Abstract
Background
Risk factors for perinatal posttraumatic stress disorder (PTSD) among parents of an infant in the NICU have varied in previous literature. The relationships between perception of illness severity and objective measures of illness severity with PTSD are not well understood.
Aims
To determine if PTSD among parents after an infant NICU discharge can be predicted by 1) objective measures of infant illness severity or 2) perceptions of infant illness severity.
Study Design
A prospective, observational study.
Subjects
Parent/infant dyads who were in the NICU for ≥ 14 days.
Outcome Measures
Objective measures of illness severity were obtained from the electronic health record. Perceptions of illness were measured by the response to the question, “How sick is your child/patient?” on a 5-point Likert scale. The Perinatal Post-Traumatic Stress Disorder Questionnaire (PPQ) was completed by parents three months after discharge.
Results
One hundred ninety-four dyads participated in the study, 86% of parents completed follow up screening. 25% of parents screened positive for PTSD. Parents perceived infants to be sick more often than hospital caregivers. In bivariate analysis many objective measures of illness severity were associated with PTSD. Parent perceptions of illness were also associated with PTSD after adjusting for objective measures of illness (OR 3.2, 95% CI 1.1–6.1, p = 0.008).
Conclusions
PTSD in parents after NICU discharge is multifactorial. Objective illness risk factors can be used to screen parents at risk. Hospital caregivers should strive to understand parents’ perception of illness and improve communication to potentially decrease PTSD after discharge.
Keywords: Perinatal PTSD, NICU, infant illness, perceptions of illness
Introduction
Post-traumatic stress disorder (PTSD) is common among parents who have had an infant in the neonatal intensive care unit (NICU). Researchers have estimated that between 18%−78% of mothers of premature infants experience at least one symptom of post-traumatic stress disorder [1]. Fathers of infants in the NICU, though less studied, have also been found to be at risk for and suffer from PTSD [2]. PTSD in parents has been shown to affect parenting behavior and child health across many pediatric populations[3][4]. Negative outcomes for infants with parents suffering from symptoms PTSD after NICU have been documented. A recent systematic review of the relationships between maternal PTSD during the perinatal period and child outcomes found maternal postpartum PTSD is associated with low infant birth weight lower rates of breast feeding [5]. Other research has found that mothers suffering from posttraumatic stress are more likely to display increased controlling patterns of interactions with their infants [6], and parents report poorer perceived infant-parent bond [8]. Parental post-traumatic stress reactions after having a premature infant have been found to mediate adverse infant outcomes such as sleeping problems in infants up to 18 months corrected gestational age (CGA) [9]. Targeting interventions to decrease symptoms of PTSD therefore has the potential to improve the health of both parents and children.
It is difficult for healthcare providers to predict which parents in the NICU will develop symptoms of PTSD. It is unclear whether an infant’s illness severity is a risk factor for the development of parental PTSD, with conflicting results from prior studies [10][11][12]. Maternal stress, which is more studied than PTSD, has been shown to not be associated with infant illness or with healthcare providers’ perceptions of infant illness, but rather with a parents’ perception of infant illness [13]. It is unknown whether parent or healthcare provider perception of illness severity are associated with the development of perinatal PTSD.
The purpose of this study was to determine whether perinatal PTSD after NICU discharge is associated with 1) objective measures of infant illness or 2) parent and healthcare provider perceptions of infant illness during the NICU stay.
Methods
This was a prospective study of parent-infant dyads in a 70-bed level IV NICU as part of a study of parent well-being during and after the NICU stay, with a primary goal to study the association between parent demographics, infant illness and subsequent healthcare utilization in relation to parent quality of life [14]. Parent-infant dyads were eligible if they were in the NICU for ≥ 14 days. Infant-parent dyads were excluded if the parents did not speak English, if the infant was not to be discharged home with their biological parent, or if the infant was previously discharged home or transferred to or from the cardiac intensive care unit for surgical intervention. Infants transferred from outside hospitals were considered if they had never been discharged home and were at least two weeks old. Infants receiving palliative care were included unless death was imminent as determined by the attending physician. If an infant died after initial enrollment the family was excluded from further interviews.
Outcomes and Measurements
The primary outcome was screening positive for perinatal PTSD, as measured by the Post-Traumatic Stress Disorder Questionnaire (PPQ) three months after NICU discharge. The PPQ is a 14-item questionnaire that assesses PTSD symptoms associated with the birth of an infant. Questions measure symptoms of intrusiveness, avoidance, hyperarousal, and feelings of guilt. Scoring is conducted on a five-point Likert scale ranging from “not at all” to “often, for more than one month” [15]. The PPQ has strong internal consistency (α =0.9) and test-retest reliabilities (r=0.92) [16]. Screening positive for PTSD was defined as a PPQ score of 19 or higher, consistent with literature suggesting that scores above 19 may warrant clinical treatment [15].
In order to measure healthcare provider and parent perceptions of illness, parents, bedside nurses, and attending physicians were asked to answer the question, “How sick is your child/patient?” on a five-point Likert scale ranging from “not sick” to “very sick.” Attending physicians and nurses were additionally asked to report their years of experience in their current role in the NICU; this response was dichotomized into <= 10 and > 10 years’ experience, to approximate the median for each group of respondents. Nurses were also asked to rate the degree to which they were familiar with the patient, which included “I care for this patient rarely,” “I know this patient moderately well,” and “I am the primary nurse for this patient.”
