Abstract
Objective:
To improve our understanding of timely access to urologic care, we leveraged driving time combined with a measure of urologist density.
Materials and Methods:
We identified all urologists who billed Medicare using National Provider Identifier in 2015 and geocoded their practice location. We developed drive-time based service areas for each provider using Esri’s street network dataset stratified into 30, 60, 90, and 120-minute areas. Population characteristics were aggregated and block groups were assigned to a Hospital Referral Region.
Results:
We identified 10,170 urologists that billed Medicare in 2015 in the United States. Compared to the northeast, vast expanses of land across the western US have drive times to urology care >60 minutes. However, less than 13% of the US population is unable to obtain urologic care within 30 minutes. Likely reflecting rural populations, White and American Indian populations are represented in greater proportion among those requiring a longer drive time to urologic care. Disparities were noted between areas with timely access to a high versus low density of urologists; low density areas have a greater proportion of Black and Asian populations and greater income inequality.
Conclusions:
Drive time to urologists combined with urologist density is a novel approach to investigating urologic care access and a tool for health disparities research. While almost all of the US population lives within one-hour drive time to a urologist there remains important differences in the population severed by high compared to low provider density.
Keywords: Health Services, Work Force, Health Disparities, Urologic Care
Introduction
Sociodemographic disparities in access to urologic care are frequently documented, with racial differences in screening, treatment, and survival from urologic cancers, as well as other urologic conditions.1–3 The factors driving these disparities are complex and include differences in resource allocation, access to care, delivery of care, quality of care, and physician-patient interactions. While access to care is a multidimensional construct, one of the most important barriers to care may be physical distance.
Distance to medical treatment is likely an important health determinant and has been defined as the distance decay effect; patients that live further from their medical treatment have worse outcomes.4 Patients also attend significantly fewer follow up visits the farther they must travel for care.5, 6 Furthermore, distance appears to intensify the negative effects of other aspects of health care access or scarcity.7
To date, analyses used to identify geographic disparities in access to urologic care have largely focused on county level provider analyses.8, 9 Such work has found that counties without urologic care have increased prostate, bladder, and kidney cancer mortality, and men with localized prostate cancer from rural counties are less likely to be treated compared to men from metropolitan counties.1, 9, 10 However, county-level analyses do not take into account where patients live or the influence of transportation times to care. As a result, such research is unable to adequately characterize areas with limited access to urologic care.
The ability for patients to make choices about the providers they see is an additional important component in access to care. Up to 30% of patients seek a second opinion for a variety of reasons including communication problems, concerns about the quality of care received, and issues surrounding insurance coverage.11, 12 Secondary reviews of pathology and radiologic images, which may come during a second opinion, also commonly result in substantial diagnostic changes.13, 14 In addition, a growing body of work suggests that when providers lack competition in the marketplace, they charge higher prices and have worse outcomes.15–17
To improve our understanding of timely access to urologic care, we leveraged driving time to care combined with a measure of urologist density to examine population disparities. We hypothesize that substantial population level disparities remain in timely access to urologic care.
Methods
We identified all practicing urologists who bill Medicare using National Provider Identifier in 2015 and geocoded their practice location. Providers who graduated from medical school in the last 5 years were excluded as they were likely to be in training. Street address based geocoding was constructed for all providers with street level address information matched to Environmental Systems Research Institute (Esri) national geocode locators. If street level information was absent, zip code information was used for geocoding. For providers with multiple practice locations, urologists were down-weighted by the inverse of the number of practicing locations.
We developed drive-time based service areas for each provider using Esri’s street network dataset stratified into 30, 60, 90, and 120-minute areas. We did not constrain drive time areas by geographic boundary, allowing them to cross county and state lines. Drive times incorporated traffic data. These drive time areas were then intersected with population centroids of the 2010 US census populated census block groups. We selected block group characteristics for individuals 65 years or older for the contiguous United States. We examined differences by race (White, Black, American Indian, Asian, Pacific Islander, Other, and Multiple Races), ethnicity (Hispanic, Non-Hispanic), age (65-74 years, 75-84 years, 85+ years), and income (top 10% of median household income for all block groups, bottom 10% of median household income for all block groups).
