plating. Int Orthop. 2006;30(1):7–10. doi: 10.1007/s00264-005-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meda PV, Machani B, Sinopidis C, Braithwaite I, Brownson P, Frostick SP. Clavicular hook plate for lateral end fractures:- a prospective study. Injury. 2006;37(3):277–283. doi: 10.1016/j.injury.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 37.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 38.Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15(4):419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 39.Flinkkila T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J. Hook-plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop. 2006;77(4):644–649. doi: 10.1080/17453670610012737. [DOI] [PubMed] [Google Scholar]
- 40.Lee W, Choi CH, Choi YR, Lim KH, Chun YM. Clavicle hook plate fixation for distal-third clavicle fracture (Neer type II): comparison of clinical and radiologic outcomes between Neer types IIA and IIB. J Shoulder Elbow Surg. 2017;26(7):1210–1215. doi: 10.1016/j.jse.2016.11.046. [DOI] [PubMed] [Google Scholar]
- 41.Good DW, Lui DF, Leonard M, Morris S, McElwain JP. Clavicle hook plate fixation for displaced lateral-third clavicle fractures (Neer type II): a functional outcome study. J Shoulder Elbow Surg. 2012;21(8):1045–1048. doi: 10.1016/j.jse.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 42.Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84(2):184–190. doi: 10.3109/17453674.2013.786637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang C, Huang J, Luo Y, Sun H. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop. 2014;38(7):1461–1468. doi: 10.1007/s00264-014-2340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fazal MA, Saksena J, Haddad FS. Temporary coracoclavicular screw fixation for displaced distal clavicle fractures. J Orthop Surg (Hong Kong) 2007;15(1):9–11. doi: 10.1177/230949900701500103. [DOI] [PubMed] [Google Scholar]
- 45.Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28(7):693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 46.Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22(6):366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle: a report of five cases. J Bone Joint Surg Br. 1991;73(2):291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 48.Yang SW, Lin LC, Chang SJ, Kuo SM, Hwang LC. Treatment of acute unstable distal clavicle fractures with single coracoclavicular suture fixation. Orthopedics. 2011;34(6):172. doi: 10.3928/01477447-20110427-10. [DOI] [PubMed] [Google Scholar]
- 49.Mirbolook A, Sadat M, Golbakhsh M, Mousavi MS, Gholizadeh A, Saghari S. Distal clavicular fracture treatment with suture anchor method. Acta Orthop Traumatol Turc. 2016;50(3):298–302. doi: 10.3944/AOTT.2015.15.0023. [DOI] [PubMed] [Google Scholar]
- 50.Kanchanatawan W, Wongthongsalee P. Management of acute unstable distal clavicle fracture with a modified coracoclavicular stabilization technique using a bidirectional coracoclavicular loop system. Eur J Orthop Surg Traumatol. 2016;26(2):139–143. doi: 10.1007/s00590-015-1723-1. [DOI] [PubMed] [Google Scholar]
- 51.Cho CH, Jung JH, Kim BS. Coracoclavicular stabilization using a suture button device for Neer type IIB lateral clavicle fractures. J Shoulder Elbow Surg. 2017;26(5):804–808. doi: 10.1016/j.jse.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 52.Yan HW, Li L, Wang RC, et al. Clinical efficacies of coracoclavicular ligament reconstruction using suture anchor versus hook plate in the treatment of distal clavicle fracture. Orthop Traumatol Surg Res. 2017;103(8):1287–1293. doi: 10.1016/j.otsr.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 53.Hsu KH, Tzeng YH, Chang MC, Chiang CC. Comparing the coracoclavicular loop technique with a hook plate for the treatment of distal clavicle fractures. J Shoulder Elbow Surg. 2018;27(2):224–230. doi: 10.1016/j.jse.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 54.Loriaut P, Moreau PE, Dallaudiere B, et al. Outcome of arthroscopic treatment for displaced lateral clavicle fractures using a double button device. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1429–1433. doi: 10.1007/s00167-013-2772-9. [DOI] [PubMed] [Google Scholar]
- 55.Kraus N, Stein V, Gerhardt C, Scheibel M. Arthroscopically assisted stabilization of displaced lateral clavicle fractures with coracoclavicular instability. Arch Orthop Trauma Surg. 2015;135(9):1283–1290. doi: 10.1007/s00402-015-2271-1. [DOI] [PubMed] [Google Scholar]