Parent demographic variables were collected by self-report at the time of enrollment and included relationship to infant, age, mode of delivery, insurance, race, highest level of education, lives alone, and history of either self or family mental health concerns. Variable related to infant illness severity were collected from the electronic health record and have been defined previously [14]. These variables included gestational age, birth weight, congenital anomalies, bronchopulmonary dysplasia, sepsis, intraventricular hemorrhage, necrotizing enterocolitis, periventricular leukomalacia, hypoxic ischemic encephalopathy, hydrocephalus, seizures, NICU length of stay, number of surgeries while in the NICU, number of consultations while in the NICU, behavioral health consultation, palliative care consultation, days of mechanical ventilation, vasopressors, home oxygen requirement, tracheostomy, home nasogastric feedings, gastrostomy tube, number of medications at time of discharge.
Study Procedures
The purpose of the study was explained to infants’ parents by one of two research assistants (JW and JL). Once written informed consent was obtained, the perception of infant illness severity was obtained from the parents, bedside nurses, and attending physicians on the same day as enrollment. Responses were entered by the respondent confidentially into a secure research database on a tablet [17]. All interviews among the different participants were conducted independently so as not to influence each other’s responses. Parent demographic data was also obtained by self-report.
At the time of NICU discharge, the electronic health record review was completed. Three months after discharge, parents were contacted to complete the PPQ. All parents were offered support resources for perinatal PTSD. All parents received a stipend for participation.
Statistical Analysis
Bivariate analyses were performed to evaluate which parent demographic and infant illness variables were associated with screening positive for PTSD after discharge. In order to capture the broad range of infant illness in our cohort, numeric risk scores for infant illness such as the Clinical Risk Index for Babies and Score for Neonatal Acute Physiology were considered, but were not feasible because of the number of transferred infants and term infants with complex anomalies who are not well represented by those strategies [18][19]. Instead, we created an indicator variable for the presence of at least one infant illness risk factor associated with both statistical significance in bivariate analysis and at least double the cohort baseline risk of screening positive for PTSD. We then used this infant illness indicator variable for subsequent analysis.
We used bivariate analyses to evaluate how parent, nurse and physician perceptions of illness were associated with screening positive for PTSD after discharge. Perceptions of illness responses were then dichotomized for clarity. “Not sick”, “a little sick” and “somewhat sick” were combined into the category “not sick”. “Moderately- very sick” were combined into the category “sick”. Using these dichotomous perceptions of illness variables, we evaluated whether parent perception of infant illness was associated with objective measures of infant illness severity. Differences between proportions were tested using chi-squared or Fisher’s exact tests. Differences between continuous variables were tested with Mann-Whitney U tests.
We then tested whether parent perceptions of illness were associated with nurse and physician perceptions of infant illness. We defined “agreement” between parent-nurse and parent-physician pairs in two ways: first, as responding “sick” or “not sick” similarly according to our dichotomized variable; and second, as responding within one point of each other on the 5-point Likert scale. Chi-squared tests were used to compare differences in proportions.
Finally, in order to assess how perceptions of illness severity were associated with PTSD in the setting of infant illness, we ran a multivariable logistic regression model testing the association between screening positive for PTSD and parent, nurse, and physician perceptions of illness severity, our dichotomous clinical indicator of the infant’s objective illness severity, and an interaction term between parent perception of illness and the infant-illness indicator variable. Parent history of previous mental health concerns was also added to the model, as well as any parent demographic factors associated with PTSD at p<0.2. We chose this modeling approach to be able to more directly compare the magnitude of effect of perception of illness versus objective illness; alternative models including individual illness variables associated with PTSD at p<0.2 in bivariate analysis, as well as stratifying the data by the illness indicator variable, were also considered.
A p value of <0.05 was accepted for statistical significance. Data were analyzed using STATA version 14 (College Station, TX) [20]. The study was approved by the institution’s Institutional Review Board (IRB).
Results
A total of 214 parents consented to participate. Of these, 20 were excluded from three-month follow-up because of social reasons, transfer to cardiac intensive care, or death. Of the 194 parent-infant dyads eligible for follow-up, 167 (86%) completed three-month follow up [14]. PTSD screening questions were completed by 162 of the 167 parents and were included in this analysis. The median day of life of the infant at the time of enrollment was 19 (IQR 16–39). Parent perception of illness was not associated with the day of life at assessment (Kruskal Wallis p = 0.11).
Demographic and clinical characteristics of the participants have been reported [14]. Most parents enrolled in the study were the mothers; parents reported a wide range of educational backgrounds. About 50% of parents in the study had public insurance. Among infant illness characteristics, 21% were born < 28 weeks, 30% had congenital anomalies, and 4% had hypoxic ischemic encephalopathy that required cooling. There were no statistically significant differences in parent or infant characteristics between eligible dyads lost to follow-up and those who completed follow-up.
Overall, 41/164 (25%) of parents screened positive for PTSD three months after NICU discharge. In Table 1, bivariate associations between screening positive for PTSD and demographic, infant illness, and perceptions of infant illness are displayed. Parent demographic characteristics were not significantly associated with screening positive for PTSD. Several infant illness characteristics were significantly associated with higher proportion of screening positive for perinatal PTSD. Among these, several infant illness characteristics had not only a statistically significant association, but also a clinically significant proportion ( ≥ 50%) of parents screened positive for PTSD. Fifty-five (34% of total cohort) had at least one risk factors which included gestational age of 23–25 weeks, birth weight < 1 kg, late onset sepsis, periventricular leukomalacia, hypoxic-ischemic encephalopathy, palliative care consultation, vasopressor support, and tracheostomy. For parents of infants with one of these high-risk clinical risk factors, 44% screened positive for PTSD, versus 16% of parents of infants with none of these conditions (P < 0.001).