For visualization purposes and the construction of our urologic density variable, each block group was assigned to a Hospital Referral Region (HRR) and population characteristics were aggregated by HRR. Dartmouth atlas constructed HRRs to identify geographic boundaries within which patients are likely to seek tertiary-level care. Use of HRR is likely to be a better representation for meaningful geographic boundaries for urologic care than zip code level or county estimates.9, 18 Urologic density was defined as the ratio of the population over age 65 to the number of urologists in an area.
Results
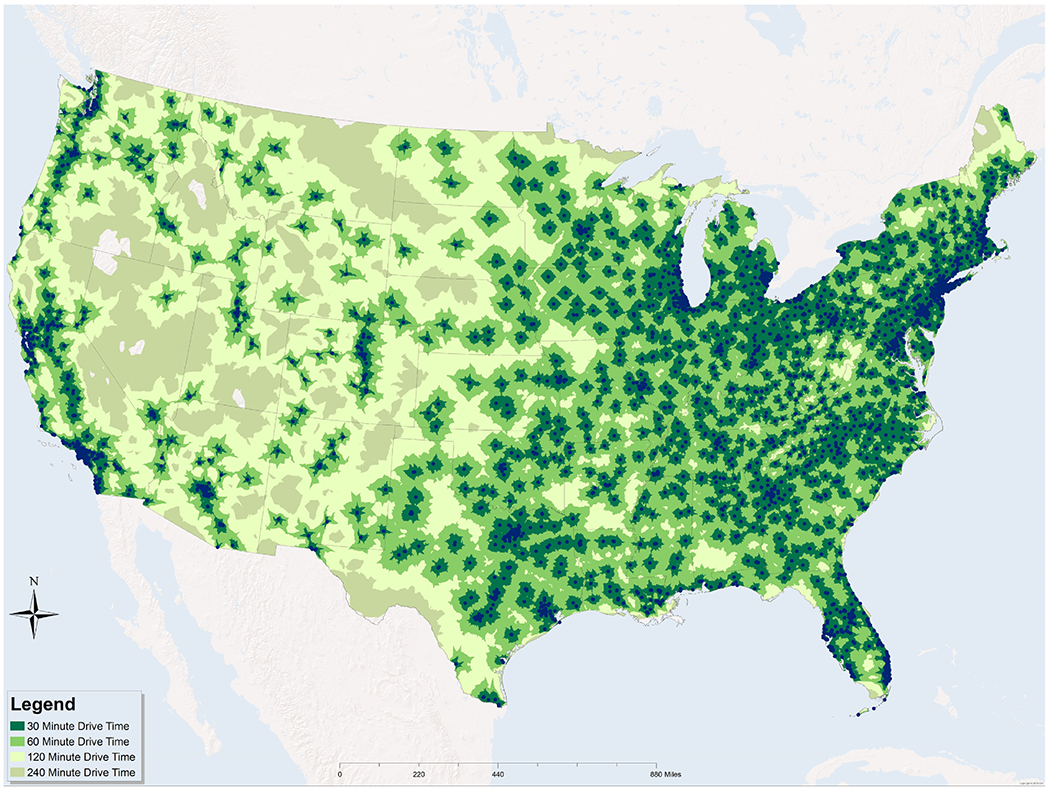
We identified 10,170 urologists that billed Medicare in 2015 and whose primary practice was located within the contiguous United States. There are substantial differences in drive time to urology care across the US (Figure 1). Vast expanses of land across the western US have drive times to urology care >60 minutes compared to predominantly shorter times in the northeastern US. However, when considering population density, less than 3% of patients have a drive time to urologic care of over one hour while over 87% can obtain access within 30 minutes (Table 1).
Figure 1.
Drive time to US urologists grouped by Hospital Referral Region.
Note: Blue dots represent individual urologist practice locations.
