SUMMARY
BACKGROUND:
A lack of capacity to diagnose tuberculosis (TB) in children at peripheral health facilities and limited contact screening and management contribute to low case finding in TB-endemic settings.
OBJECTIVE:
To evaluate the implementation of a pilot project that strengthened diagnosis, treatment and prevention of child TB at peripheral health facilities in Uganda.
METHODS:
In June 2015, health care workers at peripheral health facilities were trained to diagnose and treat child TB. Community health care workers were trained to screen household TB contacts. Before- and-after analysis as well as comparisons with non-intervention districts were used to evaluate impact on caseload and treatment outcomes.
RESULTS:
By December 2016, the average number of children (age < 15 years) diagnosed with TB increased from 45 to 108 per quarter. The proportion of child TB among all TB cases increased from 8.8% to 15%, and the proportion completing treatment increased from 65% to 82%. Of 2270 child TB contacts screened, 55 (2.4%) were diagnosed with TB. Of 910 eligible child contacts, 670 (74%) started preventive therapy, 569 (85%) of whom completed therapy.
CONCLUSION:
The strengthening of child TB services at peripheral health facilities in Uganda was associated with increased case finding, improved treatment outcomes and the successful implementation of contact screening and management.
Keywords: tuberculosis, preventive therapy, child, contact screening, Uganda, implementation research
RESUME
CONTEXTE :
Le manque de capacités de diagnostic de la tuberculose (TB) chez les enfants dans les structures de santé périphériques et un dépistage et une prise en charge limités des contacts contribuent à une faible détection des cas dans les contextes d’endémie de TB.
OBJECTIF :
Evaluer la mise en œuvre d’un projet pilote qui a renforcé le diagnostic, le traitement et la prévention de la TB de l’enfant dans les structures de santé périphériques en Ouganda.
MÉTHODE :
En juin 2015, les travailleurs de santé; des structures de santé périphériques ont été formés à diagnostiquer et à traiter la TB de l’enfant. Les travailleurs de santé communautaire ont été formés à réaliser le dépistage des contacts domiciliaires de TB. L’analyse avant et après la formation ainsi que la comparaison avec les districts sans intervention a évalué l’impact sur le volume des patients et les résultats du traitement.
RÉSULTATS:
En décembre 2016, le nombre moyen d’enfants (âge < 15 ans) ayant eu un diagnostic de TB par trimestre avait augmenté de 45 à 108. La proportion de TB de l’enfant parmi tous les cas de TB avait augmenté de 8,8% à 15% et la proportion ayant achevé le traitement avait augmenté de 65% à 82%. Parmi les 2270 enfants contacts de TB dépistés, 55 (2,4%) ont eu un diagnostic de TB. Sur 910 enfants contacts éligibles, 670 (74%) ont débuté un traitement préventif et 569 (85%) l’ont terminé.
CONCLUSION :
Le renforcement des services de TB de l’enfant dans les structures de santé périphériques en Ouganda a été associé avec une augmentation de la détection des cas, une amélioration des résultats du traitement et une mise en œuvre réussie du dépistage et de la prise en charge des contacts.
RESUMEN
MARCO DE REFERENCIA:
La carencia de medios para diagnosticar la tuberculosis (TB) de los niños en los establecimientos periféricos de salud y la restringida investigatión y gestión de los contactos contribuyen a un resultado deficiente de la búsqueda de casos en entornos donde la TB es endémica.
OBJETIVO:
Evaluar la ejecución de un proyecto piloto de fortalecimiento del diagnóstico, el tratamiento y la prevención de la TB pediátrica en los establecimientos periféricos de atención de salud en Uganda.
MÉTODOS:
En junio del 2015, los profesionales de salud de los establecimientos periféricos de salud recibieron una capacitación sobre el diagnóstico y el tratamiento de la TB de los niños. Se impartió una formación a los trabajadores de salud comunitarios destinada a la realización de la investigación de los contactos domiciliarios de pacientes con tuberculosis. La repercusión sobre la cantidad de casos detectados y los desenlaces terapéuticos se examinó mediante análisis antes y después de la intervención y la comparación de los resultados con los de otros distritos que no habían participado.
RESULTADOS:
En diciembre del 2016, el número promedio de niños (edad < 15 años) diagnosticados con TB por trimestre aumentó de 45 a 108. La proporción de niños en todos los casos de TB aumentó de 8,8% a 15% y la proporción de casos que completaron el tratamiento aumentó de 65% a 82%. De los 2270 contactos pediátricos de casos de TB investigados, en 55 se diagnosticó TB (2,4%). De los 910 contactos pediátricos que cumplían los requisitos, 670 (74%) iniciaron el tratamiento preventivo y 569 (85%) lo completaron.
CONCLUSIÓN:
Con el fortalecimiento de los servicios de atención de la TB pediátrica en los establecimientos periféiricos de salud de Uganda se lograron progresos en la búsqueda de casos, mejores desenlaces terapéuticos y una ejecución eficaz de la investigación y la gestión de contactos.
THE WORLD HEALTH ORGANIZATION (WHO) estimated that in 2016 there were one million cases of tuberculosis (TB) in children (age < 15 years), representing 10% of the global caseload, and 253 000 deaths in children due to TB.1 The certainty of the estimates is challenged by underdiagnosis due to clinical overlap with other common childhood diseases and underreporting to the national tuberculosis programmes (NTPs) in TB-endemic countries.1–3 Nonetheless, it is increasingly recognised that TB is an important treatable and preventable cause of child morbidity and mortality.4 The WHO’s End TB Strategy includes a greater focus on prevention and more explicit reference to the needs of children than previous global TB control strategies.5–7 The Stop TB Partnership’s Global Plan to End TB includes a very ambitious target that by 2020, 90% or more of children who have been exposed to TB receive treatment for infection.8 To progress toward such a target, there is need for evidence from TB-endemic, resource-limited settings that demonstrates effective implementation.