Table 1:
Parent and infant bivariate associations with perinatal PTSD
| CHARACTERISTICS | TOTAL | SCREENED + FOR PERINATAL PTSD N (%) | P VALUE |
|---|---|---|---|
| INFANT CHARACTERISTICS | |||
| GESTATIONAL AGE AT BIRTH | 0.025 | ||
| 23–25 WEEKS | 20 | 11 (55%) | |
| 26–28 WEEKS | 16 | 3 (19%) | |
| 29–33 WEEKS | 60 | 10 (17%) | |
| 34–36 WEEKS | 29 | 7 (24%) | |
| >37 WEEKS | 39 | 10 (26%) | |
| BIRTH WEIGHT | 0.001 | ||
| < 1 KG | 28 | 14 (50%) | |
| > 1 KG | 136 | 27 (20%) | |
| BRONCHOPULMONARY DYSPLASIA (OR CHRONIC LUNG DISEASE) | 0.004 | ||
| YES | 48 | 19 (40%) | |
| NO | 114 | 21 (18%) | |
| LATE ONSET SEPSIS | <0.001 | ||
| YES | 16 | 11 (69%) | |
| NO | 148 | 30 (20%) | |
| SEVERE INTRAVENTRICULAR HEMORRHAGE | 0.043 | ||
| YES | 21 | 9 (43%) | |
| NO | 143 | 32 (22%) | |
| PERIVENTRICULAR LEUKOMALACIA | 0.102 | ||
| YES | 5 | 3 (60%) | |
| NO | 158 | 38 (24%) | |
| HYPOXIC ISCHEMIC ENCEPHALOPATHY REQUIRING COOLING | 0.035 | ||
| YES | 6 | 4 (67%) | |
| NO | 158 | 37 (23%) | |
| NICU LENGTH OF STAY | 0.001 | ||
| <28 DAYS | 43 | 3 (7%) | |
| 29–60 DAYS | 64 | 16 (25%) | |
| 61–90 DAYS | 20 | 5 (25%) | |
| >91 DAYS | 37 | 17 (46%) | |
| NUMBER OF SURGERIES WHILE IN NICU | <0.001 | ||
| <= 1 SURGERY | 126 | 23 (18%) | |
| > 1 SURGERY | 38 | 18 (47%) | |
| NUMBER OF CONSULTS WHILE IN NICU | <0.001 | ||
| <= 2 CONSULTS | 98 | 13 (13%) | |
| >2 CONSULTS | 65 | 28 (43%) | |
| DAYS ON A MECHANICAL VENTILATOR | <0.001 | ||
| 0 DAYS | 78 | 9 (12%) | |
| 1–7 DAYS | 41 | 11 (27%) | |
| >7 DAYS | 44 | 21 (48%) | |
| REQUIRED PRESSORS | <0.001 | ||
| YES | 27 | 14 (52%) | |
| NO | 137 | 27 (20%) | |
| TRACHEOSTOMY | 0.044 | ||
| YES | 9 | 5 (56%) | |
| NO | 155 | 36 (23%) | |
|
| |||
| “HIGH-RISK” INFANT CHARACTERISTICS | |||
| YES | 55 | 24 (44%) | <0.001 |
| NO | 109 | 17 (16%) | |
|
| |||
| PARENT CHARACTERISTICS | |||
| PARENT LIVES ALONE | 0.072 | ||
| Yes | 10 | 5 (50%) | |
| No | 154 | 36 (23%) | |
| HISTORY OF MENTAL HEALTH CONCERNS | 1 | ||
| YES | 54 | 14 (26%) | |
| NO | 108 | 27 (25%) | |
-Table 1 shows infant and parent characteristics associated with parents screening positive for PTSD 3 months after discharge. “High-risk” infant characteristics were defined as any individual infant characteristic associated with parents having at least twice the total study group proportion of screening positive for PTSD. These included: birth at 23–25 weeks gestation, birth weight < 1 kg, late onset sepsis, PVL, HIE requiring whole body cooling, palliative care consultation, vasopressor support, and tracheostomy.
The following variables were not statistically significantly associated with screening positive for PTSD: # of siblings to the infant, access to a car, family staying at Ronald McDonald House/family lives a significant distance from the hospital, Fetal Concerns Care prior to delivery, infant gender, multiple gestation, retinopathy of prematurity, patent ductus arteriosus, early-onset sepsis, grade of IVH, pulmonary hypertension, monitor at the time of discharge
Perceived greater illness severity was associated with higher proportion of parents screening positive for PTSD. Table 2 shows the distribution of parents, nurses, and doctors who rated the infant as “sick.” Parent perception of illness was associated with objective measures of infant illness. Parents were more likely to report their infant as sick if their infant was born at an earlier gestational age, lower birthweight, moderate-severe bronchopulmonary dysplasia, grade 3–4 intraventricular hemorrhage, hypoxic ischemic encephalopathy requiring whole body cooling, palliative care consultation, required pressor support, or received a tracheostomy (supplemental Table 3). Other than being a single parent, demographic risk factors were not associated with differences in parental perception of illness.
