We report eight children with COVID-19 presenting at a single centre in the UK with symptoms of atypical appendicitis before rapid deterioration requiring hospitalisation and, in some cases, intensive care support. All children had imaging confirming terminal ileitis and no surgical intervention was required at the time of writing. We draw attention to an unusual presentation of COVID-19 in children and adolescents and we recommend abdominal imaging when investigating for possible appendicitis.
There have been 4 730 968 confirmed cases and 315 488 deaths from COVID-19 worldwide since emergence of the infection in December, 2019, in Wuhan, China.1 To date, most of the case load and mortality has been seen in the adult population. Currently in the UK, there is concern regarding an inflammatory syndrome related to COVID-19 in children with gastrointestinal symptoms in the presence of both positive and negative severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) PCR tests.2, 3
Children have been observed to have milder clinical manifestations of the virus than do adults, sometimes acting as asymptomatic carriers of infection.4 Although gastrointestinal symptoms have not been recognised in the early stages of the pandemic, and are infrequently reported in the literature on infection in adults,5 it has been reported that a high mean viral load in the nasopharynx is associated with the occurrence of diarrhoea in patients with severe acute respiratory syndrome.6 We draw attention to COVID-19 presenting in paediatric patients with primary symptoms of fever and abdominal pain, which might be mistaken for appendicitis.
Eight patients in a tertiary paediatric institution were referred for a surgical review over an 8-day period (April 25–May 2, 2020). All patients presented with a combination of symptoms including fever, abdominal pain, diarrhoea, and vomiting. The working diagnosis was of systemic sepsis based on raised blood inflammatory markers thought to be secondary to suspected appendicitis. All patients apart from one presented with markedly elevated C-reactive protein. Further clinical details are provided in the appendix (pp 1–2). Patients received antibiotics and fluids, and were investigated with blood tests, urine and bloods cultures, and, in patient 4, a lumbar puncture. All patients, except for patient 6, initially had an abdominal ultrasound scan. Patients 4, 5, 6, and 7 had abdominal CT scans and patient 6 had an abdominal ultrasound following the CT. Findings on ultrasound were in line with lymphadenopathy and presence of inflammatory fat throughout the mesentery, with thickening of the terminal ileum (appendix pp 1–2). These findings were mirrored on CT (appendix pp 1–2), which represents a better modality to show a non-inflamed appendix than does ultrasonography.
Patient 4 had a severe inflammatory response and myocarditis, and was transferred from another institution to be offered extracorporeal membrane oxygenation. Three patients (3, 5, and 6) developed a systemic inflammatory response and were transferred directly to paediatric intensive care due to haemodynamic instability. Patients 3 and 6 were initially planned for laparoscopy and appendicectomy in the local institution. Plans for operative intervention were subsequently abandoned due to haemodynamic instability, requirement for inotropes and intensive care support, and, in the case of patient 3, a positive SARS-CoV-2 PCR.
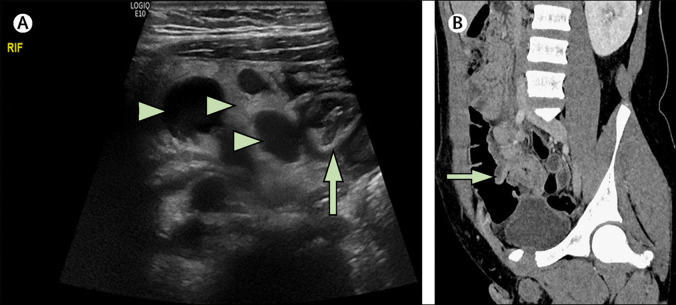
Although SARS-CoV-2 PCR was negative, patients 2 and 7 were suspected to have COVID-19 because of the similarity of their clinical presentation and imaging (appendix pp 1–2). Patient 7 presented with a 5-day history of right iliac fossa pain and fever. The radiological findings common to patients in this series are shown in the figure .
Figure.
Imaging for patient 7
(A) Initial ultrasound shows lymphadenopathy and inflammatory fat throughout the mesentery (arrowheads) and thickening of the terminal ileum (arrow). (B) CT confirms this finding (arrow) and shows a non-inflamed appendix and adjacent mesenteric fat.
Patients 2, 3, 4, and 6 received immunoglobulin and steroid treatment for atypical Kawasaki disease. Patient 2 had peripheral oedema and patient 3 had periorbital oedema, but no specific features of Kawasaki disease. Patients 4 and 6 were treated because of the perceived benefit in managing the severe systemic inflammatory syndrome.
All patients, except for patients 1 and 8 (who have been discharged), are receiving ongoing inpatient care and their outcomes are unknown. No patients have died.
We note that six patients were from a black or Asian ethnic group (appendix pp 1–2). Disparity in outcome of frontline workers and the general population in black and minority ethnic groups has been widely reported across the UK, Europem, and North America, and is now addressed as a priority for public health research.7 Ethnicity represents a complex entity and the ethnic make-up of this cohort, albeit a small patient group, supports the theory of a possible interaction of ethnicity-related factors on SARS-CoV-2 infection likelihood and severity.
Our experience serves to increase the awareness of this clinical presentation, particularly for clinicians and surgeons who assess and manage children with abdominal pain and suspected appendicitis. Although clinical examination should guide decision making, and ultrasound is often the only diagnostic imaging modality to exclude appendicitis in the UK, cross-sectional imaging was necessary for differential diagnosis in half (four) of our patients. Given the convincing nature of clinical findings for appendicitis in children with COVID-19, we stress the importance of abdominal imaging and a swab for SARS-CoV-2 PCR in all children before surgical intervention. It is important to stress the need to visualise the appendix through ultrasound, CT, or both. Broad-spectrum antibiotics should be adopted in these patients and transfer to a tertiary paediatric centre should be considered early in the disease course because their condition can rapidly deteriorate. We encourage others to report their experience to better understand how COVID-19 presents in children.
Acknowledgments
We declare no competing interests.
Supplementary Material
References
- 1.Johns Hopkins University and Medicine COVID-19 dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. https://coronavirus.jhu.edu/map.html
- 2.Campbell D, Sample I. At least 12 UK children have needed intensive care due to illness linked to Covid-19. April 27, 2020. https://www.theguardian.com/world/2020/apr/27/nhs-warns-of-rise-in-children-with-new-illness-that-may-be-linked-to-coronavirus?CMP=Share_iOSApp_Other
- 3.Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020 doi: 10.1016/S0140-6736(20)31094-1. published online May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen K, Yang Y, Wang T. Diagnosis, treatment and prevention of 2019 novel coronavirus infection in children: experts' consensus statement. World J Pediatr. 2020 doi: 10.1007/s12519-020-00343-7. published online Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li L, Wu W, Chen S. Digestive system involvement of novel coronavirus infection: prevention and control infection from a gastroenterology perspective. J Dig Dis. 2020;21:199–204. doi: 10.1111/1751-2980.12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng VCC, Hung IFN, Tang BSF. Viral replication in the nasopharynx is associated with diarrhoea in patients with severe acute respiratory syndrome. Clin Infect Dis. 2004;38:467–475. doi: 10.1086/382681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pareek M, Bangash MN, Pareek N. Ethniticy and COVID-19: an urgent public health research priority. Lancet. 2020;395:1421–1422. doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.