Uganda is a high TB-HIV burden country that reported 3316 child TB cases in 2014, representing 8% of the total burden.9,10 This proportion is likely to be an underestimate, as children aged <15 years represent nearly half of the total population in Uganda, and risk factors for TB such as human immunodeficiency virus (HIV) infection and malnutrition are endemic.2 Furthermore, the screening and management of child household contacts of TB cases, with potential to improve case finding and prevention11 and recommended by global and national policy,5,8 is not routinely implemented in Uganda.12
To address these challenges for TB case detection in children, a pilot project entitled ‘Decentralise Tuber-culosis services and Engage Communities to Transform lives of Children with Tuberculosis’ or ‘DETECT Child TB’ was started in two districts in Uganda in 2015. The overall goal was to strengthen district- and community-level health care delivery to improve childhood TB case finding, treatment and prevention.
METHODS
The DETECT Child TB Project was established in collaboration with Uganda’s National TB and Leprosy Programme (NTLP). Two contrasting districts were selected: Kabarole, a rural district in western Uganda (population 469 236) and Wakiso, an urban/peri-urban district in central Uga nda (population 1997 418).13 Similar to other districts in Uganda, provision of health services is decentralised, with health facilities arranged in the hierarchy shown in Table 1. The project covered all Level III and IV health facilities and hospitals in each district (24 in Kabarole and 33 in Wakiso).
Table 1.
Services provided by health facility levels of the National Health Service and numbers in each district
| Kabarole District | Wakiso District | |
|---|---|---|
| n | n | |
| Level I: Village health teams | 70 | 108 |
| Health promotion | ||
| Encourage community participation | ||
| Integrated community case management* | ||
| Level II: Health centre II | 7 | 16 |
| Community outreach services | ||
| Linkages with village health teams | ||
| Preventive care services | ||
| Out-patient care | ||
| Treatment support for tuberculosis | ||
| Level III: Health centre III | 23 | 29 |
| Laboratory services including AFB smear | ||
| Maternity services | ||
| TB treatment and prevention services | ||
| Basic emergency obstetric and new-born care† | ||
| Level IV: Health centre IV | 3 | 8 |
| In-patient services | ||
| Laboratory services, including Xpert® MTB/RIF | ||
| Imaging services, including chest radiography | ||
| Comprehensive emergency obstetric and newborn care‡ | ||
| TB treatment and prevention services | ||
| Blood transfusion services | ||
| Surgical services | ||
| Level V: District/regional referral hospitals | 4 | 9 |
| All services at Level III and IV, plus specialist clinical care services |
A community-based strategy that utilises community health care workers to deliver timely and effective treatment of malaria, pneumonia and diarrhoea to populations with limited access to facility-based health care providers.14
Includes capacity to administer antibiotics, uterotonic drugs (oxytocin) and anticonvulsants (magnesium sulphate); capacity to conduct manual removal of the placenta; removal of retained products following miscarriage or abortion; assisted vaginal delivery (with vacuum extractor); and basic neonatal resuscitation care.15
Includes all the above plus performing Caesarean sections, safe blood transfusion and care for sick and low-birth-weight newborns.15
AFB = acid-fast bacilli; TB = tuberculosis.
A baseline survey was undertaken in April 2015 that provided a situational analysis of child TB services in the two districts for the 2 years preceding project implementation (2013–2014). The findings provided data for the pre-implementation period and informed the development of training materials and job aides for health care workers (HCWs). The training materials focused on the diagnosis of TB in children, including clinical diagnosis—but excluding chest radiology due to unavailability at Levels I–IV of care in Uganda—and implementation of contact screening and management. All materials were consistent with WHO guidelines and were informed by training materials developed by the International Union Against Tuberculosis and Lung Disease (The Union).16–18
In June 2015, 15 district-level HCWs from each district attended a Trainer of Trainers workshop. These Level V HCWs then trained other HCWs at the more peripheral facility levels (III and IV) in child TB diagnosis, treatment and prevention. Pre- and post-training testing evaluated changes in knowledge on child TB diagnosis and management. The district-level HCWs provided on-site mentorship and supportive supervision, monthly during the first 3 months and then quarterly. On-site mentorship reinforced knowledge and skills gained from the training, as well as adherence to national guidelines, which emphasise a systematic approach that includes careful clinical evaluation for TB-related symptoms and signs, history of TB contact, and where possible, investigations for bacteriological confirmation (Figure 1). Supportive supervision addressed health system challenges. An off-line version of The Union’s e-learning child TB course was offered to HCWs at level IV health facilities and hospitals to increase the number of staff with competence in child TB diagnosis and management.18 HCWs from these facilities also received training in sputum collection techniques, i.e., sputum induction and gastric lavage.
Figure 1.