Table 1:
Percentage of Population over 65 by Drive Time
| Within 30 min | Between 30 and 60 | Outside 60 min | ||||
|---|---|---|---|---|---|---|
| Absoloutea | Relativeb | Absoloutea | Relativeb | Absoloutea | Relativeb | |
| Total | 87.47 | 10.28 | 2.25 | |||
| Race | ||||||
| White | 72.48 | 82.87 | 9.38 | 91.07 | 1.81 | 80.44 |
| Black | 8.21 | 9.39 | 0.59 | 5.73 | 0.05 | 2.22 |
| American Indian | 0.35 | 0.40 | 0.10 | 0.97 | 0.07 | 3.11 |
| Asian | 3.60 | 4.12 | 0.04 | 0.39 | 0.21 | 9.33 |
| Pacific Islander | 0.06 | 0.07 | 0.00 | 0.00 | 0.02 | 0.89 |
| Other | 1.74 | 1.99 | 0.09 | 0.87 | 0.03 | 1.33 |
| Multiple Races | 1.02 | 1.17 | 0.10 | 0.97 | 0.06 | 2.67 |
| Ethnicity | ||||||
| Hispanic | 7.11 | 8.13 | 0.33 | 3.21 | 0.15 | 6.67 |
| Non-Hispanic | 80.36 | 91.87 | 9.95 | 96.79 | 2.10 | 93.33 |
| Age | ||||||
| Age 65-74 | 50.70 | 57.96 | 6.15 | 59.77 | 1.33 | 59.11 |
| Age 75-84 | 25.25 | 28.87 | 2.96 | 28.77 | 0.65 | 28.89 |
| Age 85+ | 11.52 | 13.17 | 1.18 | 11.47 | 0.27 | 12.00 |
| Income | ||||||
| Top 10% Income (>$69,648) | 12.09 | 0.19 | 0.17 | |||
| Bottom 10% Income (<$19,835) | 5.63 | 0.54 | 0.11 | |||
Notes:
absolute distribution represents the proportion by each category across all drive times.
Relative distribution refers to the proportion within each drive time category