- 56.Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for Neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132(3):399–403. doi: 10.1007/s00402-011-1455-6. [DOI] [PubMed] [Google Scholar]
- 57.Lee KW, Lee SK, Kim KJ, Kim YI, Kwon WC, Choy WS. Arthroscopic-assisted locking compression plate clavicular hook fixation for unstable fractures of the lateral end of the clavicle: a prospective study. Int Orthop. 2010;34(6):839–845. doi: 10.1007/s00264-009-0925-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pujol N, Philippeau JM, Richou J, Lespagnol F, Graveleau N, Hardy P. Arthroscopic treatment of distal clavicle fractures: a technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):884–886. doi: 10.1007/s00167-008-0578-y. [DOI] [PubMed] [Google Scholar]
- 59.Sautet P, Galland A, Airaudi S, Argenson JN, Gravier R. Arthroscopy-assisted fixation of fracture of the distal part of the clavicle by subcoracoid suture and clavicle button. Orthop Traumatol Surg Res. 2018;104(8):1237–1240. doi: 10.1016/j.otsr.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 60.Mochizuki Y, Kaneko T, Kawahara K, Toyoda S, Ikegami H, Musha Y. Outcome of arthroscopy-assisted treatment for distal clavicle fractures. Arch Orthop Trauma Surg. 2019;139(10):1393–1398. doi: 10.1007/s00402-019-03219-2. [DOI] [PubMed] [Google Scholar]
- 61.Eskola A, Vainionpaa S, Patiala H, Rokkanen P. Outcome of operative treatment in fresh lateral clavicular fracture. Ann Chir Gynaecol. 1987;76(3):167–169. [PubMed] [Google Scholar]
- 62.Regel JP, Pospiech J, Aalders TA, Ruchholtz S. Intraspinal migration of a Kirschner wire 3 months after clavicular fracture fixation. Neurosurg Rev. 2002;25(1-2):110–112. doi: 10.1007/s101430100186. [DOI] [PubMed] [Google Scholar]
- 63.Leppilahti J, Jalovaara P. Migration of Kirschner wires following fixation of the clavicle: a report of 2 cases. Acta Orthop Scand. 1999;70(5):517–519. doi: 10.3109/17453679909000992. [DOI] [PubMed] [Google Scholar]
- 64.Lyons FA, Rockwood CA., Jr Migration of pins used in operations on the shoulder. J Bone Joint Surg Am. 1990;72(8):1262–1267. [PubMed] [Google Scholar]
- 65.Wang SJ, Wong CS. Extra-articular knowles pin fixation for unstable distal clavicle fractures. J Trauma. 2008;64(6):1522–1527. doi: 10.1097/TA.0b013e3180593646. [DOI] [PubMed] [Google Scholar]
- 66.Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH. Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fracturesA prospective evaluation of 32 cases. J Trauma. 2004;56(5):1102–1105. doi: 10.1097/01.ta.0000082649.57981.f9. [DOI] [PubMed] [Google Scholar]
- 67.Jou IM, Chiang EP, Lin CJ, Lin CL, Wang PH, Su WR. Treatment of unstable distal clavicle fractures with Knowles pin. J Shoulder Elbow Surg. 2011;20(3):414–419. doi: 10.1016/j.jse.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 68.Tsai CH, Hsu HC, Huan CY, Chen HT, Fong YC. Late migration of threaded wire (schanz screw) from right distal clavicle to the cervical spine. J Chin Med Assoc. 2009;72(1):48–51. doi: 10.1016/S1726-4901(09)70021-8. [DOI] [PubMed] [Google Scholar]
- 69.Kwak SH, Lee YH, Kim DW, Kim MB, Choi HS, Baek GH. Treatment of unstable distal clavicle fractures with multiple Steinmann Pins-A modification of Neer's method: a series of 56 consecutive cases. J Orthop Trauma. 2017;31(9):472–478. doi: 10.1097/BOT.0000000000000850. [DOI] [PubMed] [Google Scholar]
- 70.Badhe SP, Lawrence TM, Clark DI. Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg. 2007;127(1):25–28. doi: 10.1007/s00402-006-0197-3. [DOI] [PubMed] [Google Scholar]
- 71.Kao FC, Chao EK, Chen CH, Yu SW, Chen CY, Yen CY. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma. 2001;51(3):522–525. doi: 10.1097/00005373-200109000-00016. [DOI] [PubMed] [Google Scholar]
- 72.Choi S, Kim SR, Kang H, Kim D, Park YG. Modified tension band fixation and coracoclavicular stabilisation for unstable distal clavicle fracture. Injury. 2015;46(2):259–264. doi: 10.1016/j.injury.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 73.Boonard M, Sumanont S, Arirachakaran A, et al. Fixation method for treatment of unstable distal clavicle fracture: systematic review and network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(6):1065–1078. doi: 10.1007/s00590-018-2187-x. [DOI] [PubMed] [Google Scholar]