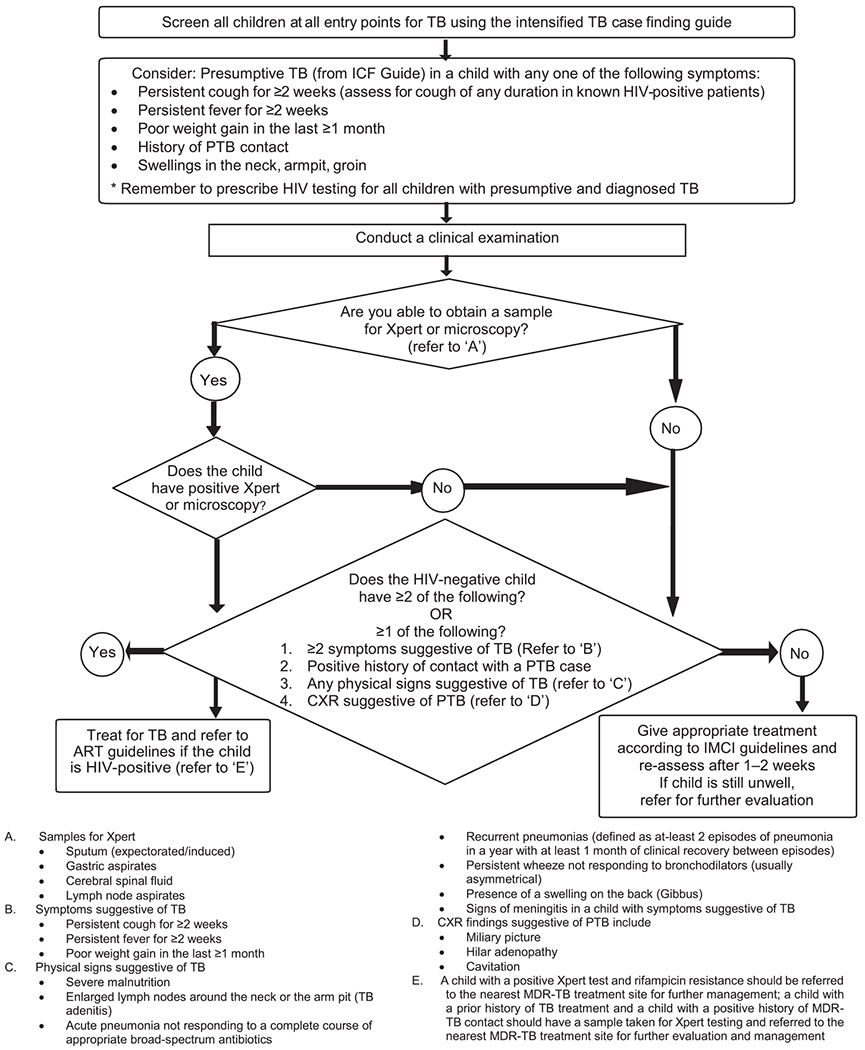
The Uganda national algorithm for the diagnosis of TB in children aged <15 years. TB = tuberculosis; ICF = International Classification of Functioning, Disability and Health; PTB = pulmonary TB; HIV = human immunodeficiency virus; CXR = chest radiography; ART = antiretroviral therapy; IMCI = Integrated Management of Childhood Illness; MDR-TB = multidrug-resistant TB.
Separate training materials and job aides such as flip charts and contact screening forms were developed for the village health teams (VHTs), the Ugandan term for a community health worker. VHTs were given 2 days of training consisting of didactic sessions and role plays on how to carry out symptom-based screening and management of household contacts of index TB cases according to the national isoniazid preventive therapy (IPT) screening algorithm (Appendix Figure A) and WHO guidelines.*7 Symptom-based screening for IPT was recently validated against a radiologically based standard in Uganda, and found to have a negative predictive value of 97.6%.19 VHTs identified, screened and referred symptomatic contacts for further evaluation for TB disease and asymptomatic contacts aged <5 years for IPT. The VHTs also monitored adherence to treatment for index cases, child TB cases and persons on IPT. The VHTs were supported with a small performance-based allowance that was based on the number of homes visited each month.
The project also provided general strengthening support to health systems to improve clinic and laboratory functionality. This included repair of malfunctioning microscopes, technical support for bi-monthly quantification and ordering of laboratory reagents and anti-tuberculosis medicines and provision of buffer laboratory and clinic supplies such as sputum containers and single-drug preparations of isoniazid.
Data management and analysis
Data on TB cases diagnosed, treatment outcomes and HIV testing, disaggregated by sex, age group and TB type, were collected through the routine NTLP reporting system. The project collected additional data in a contact register on the parameters for contact screening and management. Data were manually extracted from the NTLP reporting tools by the district officers and entered into data entry forms using Microsoft Excel (MicroSoft, Redmond, WA, USA). Submitted data were validated by project officers.
Stata v 13 was used for data analysis (StataCorp, College Station, TX, USA). The impact of the intervention was measured by comparing data on case finding and treatment outcomes collected retrospectively for 18 months before implementation (January 2014–June 2015) to data collected prospectively for 18 months during implementation (July 2015–December 2016). The χ2 test was used to analyse categorical variables. Child TB case notifications from July 2015 to December 2016 were compared between the intervention districts and two non-intervention districts (Mukono and Hoima) located in the same geographic region and with similar sociodemographic characteristics. The implementation of household contact tracing during project implementation was analysed and presented using numbers and proportions.
Ethical approval
The project was approved by the Joint Clinical Research Centre’s Institutional Review Board, the Uganda National Council of Science and Technology, Kampala, Uganda, and the Union Ethics Advisory Group, Paris, France.
RESULTS
The project led to an increase in the number of health facilities offering services for the diagnosis and treatment of TB for all ages from 24 to 30 in Kabarole District. In Wakiso District, the number of functional TB units was increased by 5, from 41 to 46, by repairing non-functional microscopes and training laboratory personnel. Pre- and post-training results among trained HCWs from both districts indicated a marked increase in knowledge of the diagnosis and management of child TB: the average mark of 98 HCWs in Wakiso increased from 40% (range 28–70) to 75% (64–89), and from 45% (32–64) to 78% (68–96) among 95 HCWs in Kabarole District (Appendix Table A.1).
Tuberculosis case finding and treatment outcomes
The numbers of all TB cases and the numbers and proportions of child TB cases by age group and type diagnosed according to national guidelines (Figure 1) before and after project implementation are listed in Appendix Table A.2 for each district by quarterly reporting period. Treatment outcomes in child TB cases for each district are listed by quarter in Appendix Table A.3 for the cohort that commenced treatment in the 12-month period before implementation (July 2014–June 2015), and for those who commenced treatment in the first 12 months of the project (July 2015–June 2016).
A comparison of TB case finding in both districts between the pre-implementation and the implementation periods is shown in Table 2. There was a 41% increase in overall TB case notifications, from 3076 before implementation to 4340 during project implementation, which included a 2.4-fold (or 140%) increase in TB case notifications in children (age ⩾ 15 years) and a 1.3-fold (or 32%) increase in cases aged 715 years. The majority of child TB cases were clinically diagnosed. The proportion of children diagnosed with TB who were co-infected with HIV and were started on antiretroviral therapy (ART) did not vary significantly between the two periods. The proportion of child TB cases diagnosed at health facility levels III and IV increased markedly with project implementation (Figure 2).
Table 2.