The majority of the Medicare population both within and outside a 30-minute drive time is white, non-Hispanic, and between the ages of 65 and 74. At the same time, the population living at greater than 30 minutes has a higher proportion of individuals who identify as Non-Hispanic, and American Indian or White. This is not unexpected given what is known about the demographic makeup of rural communities.19 A higher proportion of the population with an income in the top 10% lives within 30 minutes of a urologist (12.09%) relative to the population in the bottom 10% (5.63%) suggesting higher income areas have better access to timely urologic care.
Urologist Density
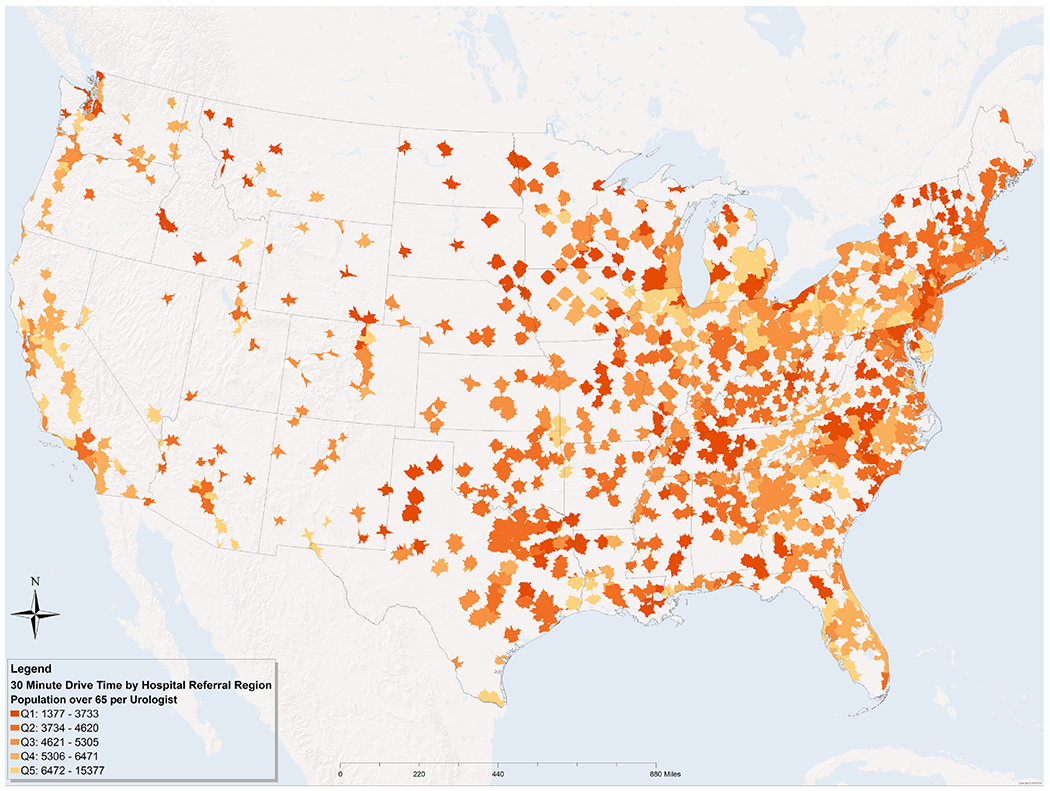
While 87.5% of the US population lives within a 30-minute drive to a urologist, this does not quantify an individual’s access to more than one urologist. Figure 2 shows the population density per urologist (stratified by quintiles) for those over 65 living within 30 (Figure 2a) and 60 (Figure 2b) minutes. Areas with the highest density had a median of one urologist per 3,272 individuals over age 65 within 30-minute drive time, versus low density areas where there is one urologist per 7,757 individuals.
Figure 2.
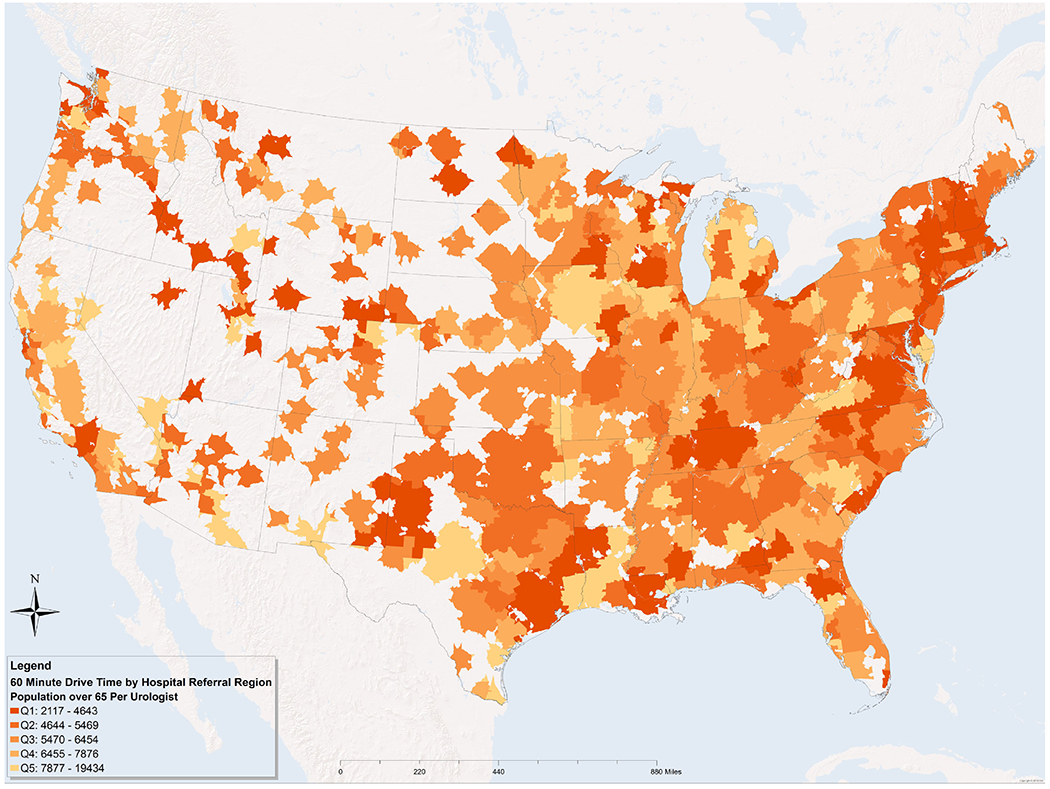
Density of urologists within A) 30 minutes and B) 60 minutes of drive time, stratified by Hospital Referral Region.