Table 2:
Distributions of parents/nurses/MD who rated infant as sick
| PERCEPTION OF ILLNESS | TOTAL | SCREEN + FOR PERINATAL PTSD | P VALUE |
|---|---|---|---|
| 5-POINT LIKERT SCALE | |||
| PARENT RESPONSE | <0.001 | ||
| NOT AT ALL SICK | 49 | 5 (10%) | |
| A LITTLE SICK | 34 | 6 (18%) | |
| SOMEWHAT SICK | 38 | 9 (24%) | |
| MODERATELY SICK | 33 | 14 (42%) | |
| VERY SICK | 8 | 6 (75%) | |
| MD RESPONSE | 0.029 | ||
| NOT AT ALL SICK | 43 | 6 (14%) | |
| A LITTLE SICK | 65 | 14 (22%) | |
| SOMEWHAT SICK | 21 | 5 (24%) | |
| MODERATELY SICK | 27 | 12 (44%) | |
| VERY SICK | 6 | 3 (50%) | |
| RN RESPONSE | 0.003 | ||
| NOT AT ALL SICK | 45 | 5 (11%) | |
| A LITTLE SICK | 55 | 11 (20%) | |
| SOMEWHAT SICK | 38 | 14 (37%) | |
| MODERATELY SICK | 21 | 8 (38%) | |
| VERY SICK | 4 | 3 (75%) | |
|
| |||
| BINARY VARIABLE | |||
| PARENT RESPONSE | <0.001 | ||
| NOT SICK | 121 | 20 (17%) | |
| SICK | 41 | 20 (49%) | |
| MD RESPONSE | 0.002 | ||
| NOT SICK | 129 | 25 (19%) | |
| SICK | 33 | 15 (45%) | |
| RN RESPONSE | 0.018 | ||
| NOT SICK | 138 | 30 (22%) | |
| SICK | 25 | 11 (44%) | |
Table 2 shows bivariate associations between parent, physician and nurse perceptions of infant illness and parents’ screening positive for perinatal PTSD. The top half of the table displays the full 5-point Likert scale; the bottom half of the table displays the dichotomized version where “not sick” = “not at all sick,” “a little sick,” or “somewhat sick.”
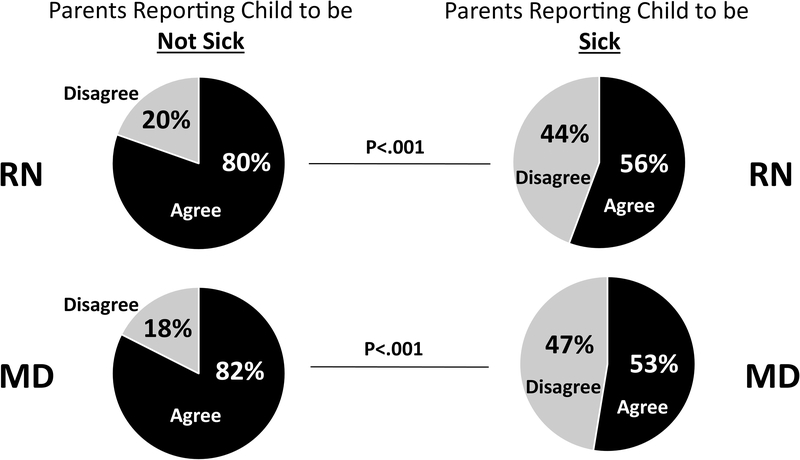
In Figure 1, the association of parent perception of infant illness with physician and nurse perceptions of infant illness is displayed. When parents perceived the infant to be “not sick”, nurses and physicians agreed with parents 85% and 86% of the time, respectively. Conversely, when parents perceived their infant to be “sick”, nurses and physicians agreed with this assessment only 41% and 43% of the time, respectively. This pattern was the same when “agreement” was defined as no more than 1-point difference on the 5-point Likert scale.
Figure 1. Parent-physician and parent-nurse agreement in perception of illness severity.
Figure 1 shows the proportion of physicians and nurses that agree with parent responses to the question “How sick is your child/patient?” Responses were dichotomized from the original 5-point Likert scale such that “not sick” = “not at all sick,” “a little sick,” or “somewhat sick;” “sick” = “moderately sick” or “very sick.”
In Table 4, a multivariable model of risk factors associated with perinatal PTSD is displayed. Parents whose infants were clinically assessed to be “sick” and who also perceived their infant to be “sick” had 3 times the odds of screening positive for perinatal PTSD, adjusted for parents’ previous history of mental health concerns and respondent being a single parent. Neither physician nor nurse perception of infant illness severity were associated with perinatal PTSD. The day of life, ventilation, and feeding status at the time of assessment of perception of illness assessment were tried in the models but were not significant and did not change the relationships between perception of illness and subsequently screening positive for PTSD. Nearly identical results were found with alternative modeling strategies including an analysis stratified by illness and another model including individual illness variables rather than an indicator variable.