TB case finding for Kabarole and Wakiso Districts before and during project implementation
| Pre-implementation: January 2014–June 2015 n/N (%) | Implementation: July 2015–December 2016 n/N (%) | P value | |
|---|---|---|---|
| Total TB | 3076 | 4340 | |
| Child TB age < 15 years | 271/3076 (8.8) | 647/4340 (14.9) | <0.01 |
| Child TB (0–4 years) | 99/271 (36.5) | 324/647 (50.1) | <0.01 |
| PTB* | 178/271 (65.7) | 541/647 (83.6) | <0.01 |
| Bacteriologically confirmed TB | 44/178 (24.7) | 71/541 (13.1) | 0.04 |
| Bacteriologically confirmed TB in patients aged < 5 years | 9/44 (20.5) | 16/71 (22.5) | 0.79 |
| Extra-pulmonary TB | 93/271 (34.3) | 106/647 (16.4) | <0.01 |
| TB-HIV co-infected children | 111/271 (40.9) | 234/647 (36.1) | 0.17 |
| TB-HIV children on ART | 94/111 (84.6) | 178/234 (76.1) | 0.06 |
| Average number of child TB per quarter | 45 | 108 |
Intra-thoracic lymph node disease was not included with PTB.
TB = tuberculosis; PTB = pulmonary TB; HIV = human immunodeficiency virus; ART: antiretroviral treatment.
Figure 2.
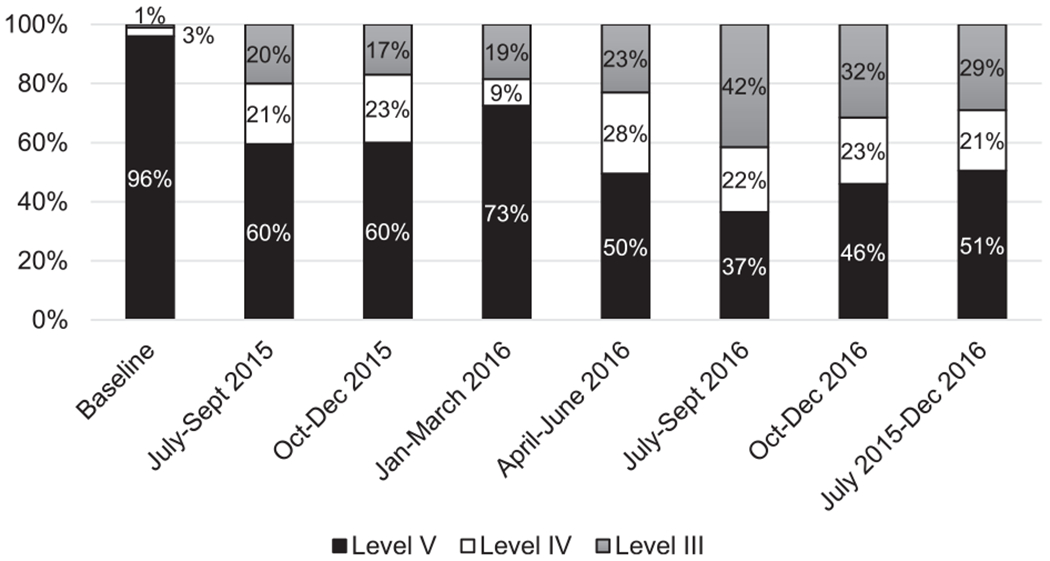
Proportion of child TB cases diagnosed by health facility level in Kabarole and Wakiso Districts. TB = tuberculosis.
The proportion of all TB cases who were children increased from 8.8% to 15% (P < 0.01). The proportion of TB cases in children aged <5 years increased from 36.5% to 50% (P < 0.01); the proportion of child TB that was pulmonary TB increased from 68% to 84% (P < 0.01). The increase in child TB as a proportion of all TB was greater in rural Kabarole District (7% to 16%) than in periurban Wakiso District (10% to 14%) (Appendix Table A.2). Figure 3 shows that the proportions of child TB notifications out of all TB cases recorded was consistently higher in the Kabarole and Wakiso Districts than in the two comparison districts of Hoima and Mukono. Table 3 shows significant improvements in treatment outcomes for children started on anti-tuberculosis treatment within the first 12 months of the project compared to those started on treatment 12 months before the project.
Figure 3.
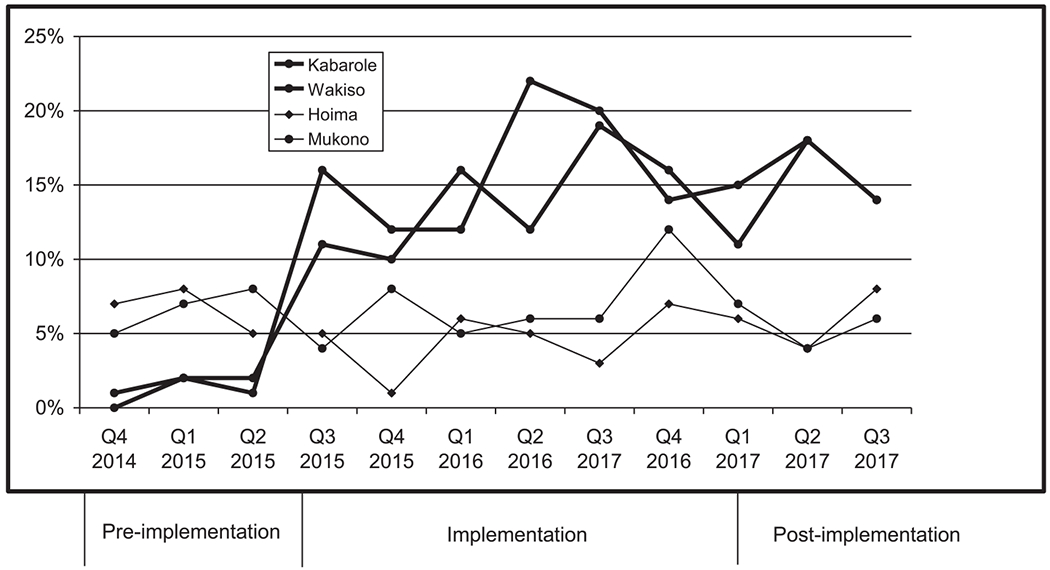
Child TB cases as a proportion of total reported TB caseload over 3 years in implementation districts compared to non-implementation districts. Q = quarter; TB = tuberculosis.