Low density HRRs have a greater proportion of Black and Asian populations with lesser representation by White, Pacific Islander and Hispanic populations compared to high density areas (Table 2.) Low density areas are also characterized by both a higher proportion of individuals having incomes in the top 10% as well as those with incomes in the lowest 10% suggesting income inequality may be greater in these areas.
Table 2.
Between group demographic comparisons of the most versus least dense at 30 minute drive times
| Overall | Q1 Density | Q5 Density | |||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P-Valuea | |
| Total | 40,729,348 | 100 | 5,175,270 | 12.71% | 5,781,449 | 14.19 | |
| Median Concentrationb | 4,721 | 3,272 | 7,757 | ||||
| Race | |||||||
| White | 33,749,404 | 82.86% | 4,582,584 | 88.55% | 4,725,186 | 81.73% | ref |
| Black | 3,824,288 | 9.39% | 260,935 | 5.04% | 660,302 | 11.42% | <0.0001 |
| American Indian | 165,267 | 0.41% | 21,494 | 0.42% | 24,209 | 0.42% | <0.0001 |
| Asian | 1,677,107 | 4.12% | 138,393 | 2.67% | 222,433 | 3.85% | <0.0001 |
| Pacific Islander | 26,858 | 0.07% | 4,510 | 0.09% | 2,394 | 0.04% | <0.0001 |
| Other | 810,505 | 1.99% | 110,443 | 2.13% | 84,814 | 1.47% | 0.24 |
| Multiple Races | 475,919 | 1.17% | 56,911 | 1.10% | 62,111 | 1.07% | <0.0001 |
| Ethnicity | |||||||
| Hispanic | 3,311,818 | 8.13% | 505,052 | 9.76% | 305,458 | 5.28% | <0.0001 |
| Non-Hispanic | 37,417,530 | 91.87% | 4,670,218 | 90.24% | 5,475,991 | 94.72% | ref |
| Age | |||||||
| 65-74 | 23,609,552 | 57.97% | 2,979,888 | 57.58% | 3,344,454 | 57.85% | ref |
| 75-84 | 11,755,678 | 28.86% | 1,525,535 | 29.48% | 1,659,543 | 28.70% | <0.0001 |
| 85+ | 5,364,118 | 13.17% | 669,847 | 12.94% | 777,452 | 13.45% | <0.0001 |
| Income | |||||||
| Top 10% (>$69,648) | 4,832,818 | 11.87% | 408,044 | 7.88% | 711,136 | 12.30% | ref |
| Bottom 10% (<$19,835) | 2,696,585 | 6.62% | 302,468 | 5.84% | 436,340 | 7.55% | <0.0001 |
Note:
P-value compares distributions at the Q1 versus Q5 density.
Medicare population per urologist.
Discussion
In this study, we utilized a novel approach to evaluate disparities in access to urologic care by measuring the drive time to urologists combined with provider density. We found that nearly all of the US population lives within one-hour drive time of a urologist and 87.5% of the population 65 and older has access to a urologist within 30-minute drive time.