Table 4:
Multivariable model
| VARIABLE | ODDS RATIO | 95% CI | P VALUE |
|---|---|---|---|
| CLINICAL ILLNESS INDICATOR | |||
| YES | 3.1 | 1.1 – 9.0 | 0.040 |
| NO | 1.0 | ||
| PARENT PERCEIVES “SICK” | |||
| YES | 3.8 | 1.2 – 12.6 | 0.027 |
| NO | 1.0 | ||
| INTERACTION BETWEEN CLINICAL ILLNESS / PARENT PERCEIVES “SICK” | |||
| YES | 0.7 | 0.1 – 3.9 | 0.696 |
| NO | 1.0 | ||
| RN PERCEIVES “SICK” | |||
| YES | 1.0 | 0.3 – 3.4 | 0.999 |
| NO | 1.0 | ||
| MD PERCEIVES “SICK” | |||
| YES | 1.7 | 0.6 – 5.1 | 0.355 |
| NO | 1.0 | ||
| HISTORY OF PREVIOUS MENTAL HEALTH CONCERNS | |||
| YES | 0.9 | 0.4 – 2.1 | 0.767 |
| NO | 1.0 | ||
| SINGLES PARENT | |||
| YES | 1.7 | 0.4 – 8.0 | 0.510 |
| NO | 1.0 |
Table 4 shows a multivariable logistic regression model of infant illness and perceptions of infant illness, as well as an interaction term between parent perceived illness and objective infant illness. “High risk” infant characteristics are defined as any infant clinical characteristic associated with parents having more than twice the baseline proportion of screening positive for PTSD, and included: birth at 23–25 weeks gestation, birth weight < 1 kg, late onset sepsis, PVL, HIE requiring whole body cooling, palliative care consultation, vasopressor support, and tracheostomy. Parent, nurse and physician perceived as “sick” was defined as responding to he question “How sick is your child/patient?” on a 5-point Likert scale as “moderately – very sick”.
Discussion
This study’s goal was to examine the relationships between both objective measures of infant illness severity and perceptions of illness severity with the risk for perinatal PTSD in parents who have had an infant in the NICU. We found that many objective measures of infant illness severity are both statistically and clinically significant risk factors for perinatal PTSD in parents after having an infant in the NICU. We also found that parent perceptions of infant illness severity correlated with increased risk for perinatal PTSD when assessed three months after their infant’s discharge, adjusted for objective measures of infant illness.
Twenty-five percent of parents in this study screened positive for PTSD three months after NICU discharge. These results are comparable to previous studies of parents with infants in the NICU [21]. Psychosocial support systems for parents in the NICU are increasingly recognized as essential to providing holistic care. Notably, this study was conducted in a single-room NICU with a broad range of support systems including faculty psychologists, social workers, and a family support coordinator. While these support systems continue to offer vital services to NICU families, our findings suggest that parents with infants in the NICU continue to be at risk for adverse mental health outcomes. We identified a number of objective measures of infant illness severity that were associated with parents screening positive for PTSD. More than 50% of parents whose infants were born 23–25 weeks, birth weight < 1 kg, with late onset sepsis, periventricular leukomalacia, hypoxic-ischemic encephalopathy, palliative care consultation, vasopressor support, or tracheostomy screened positive for PTSD. Our results may differ from previous studies on infant illness severity and PTSD secondary to the clinical makeup of the NICU in which the study was conducted. Identifying statistically independent clinical risk factors was difficult due to the small number of infants with some risk factors and the collinearity of many clinical risks. Nonetheless, these risk factors have something qualitatively in common with each other: parents have experienced an infant with critical illness, its associated clinical interventions, and difficult conversations. Ideally, policies and procedures should be developed and implemented to ensure parents in the NICU are universally screened for symptoms of PTSD, depression, and anxiety [22]. However, given the varying sizes and resources available to NICUs, universal screening is often difficult and not fully implemented. Our findings can be used to help target screening and interventions to parents at highest risk for developing perinatal PTSD after discharge from the NICU. Utilization of previously researched interventions and standards of care to decrease parental distress allows healthcare providers the ability to begin offering services to families at risk [23] [24].
We found that parent perception of infant illness was significantly associated with screening positive for PTSD. Parents were more likely to perceive their infants as sick than the physicians and nurses caring for their infants. This is in contrast to previous research that found mothers in the NICU more often perceive their infants to be less sick than healthcare providers [25]. Differences in illness perceptions have been reported between healthcare providers and patients in previous literature [26] [27]. Furthermore, the relationship between PTSD and illness perception has been described in other populations [28]. This study is the first to identify a relationship between parent perception of illness and perinatal PTSD after discharge. Perinatal PTSD is detrimental to infant, parent and family health. The disconnect between NICU caregivers and parent perceptions of illness suggests a potential opportunity for healthcare providers to improve the wellbeing of parents in the NICU. It is imperative for healthcare providers to understand parents’ perceptions of illness in order to have meaningful and therapeutic conversations with parents about the health status of their infants. While hospital caregivers are not always able to influence infant illness severity, they are able to support parents in their formation of perception of illness and understanding of their NICU experience [29]. This is not to suggest there should be a minimization of parental perceptions or that parents’ perceptions should align with those of the healthcare caregivers. Rather, we suggest that work should focus on helping parents create a narrative of their infant’s illness that makes sense and is manageable [30] [31]. Further interventions also need to be developed to support providers in this endeavor.
Additionally, it is notable that 10% of parents did not perceive their infants as “sick” yet screened positive for PTSD. This indicates that PTSD in parents in the NICU is multifactorial. It must be considered that PTSD in this population may arise from previously documented risk factors such as reproductive variables, lack of support, or the coexistence of postpartum depression and/or acute stress disorder [32] [33][7][34].
There are several limitations to this study. Although a wide range of parent demographic and infant illness were represented, this was a single-center study with English speaking only patients, which may limit the generalizability of our findings. A validated illness risk score was not feasible in our patient population which includes transferred patients and term infants with anomalies, which made categorization of objective illness severity more difficult. Another limitation was the use of a single question to measure perception of infant illness severity; we chose this approach to align parent responses with nurse and physician responses but did not measure how or why these perceptions were constructed. Parent and family mental health history was assessed using a broad single self-report question; this was limited in scope secondary to the primary study goals of the primary study [14]. In future work it will be important to examine which components of prenatal physical and mental well-being are most predictive of perinatal PTSD symptoms. Finally, this study did not examine secondary PTSD in healthcare providers. Previous research tells us that nurses and physicians are at risk for secondary PTSD related to their work environments which may lead increased compassion fatigue [35]. Secondary PTSD has been found to adversely impact hospital caregivers work and personal lives [36] and the possibility that this influences perception of illness severity was not studied.