Table 3.
TB treatment outcomes in Kabarole and Wakiso Districts before and during project implementation
| Pre-implementation: July 2014–June 2015 n/N (%) | Implementation: July 2015–June 2016 n/N (%) | P value | |
|---|---|---|---|
| Child TB, age < 15 years | 186 | 382 | |
| Bacteriologically confirmed TB | 12 | 18 | |
| Cured* | 12/12 (100) | 16/18 (88.9) | 0.3 |
| Treatment completed† | 109/186 (58.6) | 294/382 (77.0) | <0.01 |
| Treatment success‡ | 121/186 (65.1) | 310/382 (81.2) | <0.01 |
| Died | 16/186 (8.6) | 15/382 (3.9) | 0.03 |
| Lost to follow-up | 29/186 (15.6) | 43/382 (11.3) | 0.1 |
| Treatment failure | 12/186 (6.5) | 1/382 (0.3) | <0.01 |
| Not evaluated | 8/186 (4.3) | 13/382 (3.4) | 0.6 |
Defined as two negative sputum smear results (one in the final month of anti-tuberculosis treatment) in a child who previously had bacteriologically confirmed TB.20
Defined as completion of 6 months of anti-tuberculosis treatment but without negative sputum smear results on at least one occasion during treatment.20
Defined as the sum of cured and treatment completed.20
TB = tuberculosis.
Community-based household contact screening and management
From July 2015 to December 2016, 1617 patients with bacteriologically confirmed TB received a home visit from the VHT, and 2270 child contacts were screened (Table 4). Of these, 602 (27%) were symptomatic at the time of screening and were referred to the health facilities for further evaluation, 486 (81%) of the symptomatic contacts attended the health facilities and 55 (11.3%) were diagnosed with TB and started on treatment. These 55 children represent 8.5% of the total number of children started on anti-tuberculosis treatment during the project period. There were 910 asymptomatic child contacts aged <5 years and therefore eligible for IPT. Of these, 670 (74%) were started on IPT. Patients were started on IPT at the health facility but received drug refills by the VHTs if they were unable to make repeat visits to the health facility. By December 2016, 86% of all those who were started on IPT before June 2016 had completed therapy. Only 3 (0.4%) of the 670 children commenced on IPT were subsequently diagnosed with TB. All three children were asymptomatic on initial screening but were clinically diagnosed with TB 1–2 months after initiating IPT treatment. All the children were started on treatment for presumed drug-susceptible TB on the basis of their index cases, and responded well to therapy.
Table 4.
Household screening and uptake in cascade of care
| July–December 2015 n (%) | January–December 2016 n (%) | July–December 2016 n (%) | Total n (%) | |
|---|---|---|---|---|
| Wakiso District | ||||
| Index cases, n | 534 | 493 | 516 | 1543 |
| Households screened, n | 306 | 354 | 378 | 1038 |
| Children (<15 years) in households, n | 393 | 385 | 519 | 1297 |
| Symptomatic children | 136 (35) | 102 (27) | 140 (27) | 378 (29) |
| Children evaluated for TB | 114 (84) | 87 (85) | 143 (102) | 344 (91) |
| Children diagnosed with TB | 8 (7) | 11 (13) | 13 (9) | 32 (9) |
| Children eligible for IPT, n* | 124 | 165 | 163 | 452 |
| Children who commenced IPT | 27 (22) | 173 (105) | 145 (89) | 345 (76) |
| Children who completed IPT | 27 (100) | 150 (87) | 121 (83) | 298 (86) |
| Children who developed TB on IPT | 0 | 3 (1.7) | 0 | 3 (0.8) |
| Kabarole District | ||||
| Index cases, n | 251 | 282 | 245 | 778 |
| Households screened, n | 176 | 210 | 193 | 579 |
| Children (<15 years) in households, n | 292 | 328 | 353 | 973 |
| Symptomatic children | 95 (33) | 93 (28) | 36 (10) | 224 (23) |
| Children evaluated for TB | 46 (48) | 70 (75) | 26 (72) | 142 (63) |
| Children diagnosed with TB | 3 (7) | 7 (10) | 13 (50) | 23 (16) |
| Children eligible for IPT, n* | 113 | 132 | 213 | 458 |
| Children who commenced IPT | 52 (46) | 94 (71) | 179 (84) | 325 (71) |
| Children who completed IPT | 52 (100) | 69 (73) | 150 (84) | 271 (83) |
| Children who developed TB on IPT | 0 | 0 | 0 | 0 |
| Total | ||||
| Index cases, n | 785 | 775 | 761 | 2321 |
| Households screened, n | 482 | 564 | 571 | 1617 |
| Children (<15 years) in households, n | 685 | 713 | 872 | 2270 |
| Symptomatic children | 231 (34) | 195 (27) | 176 (20) | 602 (27) |
| Children evaluated for TB | 160 (69) | 157 (81) | 169 (96) | 486 (81) |
| Children diagnosed with TB | 11 (7) | 18 (12) | 26 (15) | 55 (11) |
| Children eligible for IPT, n* | 237 | 297 | 376 | 910 |
| Children who commenced IPT | 79 (33) | 267 (90) | 324 (86) | 670 (77) |
| Children who completed IPT | 79 (100) | 219 (82) | 271 (84) | 569 (85) |
| Children who developed TB on IPT | 0 | 3 | 0 | 3 (0.4) |
Only included children aged <5 years.
TB = tuberculosis, IPT = isoniazid preventive therapy.
DISCUSSION
Decentralisation and strengthening of child TB services in Uganda was associated with a significant increase in case notifications and improved treatment outcomes for child TB cases. A major reason for these findings is that a much larger proportion of child TB cases were diagnosed and managed at more peripheral health facilities. Before the project, health workers at these levels did not have the knowledge and skills to diagnose and manage TB in children, which led to either underdiagnosis of cases or referral of presumptive cases to specialist paediatric services at the tertiary care level. This often created additional barriers to access to care. The successful introduction of integrated household contact screening and management by VHTs also contributed to a modest increase in case detection. Scale-up of this model in 10 high TB burden districts is currently ongoing with funding from the 2018–2020 Uganda Global Fund grant.