However, we did identify important disparities in timely access to urologic care. On the one hand, White and American Indian populations, which make up a greater proportion of rural communities, are represented in greater proportions among those living further than 30 minutes from a urologist. On the other hand, Black and Asian populations are more likely to live in areas with timely access to few urology providers. Taken together, this suggests that there are various forms of disparities in timely access to care; people in rural communities live a greater distance from providers, whereas urban areas have a distribution of providers that limits access to some minority communities and those living with greater income inequality. While not well-explored in the urologic literature, income inequality is known to result in worse health outcomes.20
Our study has important limitations related to the use of administrative and population data. Presence of a urologist nearby does not necessarily ensure adequate access. This study depicts available urology practice locations based on claims data and does not describe where individual patients actually travel to receive urologic care. Many other factors also limit access to care. For instance, insurance status and a provider’s acceptance of insurance policies impact access. Additionally, we estimated population locations using census blocks. This may over- or under-estimate travel times for some within census blocks. However, this is likely to represent small differences and unlikely to influence this analysis. Finally, our analysis only includes urologists that have billed Medicare, which likely does not accurately reflect the estimated 4.1% of urologists that only work at a Veterans Affairs hospital or the estimated 8.5% of pediatric fellowship trained urologists.21
We also limited population descriptions and density calculations to those 65 or older. While this was chosen to reflect the source of data for urologists and because the average age of urology patients tends to be older, there may be some areas where our calculations of access are over or under representations. Finally,
While we have uncovered some notable disparities in timely access to urologic care, further work will need to examine whether these differences are related to patient outcomes. Other work has shown that longer distance to a urologist has been associated with a higher rate of high risk prostate cancer at diagnosis, with an increased impact of this relationship among black patients.3 Additionally, for patients receiving definitive radiation, increased travel distance is associated with an increased rate of receiving stereotactic body radiotherapy. This modality requires a shorter treatment course compared to traditional external beam radiotherapy, but has less long term outcomes data.22 Additional evidence supports greater distance to care resulting in later stage at presentation for kidney cancer23, and inconsistent evidence suggests greater mortality after cystectomy.24, 25
Additional research will also need to explore whether driving time is the best measure to assess timely access for all populations. For example, some urban/metropolitan centers may have short drive times but long public transportation times. It may be that certain populations face substantial access issues due to lack of urologists near available public transportation.26
Whether the travel time to high versus low density of urologists is related to health outcomes also remains to be investigated. It may be that there is a sweet spot of access where patients are able to obtain timely care from the optimal number of urologic providers. That is, patients served by few providers may experience worse outcomes due to the distance decay effect. At the same time, growing evidence suggests that areas served by high provider density may experience inferior outcomes. For example, recent work demonstrates patients in markets with high concentrations of providers experience greater use of low-value bladder cancer care27, 28, worse cardiac outcomes17, and higher prices for joint replacement and other common surgical procedures.15, 29 Taken together, it may be that patients living in areas with timely access to either few urologists or too many urologists experience sub-optimal outcomes.
While our results identify significant variation in access to urologic care, these results appear more optimistic than previous studies of urologist geographic location. For example, the AUA census identified that 63.5% of counties lack a urologist and only 10% of urologists practice in non-metropolitan counties.21 Based on our analysis it appears that urologists are aggregating in similar locations to the Medicare population and that the absence of a urologist in a given county does not preclude the presence of a urologist within close driving distance.
Conclusions
Drive time to urologists combined with urologist density is a novel approach to investigating urologic care access and could be a useful tool for future health disparities research. While almost all of the US population lives within one-hour drive time to a urologist, there remain important differences in the population which is severed by high compared to low provider density.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yao N, Foltz SM, Odisho AY et al. : Geographic Analysis of Urologist Density and Prostate Cancer Mortality in the United States. PLoS ONE, 10: e0131578, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Selph JP, Peterson AC: Review Article: Past, Present and Future of Cancer Survivorship and the Importance of the Urologist. Urology Practice, 4: 60, 2017 [DOI] [PubMed] [Google Scholar]