Conclusion
Perinatal PTSD after having an infant in the NICU is associated with both infant illness severity and parental perception of infant illness severity. Hospital caregivers in the NICU should work to identify parents at highest risk for PTSD after NICU discharge and ensure access to appropriate services and care while both in the NICU and after hospital discharge. Future studies of how parents form their perceptions of infant illness would support intervention development.
Supplementary Material
Table 3:
Associations between parent perception of illness and objective illness of infant
| CHARACTERISTICS | TOTAL | PARENT REPORTED AS “SICK” N (%) | P VALUE |
|---|---|---|---|
| INFANT CHARACTERISTICS | |||
| GESTATIONAL AGE AT BIRTH | 0.024 | ||
| 23–25 WEEKS | 19 | 10 (53%) | |
| 26–28 WEEKS | 16 | 4 (25%) | |
| 29–33 WEEKS | 10 | 11 (18%) | |
| 34–36 WEEKS | 29 | 4 (14%) | |
| >37 WEEKS | 38 | 12 (32%) | |
| BIRTH WEIGHT | 0.003 | ||
| < 1 KG | 27 | 13 (48%) | |
| > 1 KG | 135 | 28 (21%) | |
| BRONCHOPULMONARY DYSPLASIA & SEVERITY | 0.006 | ||
| NONE/MILD | 113 | 22 (19%) | |
| MODERATE/SEVERE | 47 | 19 (40%) | |
| LATE ONSET SEPSIS | 0.169 | ||
| YES | 15 | 6 (40%) | |
| NO | 147 | 35 (24%) | |
| INTRAVENTRICULAR HEMORRHAGE | <0.001 | ||
| YES | 21 | 12 (57%) | |
| NO | 141 | 29 (21%) | |
| PERIVENTRICULAR LEUKOMALACIA | 0.072 | ||
| YES | 5 | 3 (60%) | |
| NO | 156 | 38 (24%) | |
| HYPOXIC ISCHEMIC ENCEPHALOPATHY REQUIRING COOLING | 0.643 | ||
| YES | 6 | 2 (33%) | |
| NO | 156 | 39 (25%) | |
| NICU LENGTH OF STAY | 0.001 | ||
| <28 DAYS | 43 | 3 (7%) | |
| 29–60 DAYS | 63 | 17 (27%) | |
| 61–90 DAYS | 20 | 5 (25%) | |
| >91 DAYS | 36 | 16 (44%) | |
| NUMBER OF SURGERIES WHILE IN NICU | <0.001 | ||
| <= 1 SURGERY | 125 | 23 (18%) | |
| > 1 SURGERY | 37 | 18 (49%) | |
| NUMBER OF CONSULTS WHILE IN NICU | <0.001 | ||
| <=2 CONSULTS | 98 | 14 (13%) | |
| >2 CONSULTS | 63 | 27 (43%) | |
| DAYS ON A MECHANICAL VENTILATOR | <0.001 | ||
| 0 DAYS | 78 | 7 (9%) | |
| 1–7 DAYS | 41 | 11 (27%) | |
| >7 DAYS | 42 | 22 (52%) | |
| REQUIRED PRESSORS | 0.043 | ||
| YES | 27 | 11 (41%) | |
| NO | 135 | 30 (22%) | |
| TRACHEOSTOMY | 0.009 | ||
| YES | 9 | 6 (67%) | |
| NO | 153 | 35 (23%) | |
|
| |||
| “HIGH-RISK” INFANT CHARACTERISTICS | <0.001 | ||
| YES | 78 | 36 (46%) | |
| NO | 134 | 23 (17%) | |
|
| |||
Table 3 shows associations between infant illness variables and parent perceptions of illness. Parent perception of illness was rated on a 5-point Likert scale and then dichotomized for clarity. “Not sick”, “a little sick”, and “somewhat sick” were combined in the category “not sick”. “Moderately-very sick” were combined in the category “sick”. “High-risk” infant characteristics are defined in Table 1 as any infant illness characteristic associated with at least twice the study cohort proportion of parents screening positive for PTSD; these characteristics included: birth at 23–25 weeks gestation, birth weight < 1 kg, late onset sepsis, PVL, HIE requiring whole body cooling, palliative care consultation, vasopressor support, and tracheostomy.
-P- values were calculated using chi-squared or Fisher’s exact tests.
Highlights.
Many objective measures of infant illness severity are both statistically and clinically significant risk factors for perinatal PTSD in parents after having an infant in the NICU.
Parent perception of infant illness severity correlates with increased risk for perinatal PTSD in parents after having an infant in the NICU after adjusting for objective measures of infant illness severity.
The disconnect between NICU caregivers and parent perception of illness suggests there is opportunity for healthcare providers to improve the wellbeing of parents in the NICU.
Acknowledgments
Funding: This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, [grant number UL1TR001436], and MCW Presidential Faculty Scholar Award [JL].