Evidence of impact is supported by comparisons with two non-intervention districts that did not show a similar increase in child TB case detection over the same time period. Further evidence that the project strengthened the diagnosis of TB in children is that there was an increase in both the proportion of child TB cases detected in younger children (age < 5 years) and in the proportion of child TB that was pulmonary TB. Pulmonary TB is the most common form of TB in children, but is more difficult to clinically diagnose than extra-pulmonary TB,2,17 and is particularly challenging in infants and young children due to clinical and radiological overlap with pneumonia.21
There was also a significant increase in the treatment success rate of children treated for TB, along with a significant decrease in the proportions of death or treatment failure. The increased numbers of trained HCWs available to provide treatment support and community follow-up of children on anti-tuberculosis treatment by the VHTs may be contributing factors. Another may be that the decentralisation of diagnostic services and household screening resulted in earlier diagnosis of TB in children than before the intervention, and so less severe disease. Severity of disease in child TB cases diagnosed in rural Uganda has been associated with mortality.22
Strengthening of community linkages through training of VHTs resulted in the successful implementation of household contact screening, with active case detection in 11% of symptomatic child contacts and high uptake and completion of IPT. The IPT uptake of >85% is higher than previously reported from a number of settings, including urban Uganda.6,23,24 There are likely advantages to having household screening and IPT drug refills delivered by the same community HCW who provides treatment support for the index case. Studies that reported poor uptake and adherence were conducted at clinics that were based at referral-level facilities and were separate from the TB clinics that provided care for the adult index cases.23–27An integrated approach within programmatic services for the index case reported high levels of uptake and delivery, similar to our findings.28–30
There is a need for more evidence on the role of community HCWs as key partners in health care delivery.31 This cadre can provide integrated family-based care and treatment support for both index cases as well as contacts eligible for IPT, overcoming many of the barriers to delivery of preventive therapy.6,26 Finally, most studies reporting outcomes for the implementation of contact screening and preventive therapy do not report on the most important outcome of the number of children diagnosed with TB while receiving preventive therapy. In this project, <1% of young child contacts receiving IPT developed TB, similar to a previous study from Uganda.11 Although adherence to IPT was not measured in this study, this proportion of young child contacts developing TB is much lower than anticipated if IPT was not provided, and similar to recent observational cohort studies using IPT.31,32
This pilot project had limitations. The main one is uncertainty about the accuracy of a clinical diagnosis of TB in children. The increased awareness and knowledge provided by training could potentially lead to overdiagnosis. This diagnostic uncertainty also needs to be considered in the interpretation of treatment outcomes. A before-and-after evaluation makes it difficult to rule out the contribution of other time-varying factors to increased case finding. Although results were compared to two districts without an intervention over the same time period, there may well have been other differences between these settings that may account for the observed results.
In conclusion, the decentralisation of child TB services in Uganda increased TB case finding overall, but particularly in incident cases of child TB and successful implementation of integrated child household contact screening and preventive therapy. Additional implementation projects aimed at decentralisation and integration of child TB services within the routine care system are needed to close the current policy-practice gap and provide important evidence of impact.