- 3.Holmes JA, Carpenter WR, Wu Y et al. : Impact of distance to a urologist on early diagnosis of prostate cancer among black and white patients. J Urol, 187: 883, 2012 [DOI] [PubMed] [Google Scholar]
- 4.Kelly C, Hulme C, Farragher T et al. : Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open, 6: e013059, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arcury TA, Preisser JS, Gesler WM et al. : Access to transportation and health care utilization in a rural region. J Rural Health, 21: 31, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Lara MD, Baker MT, Larson CJ et al. : Travel distance, age, and sex as factors in follow-up visit compliance in the post-gastric bypass population. Surg Obes Relat Dis, 1: 17, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Crawford SM, Sauerzapf V, Haynes R et al. : Social and geographical factors affecting access to treatment of lung cancer. Br J Cancer, 101: 897, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pruthi RS, Neuwahl S, Nielsen ME et al. : Recent Trends in the Urology Workforce in the United States. Urology, 82: 987, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Odisho AY, Cooperberg MR, Fradet V et al. : Urologist Density and County-Level Urologic Cancer Mortality. Journal of Clinical Oncology, 28: 2499, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cary C, Odisho AY, Cooperberg MR: Variation in prostate cancer treatment associated with population density of the county of residence. Prostate Cancer And Prostatic Diseases, 19: 174, 2016 [DOI] [PubMed] [Google Scholar]
- 11.Ruetters D, Keinki C, Schroth S et al. : Is there evidence for a better health care for cancer patients after a second opinion? A systematic review. J Cancer Res Clin Oncol, 142: 1521,2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mellink WA, Henzen-Logmans SC, Bongaerts AH et al. : Discrepancy between second and first opinion in surgical oncological patients. Eur J Surg Oncol, 32: 108, 2006 [DOI] [PubMed] [Google Scholar]
- 13.Brimo F, Schultz L, Epstein JI: The value of mandatory second opinion pathology review of prostate needle biopsy interpretation before radical prostatectomy. J Urol, 184: 126, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Wibmer A, Vargas HA, Donahue TF et al. : Diagnosis of Extracapsular Extension of Prostate Cancer on Prostate MRI: Impact of Second-Opinion Readings by Subspecialized Genitourinary Oncologic Radiologists. AJR Am J Roentgenol, 205: W73, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Austin DR, Baker LC: Less Physician Practice Competition Is Associated With Higher Prices Paid For Common Procedures. Health Aff (Millwood), 34: 1753, 2015 [DOI] [PubMed] [Google Scholar]
- 16.Baker LC, Bundorf MK, Royalty AB et al. : Physician practice competition and prices paid by private insurers for office visits In: JAMA. United States, vol. 312, pp. 1653–62, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Koch T, Wendling B, Wilson NE: Physician Market Structure, Patient Outcomes, and Spending: An Examination of Medicare Beneficiaries. Health ServRes, 53: 3549, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haddad AQ, Hutchinson R, Wood EL et al. : Association of Distance to Treatment Facility With Survival and Quality Outcomes After Radical Cystectomy: A Multi-Institutional Study. Clin Genitourin Cancer, 15: 689, 2017 [DOI] [PubMed] [Google Scholar]
- 19.Agriculture U. S. D. o.: Rural America At A Glance 2018 Edition, 2018
- 20.Kondo N, Sembajwe G, Kawachi I et al. : Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. Bmj, 339: b4471, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Urologic Association: The State of the Urology Workforce and Practice in the United States, 2016
- 22.A. MB, Yu-Wei C, V. SR et al. : Travel distance and stereotactic body radiotherapy for localized prostate cancer. Cancer, 124: 1141, 2018 [DOI] [PubMed] [Google Scholar]
- 23.Prassannah S, Sarah ON, Gausihi S et al. : The dilemma of distance: patients with kidney cancer from regional Australia present at a more advanced stage. BJU International, 113: 57, 2014 [DOI] [PubMed] [Google Scholar]
- 24.Ryan S, Serrell EC, Karabon P et al. : The Association between Mortality and Distance to Treatment Facility in Patients with Muscle Invasive Bladder Cancer. J Urol, 199: 424, 2018 [DOI] [PubMed] [Google Scholar]
- 25.Smith AB, Meyer A-M, Meng K et al. : The relationship of travel distance with cystectomy access and outcomes. Urologic Oncology: Seminars and Original Investigations, 36: 308.e1, 2018 [DOI] [PubMed] [Google Scholar]
- 26.Overholser S, Thompson I III, Sosland R et al. : Medicaid Patient Access to Urological Care in the Era of the Patient Protection and Affordable Care Act: A Baseline to Measure Policy Effectiveness. Urology Practice, 3: 276, 2016 [DOI] [PubMed] [Google Scholar]
- 27.O’Neil B, Graves AJ, Barocas DA et al. : Doing More for More: Unintended Consequences of Financial Incentives for Oncology Specialty Care. J Natl Cancer Inst, 108, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Neil B, Tyson M, Graves A et al. : The Influence of Provider Characteristics and Market Forces on Response to Financial Incentives. American Journal of Managed Care, 24, 2018. [PubMed] [Google Scholar]
- 29.Sun E, Baker LC: Concentration In Orthopedic Markets Was Associated With A 7 Percent Increase In Physician Fees For Total Knee Replacements. Health Aff (Millwood), 34: 916, 2015 [DOI] [PubMed] [Google Scholar]