Footnotes
Declarations of interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Gondwe KW, Holditch-Davis D, Posttraumatic stress symptoms in mothers of preterm infants, Int. J. Africa Nurs. Sci 3 (2015) 8–17. doi: 10.1016/j.ijans.2015.05.002. [DOI] [Google Scholar]
- [2].Aftyka A, Rybojad B, Rozalska-Walaszek I, Rzoñca P, Humeniuk E, Post-traumatic stress disorder in parents of children hospitalized in the neonatal intensive care unit (NICU): Medical and demographic risk factors, Psychiatr. Danub 26 (2014) 347–352. [PubMed] [Google Scholar]
- [3].Petit A, A., Eutrope J,Thierry A, Bednarek N, Aupetit L, Saad S, Vulliez L, Sibertin-Blanc D,Nezelof S, Rolland, Mother’s emotional and posttraumatic reactions after a preterm birth: The mother-infant interaction is at stake 12 months after birth, PLoS One. 11 (2016) 1–14. doi: 10.1371/journal.pone.0151091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Davidson JE, Jones C, Bienvenu OJ, Family response to critical illness: Postintensive care syndrome-family, Crit. Care Med 40 (2012) 1–7. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- [5].Cook N, Ayers S, Horsch A, Maternal posttraumatic stress disorder during the perinatal period and child outcomes: A systematic review, J. Affect. Disord (2018) 18–31. doi: 10.1016/j.jad.2017.07.045. [DOI] [PubMed] [Google Scholar]
- [6].Forcada-Guex M, Borghini A, Pierrehumbert B, Ansermet F, Muller-Nix C, Prematurity, maternal posttraumatic stress and consequences on the mother–infant relationship ☆, Early Hum. Dev 87 (2011) 21–26. doi: 10.1016/j.earlhumdev.2010.09.006. [DOI] [PubMed] [Google Scholar]
- [7].Beck CT, Gable RK, Sakala C, Declercq ER, Posttraumatic Stress Disorder in New Mothers: Results from a Two-Stage U.S. National Survey, Birth. 38 (2011) 216–227. doi: 10.1111/j.1523-536X.2011.00475.x. [DOI] [PubMed] [Google Scholar]
- [8].Parfitt YM, Ayers S, The effect of post-natal symptoms of post-traumatic stress and depression on the couple’s relationship and parent-baby bond, J. Reprod. Infant Psychol 27 (2009) 127–142. doi: 10.1080/02646830802350831. [DOI] [Google Scholar]
- [9].Pierrehumbert B, Nicole A, Muller-Nix C, Forcada-Guex M, Ansermet F, Parental post-traumatic reactions after premature birth: implications for sleeping and eating problems in the infant, Arch. Dis. Child. - Fetal Neonatal Ed 88 (2003) F400–F404. doi: 10.1136/fn.88.5.F400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chang H-P, Chen J-Y, Huang Y-H, Yeh C-J, Huang J-Y, Su P-H, Chen VC-H, Factors Associated with Post-Traumatic Symptoms in Mothers of Preterm Infants, Arch. Psychiatr. Nurs 30 (2016) 96–101. doi: 10.1016/j.apnu.2015.08.019. [DOI] [PubMed] [Google Scholar]
- [11].Feeley N, Zelkowitz P, Cormier C, Charbonneau L, Lacroix A, Papageorgiou A, Posttraumatic stress among mothers of very low birthweight infants at 6 months after discharge from the neonatal intensive care unit, Appl. Nurs. Res 24 (2011) 114–117. doi: 10.1016/j.apnr.2009.04.004. [DOI] [PubMed] [Google Scholar]
- [12].Shaw RJ, Lilo E, Benitz W, Storfer-Isser A, Ball MB, Proud M, Vierhaus NS, Huntsberry A, Mitchell K, Adams MM, Horwitz SM, SCREENING FOR SYMPTOMS OF POSTPARTUM TRAUMATIC STRESS IN A SAMPLE OF MOTHERS WITH PRETERM INFANTS, Issues Ment. Heal. Nurs. 35 (2014) 198–207. doi: 10.3109/01612840.2013.853332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Brooks S, Rowley S, Broadbent E, Petrie KJ, Illness perception ratings of high-risk newborns by mothers and clinicians: Relationship to illness severity and maternal stress., Heal. Psychol (2012). doi: 10.1037/a0027591. [DOI] [PubMed] [Google Scholar]
- [14].McAndrew J, S., Acharya K, Westerdahl J, Brousseau D, Panepinto J, Simpson P, Leuthner J, & Lagatta A prospective study of parent health-related quality of life before and after NICU discharge, J. Pediatr (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Callahan JL, Borja SE, Hynan MT, Modification of the Perinatal PTSD Questionnaire to enhance clinical utility, J. Perinatol 26 (2006) 533–539. doi: 10.1038/sj.jp.7211562. [DOI] [PubMed] [Google Scholar]
- [16].M.R.L., DeMier RL, Hynan MT, Harris HB, Perinatal stressors as predictors of symptoms of posttraumatic stress in mothers of infants at high risk., J. Perinatol. 16 (1996) 276–280. [PubMed] [Google Scholar]
- [17].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support, J. Biomed. Inform 42 (2009) 377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Network TIN, The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. The International Neonatal Network., Lancet (London, England). 342 (1993) 193–8. doi: 10.1016/0140-6736(93)92296-6. [DOI] [PubMed] [Google Scholar]