Acknowledgements
The authors thank the health care workers, and the children and families in Kabarole and Wakiso districts for their participation.
The DETECT Child TB Project is a collaborative project led by The Union Uganda (Kampala), in partnership with Baylor Uganda (Kampala), Mildmay Uganda (Kampala) and the National TB and Leprosy Program (NTLP) of the Ministry of Health (Kampala, Uganda) of the Government of Uganda. The project received funding from ELMA Foundation, New York, NY, USA, and an anonymous donor through The Union’s North America Office. Salary support for research to SZM was provided by Fogarty International Center, National Institutes for Health, Bethesda, MD, USA (grant #D43TW009771: HIV co-infections in Uganda: TB, Cryptococcus, and Viral Hepatitis).
APPENDIX
Table A.1.
Pre and post training results for individual health care workers trained during the DETECT Child TB Project
| Wakiso District |
Kabarole District |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Pre-test % | Post-test % | No. | Pre-test % | Post-test % | No. | Pre-test % | Post-test % | No. | Pre-test % | Post-test % |
| 1 | 45 | 73 | 50 | 38 | 75 | 1 | 40 | 70 | 49 | 40 | 78 |
| 2 | 36 | 75 | 51 | 41 | 75 | 2 | 41 | 72 | 50 | 45 | 73 |
| 3 | 28 | 74 | 52 | 35 | 76 | 3 | 39 | 90 | 51 | 48 | 72 |
| 4 | 40 | 65 | 53 | 42 | 82 | 4 | 42 | 80 | 52 | 45 | 70 |
| 5 | 32 | 75 | 54 | 43 | 75 | 5 | 47 | 78 | 53 | 43 | 78 |
| 6 | 38 | 76 | 55 | 44 | 75 | 6 | 44 | 77 | 54 | 45 | 78 |
| 7 | 40 | 75 | 56 | 52 | 74 | 7 | 48 | 76 | 55 | 46 | 74 |
| 8 | 41 | 75 | 57 | 40 | 72 | 8 | 47 | 78 | 56 | 44 | 78 |
| 9 | 44 | 76 | 58 | 45 | 70 | 9 | 45 | 79 | 57 | 43 | 71 |
| 10 | 37 | 77 | 59 | 32 | 75 | 10 | 39 | 94 | 58 | 42 | 78 |
| 11 | 33 | 75 | 60 | 36 | 71 | 11 | 40 | 72 | 59 | 43 | 78 |
| 12 | 38 | 70 | 61 | 40 | 78 | 12 | 37 | 84 | 60 | 45 | 78 |
| 13 | 45 | 67 | 62 | 41 | 76 | 13 | 35 | 78 | 61 | 40 | 72 |
| 14 | 45 | 75 | 63 | 39 | 77 | 14 | 51 | 97 | 62 | 44 | 68 |
| 15 | 40 | 73 | 64 | 42 | 75 | 15 | 46 | 78 | 63 | 45 | 71 |
| 16 | 52 | 75 | 65 | 38 | 75 | 16 | 43 | 70 | 64 | 46 | 76 |
| 17 | 35 | 75 | 66 | 39 | 82 | 17 | 42 | 78 | 65 | 47 | 75 |
| 18 | 34 | 74 | 67 | 40 | 79 | 18 | 50 | 96 | 66 | 45 | 78 |
| 19 | 36 | 77 | 68 | 40 | 78 | 19 | 44 | 78 | 67 | 48 | 77 |
| 20 | 39 | 70 | 69 | 39 | 79 | 20 | 42 | 74 | 68 | 45 | 73 |
| 21 | 40 | 72 | 70 | 37 | 75 | 21 | 43 | 81 | 69 | 46 | 74 |
| 22 | 39 | 69 | 71 | 40 | 76 | 22 | 40 | 77 | 70 | 45 | 78 |
| 23 | 42 | 80 | 72 | 32 | 75 | 23 | 40 | 96 | 71 | 44 | 78 |
| 24 | 61 | 73 | 73 | 41 | 72 | 24 | 48 | 79 | 72 | 46 | 75 |
| 25 | 42 | 74 | 74 | 40 | 73 | 25 | 45 | 78 | 73 | 45 | 76 |
| 26 | 45 | 75 | 75 | 40 | 75 | 26 | 46 | 75 | 74 | 42 | 72 |
| 27 | 38 | 73 | 76 | 48 | 89 | 27 | 45 | 69 | 75 | 41 | 79 |
| 28 | 37 | 75 | 77 | 37 | 78 | 28 | 47 | 77 | 76 | 44 | 80 |
| 29 | 35 | 76 | 78 | 38 | 75 | 29 | 49 | 78 | 77 | 45 | 78 |
| 30 | 34 | 80 | 79 | 40 | 77 | 30 | 50 | 78 | 78 | 47 | 76 |
| 31 | 40 | 75 | 80 | 37 | 79 | 31 | 52 | 92 | 79 | 48 | 78 |
| 32 | 41 | 64 | 81 | 36 | 75 | 32 | 45 | 87 | 80 | 49 | 79 |
| 33 | 40 | 77 | 82 | 51 | 87 | 33 | 44 | 74 | 81 | 44 | 80 |
| 34 | 40 | 85 | 83 | 40 | 72 | 34 | 45 | 78 | 82 | 45 | 95 |
| 35 | 42 | 75 | 84 | 39 | 77 | 35 | 46 | 77 | 83 | 37 | 78 |
| 36 | 27 | 72 | 85 | 38 | 75 | 36 | 45 | 78 | 84 | 64 | 75 |
| 37 | 38 | 73 | 86 | 41 | 79 | 37 | 42 | 77 | 85 | 45 | 76 |
| 38 | 34 | 78 | 87 | 47 | 74 | 38 | 43 | 89 | 86 | 42 | 78 |
| 39 | 70 | 79 | 88 | 42 | 75 | 39 | 45 | 79 | 87 | 44 | 81 |
| 40 | 41 | 77 | 89 | 42 | 80 | 40 | 46 | 76 | 88 | 34 | 78 |
| 41 | 40 | 74 | 90 | 47 | 72 | 41 | 32 | 78 | 89 | 45 | 78 |
| 42 | 39 | 75 | 91 | 39 | 81 | 42 | 50 | 74 | 90 | 47 | 75 |
| 43 | 39 | 76 | 92 | 37 | 75 | 43 | 45 | 72 | 91 | 46 | 68 |
| 44 | 32 | 72 | 93 | 36 | 74 | 44 | 44 | 78 | 92 | 48 | 73 |
| 45 | 37 | 75 | 94 | 37 | 70 | 45 | 45 | 72 | 93 | 57 | 78 |
| 46 | 40 | 73 | 95 | 40 | 75 | 46 | 57 | 71 | 94 | 44 | 93 |
| 47 | 37 | 65 | 96 | 42 | 76 | 47 | 46 | 92 | 95 | 52 | 74 |
| 48 | 36 | 70 | 97 | 55 | 75 | 48 | 47 | 78 | |||
| 49 | 35 | 75 | 98 | 37 | 72 | ||||||
Table A.2.