- [19].Harsha SS, Archana BR, SNAPPE-II (score for neonatal acute physiology with perinatal extension-II) in predicting mortality and morbidity in NICU, J. Clin. Diagnostic Res 19 (2015) SC10–SC12. doi: 10.7860/JCDR/2015/14848.6677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC, (n.d.). [Google Scholar]
- [21].Hynan M, Mounts K, Vanderbilt D, Screening parents of high-risk infants for emotional distress: rationale and recommendations, J. Perinatol 3372 (2013) 748–753. doi: 10.1038/jp.2013.72. [DOI] [PubMed] [Google Scholar]
- [22].Shaw RJ, Lilo EA, Storfer-Isser A, Ball MB, Proud MS, Vierhaus NS, Huntsberry A, Mitchell K, Adams MM, Horwitz SM, Screening for symptoms of postpartum traumatic stress in a sample of mothers with preterm infants, Issues Ment. Health Nurs 35 (2014) 198–206. doi: 10.3109/01612840.2013.853332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Shaw RJ, Sweester CJ, John NS, Lilo E, Corcoran JB, Jo B, Howell SHK, Benitz WE, Feinstein N, Melnyk B, Horwitz SM, Prevention of Postpartum Traumatic Stress in Mothers with Preterm Infants: Manual Development and Evaluation, Issues Ment. Heal. Nurs. Issues Ment Heal. Nurs Downloaded from Informahealthcare.Com by Stanford Univ 34 (2013) 578–586. doi: 10.3109/01612840.2013.789943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jotzo M, Poets CF, Helping Parents Cope With the Trauma of Premature Birth: An Evaluation of a Trauma-Preventive Psychological Intervention, Pediatr.. 115 (2005) 915–919. doi: 10.1542/peds.2004-0370. [DOI] [PubMed] [Google Scholar]
- [25].De Wit S, Donohue PK, Shepard J, Boss RD, Mother-clinician discussions in the neonatal intensive care unit: Agree to disagree, J. Perinatol 33 (2013) 278–281. doi: 10.1038/jp.2012.103. [DOI] [PubMed] [Google Scholar]
- [26].Petrie KJ, Jago LA, Devcich DA, The role of illness perceptions in patients with medical conditions, Curr Opin Psychiatry Curr. Opin. Psychiatry 20 (2007) 163–167. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- [27].Petrie KJ, Weinman J, Patients’ perceptions of their illness: The dynamo of volition in health care, Curr. Dir. Psychol. Sci 21 (2012) 60–65. doi: 10.1177/0963721411429456. [DOI] [Google Scholar]
- [28].Sheldrick R, Tarrier N, Berry E, Kincey J, Post-traumatic stress disorder and illness perceptions over time following myocardial infarction and subarachnoid haemorrhage, Br. J. Health Psychol 11 (2006) 387–400. doi: 10.1348/135910705X71434. [DOI] [PubMed] [Google Scholar]
- [29].Janvier A, Lantos J, Aschner J, Barrington K, Batton B, Batton D, Berg SF, Carter B, Campbell D, Cohn F, Lyerly AD, Ellsbury D, Fanaroff A, Fanaroff J, Fanaroff K, Gravel S, Haward M, Kutzsche S, Marlow N, Montello M, Maitre N, Morris JT, Paulsen OG, Prentice T, Spitzer AR, Stronger and More Vulnerable: A Balanced View of the Impacts of the NICU Experience on Parents, Pediatrics. 138 (2016) e20160655–e20160655. doi: 10.1542/peds.2016-0655. [DOI] [PubMed] [Google Scholar]
- [30].Kadivar M, Seyedfatemi N, Akbari N, Haghani H, The effect of narrative writing on maternal stress in neonatal intensive care settings, J. Matern. Neonatal Med 28 (2015) 938–943. doi: 10.3109/14767058.2014.937699. [DOI] [PubMed] [Google Scholar]
- [31].Horsch A, Tolsa JF, Gilbert L, du Chêne LJ, Müller-Nix C, Graz MB, Improving Maternal Mental Health Following Preterm Birth Using an Expressive Writing Intervention: A Randomized Controlled Trial, Child Psychiatry Hum. Dev 47 (2016). doi: 10.1007/s10578-015-0611-6. [DOI] [PubMed] [Google Scholar]
- [32].Greene MM, Rossman B, Patra K, Kratovil AL, Janes JE, Meier PP, Depression, Anxiety, and Perinatal-Specific Posttraumatic Distress in Mothers of Very Low Birth Weight Infants in the Neonatal Intensive Care Unit, J. Dev. Behav. Pediatr. 36 (2015) 362–370. doi: 10.1097/DBP.0000000000000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lefkowitz J, DS., Baxt C, & Evans, Prevalence and Correlates of Posttraumatic Stress and Postpartum Depression in Parents of Infants in the Neonatal Intensive Care Unit (NICU), J. Clin. Psychol. Med. Settings 17 (2010) 230–237. doi: 10.1007/s10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- [34].Shaw RJ, Bernard RS, DeBlois T, Ikuta LM, Ginzburg K, Koopman C, The Relationship Between Acute Stress Disorder and Posttraumatic Stress Disorder in the Neonatal Intensive Care Unit, Psychosomatics. 50 (2009) 131–137. doi: 10.1176/appi.psy.50.2.131. [DOI] [PubMed] [Google Scholar]
- [35].Meadors P, Lamson A, Swanson M, White M, Sira N, Secondary traumatization in pediatric healthcare providers: Compassion fatigue, burnout, and secondary traumatic stress, Omega J. Death Dying 60 (2010) 103–128. doi: 10.2190/OM.60.2.a. [DOI] [PubMed] [Google Scholar]
- [36].Czaja AS, Moss M, Mealer M, Symptoms of Posttraumatic Stress Disorder Among Pediatric Acute Care Nurses, J. Pediatr. Nurs 27 (2012) 357–365. doi: 10.1016/j.pedn.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.