Child TB caseload in Wakiso and Kabarole Districts from January 2014 until end December 2016
| 2015 |
2016 |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 2014 |
January–March | April–June | July–September | October–December | January–March | April–June | July–September | October–December | |
| Indicator | Pre-implementation, n | Project implementation, n | |||||||
| Wakiso District | |||||||||
| All TB cases | 1161 | 344 | 373 | 381 | 399 | 542 | 532 | 519 | 531 |
| Child TB cases | 125 | 34 | 31 | 40 | 38 | 88 | 63 | 98 | 84 |
| Proportion child cases, % | 11 | 10 | 8 | 10 | 10 | 16 | 12 | 19 | 16 |
| 0–4 years | 46 | 8 | 9 | 20 | 16 | 38 | 31 | 52 | 37 |
| Proportion 0–4 years, % | 37 | 24 | 29 | 50 | 42 | 43 | 49 | 53 | 44 |
| 5–14 years | 79 | 26 | 22 | 20 | 22 | 50 | 32 | 46 | 47 |
| PTB | 76 | 19 | 18 | 31 | 28 | 62 | 53 | 80 | 67 |
| Proportion PTB, % | 61 | 56 | 58 | 78 | 74 | 70 | 84 | 82 | 80 |
| EPTB | 49 | 15 | 13 | 9 | 10 | 26 | 10 | 18 | 17 |
| TB-HIV | 56 | 6 | 12 | 25 | 12 | 26 | 21 | 34 | 28 |
| Proportion TB-HIV, % | 44.8 | 17.6 | 38.7 | 62.5 | 31.6 | 29.5 | 33.3 | 34.7 | 33.3 |
| TB-HIV on ART | 47 | 6 | 4 | 17 | 5 | 18 | 10 | 18 | 22 |
| Kabarole District | |||||||||
| All TB cases | 780 | 209 | 209 | 209 | 202 | 199 | 317 | 246 | 263 |
| Child TB cases | 58 | 9 | 14 | 34 | 24 | 23 | 70 | 48 | 37 |
| Proportion child cases, % | 7 | 4 | 7 | 16 | 12 | 12 | 22 | 20 | 14 |
| 0–4 years | 27 | 4 | 5 | 22 | 12 | 13 | 37 | 25 | 21 |
| Proportion 0–4 years, % | 47 | 44 | 36 | 65 | 50 | 57 | 53 | 52 | 57 |
| 5–14 years | 31 | 5 | 9 | 12 | 12 | 10 | 33 | 23 | 16 |
| PTB | 50 | 8 | 13 | 32 | 22 | 19 | 64 | 47 | 35 |
| Proportion PTB, % | 86 | 89 | 93 | 94 | 92 | 83 | 91 | 98 | 95 |
| EPTB | 8 | 1 | 1 | 2 | 2 | 4 | 6 | 1 | 2 |
| TB-HIV | 28 | 3 | 6 | 8 | 12 | 19 | 5 | 28 | 16 |
| Proportion TB-HIV, % | 48.3 | 33.3 | 42.9 | 23.5 | 50.0 | 82.6 | 7.1 | 58.3 | 43.2 |
| TB-HIV on ART | 28 | 3 | 6 | 8 | 12 | 19 | 5 | 28 | 16 |
| Total (Wakiso + Kabarole) | |||||||||
| All TB cases | 1941 | 553 | 582 | 590 | 601 | 741 | 849 | 765 | 794 |
| Child TB cases | 183 | 43 | 45 | 74 | 62 | 111 | 133 | 146 | 121 |
| Proportion child cases, % | 9 | 8 | 8 | 13 | 10 | 15 | 16 | 19 | 15 |
| 0–4 years | 73 | 12 | 14 | 42 | 28 | 51 | 68 | 77 | 58 |
| Proportion 0–4 years, % | 40 | 28 | 31 | 57 | 45 | 46 | 51 | 53 | 48 |
| PTB | 126 | 27 | 31 | 63 | 50 | 81 | 117 | 127 | 102 |
| Proportion PTB, % | 69 | 63 | 69 | 85 | 81 | 73 | 88 | 87 | 84 |
| EPTB | 57 | 16 | 14 | 11 | 12 | 30 | 16 | 19 | 19 |
| TB-HIV | 84 | 9 | 18 | 33 | 24 | 45 | 26 | 62 | 44 |
| Proportion TB-HIV, % | 45.9 | 20.9 | 40.0 | 44.6 | 38.7 | 40.5 | 19.5 | 42.5 | 36.4 |
| TB-HIV on ART | 75 | 9 | 10 | 25 | 17 | 37 | 15 | 46 | 38 |
TB = tuberculosis; PTB = pulmonary TB; EPTB = extra-pulmonary TB; HIV = human immunodeficiency virus.
Table A.3.
Treatment outcomes for children treated for TB by district before and after implementation of DETECT Child TB Project
| Treatment outcome | Pre-implementation period, n | Implementation period, n | 2014–2015 Total n (%) | 2015–2016 Total n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| July–September 2014 | October–December 2014 | January–March 2015 | April–June 2015 | July–September 2015 | October–December 2015 | January–March 2015 | April–June 2015 | |||
| Wakiso District | ||||||||||
| Cured | 3 | 0 | 2 | 1 | 3 | 1 | 6 | 1 | 6 (5) | 11 (5) |
| Treatment completed | 22 | 8 | 18 | 21 | 27 | 27 | 68 | 49 | 69 (57) | 171 (78) |
| Treatment success rate, % | 56 | 67 | 59 | 71 | 75 | 74 | 84 | 79 | 75 (62) | 182 (80) |
| Died | 3 | 0 | 4 | 3 | 5 | 2 | 0 | 1 | 10 (8) | 8 (4) |
| Lost to follow-up | 11 | 1 | 6 | 1 | 4 | 4 | 9 | 0 | 19 (16) | 17 (8) |
| Treatment failure | 3 | 0 | 4 | 4 | 0 | 0 | 0 | 0 | 11 (9) | 0 |
| Not evaluated | 3 | 3 | 0 | 1 | 1 | 4 | 5 | 3 | 7 (8) | 13 (6) |
| Still on treatment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 9* | 0 | 9 (4) |
| Total cases evaluated | 45 | 12 | 34 | 31 | 40 | 38 | 88 | 63 | 122 | 229 |
| Kabarole District | ||||||||||
| Cured | 2 | 0 | 2 | 2 | 1 | 2 | 1 | 1 | 6 (10) | 5 (3) |
| Treatment completed | 8 | 18 | 6 | 8 | 24 | 18 | 17 | 55 | 40 (63) | 114 (76) |
| Treatment success rate, % | 56 | 82 | 89 | 71 | 74 | 83 | 82 | 80 | 46 (73) | 119 (79) |
| Died | 3 | 1 | 0 | 2 | 3 | 2 | 2 | 0 | 6 (10) | 7 (5) |
| Lost to follow-up | 5 | 3 | 0 | 2 | 5 | 2 | 2 | 14 | 10 (16) | 23 (15) |
| Treatment failure | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 (2) | 1 (0.7) |
| Not evaluated | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (2) | 0 |
| Still on treatment | 0 | 0 | 0 | 0 | 0 | 0 | 1 † | 0 | 0 | 1 (0.7) |
| Total cases evaluated | 18 | 22 | 9 | 14 | 34 | 24 | 23 | 70 | 63 | 151 |
| Combined data | ||||||||||
| Cured | 5 | 0 | 3 | 3 | 4 | 3 | 7 | 2 | 12 (7) | 16 (4) |
| Treatment completed | 30 | 26 | 24 | 29 | 51 | 45 | 85 | 104 | 109 (59) | 285 (77) |
| Treatment success rate, % | 56 | 75 | 74 | 71 | 75 | 79 | 83 | 80 | 121 (65) | 301 (79) |
| Died | 6 | 1 | 4 | 5 | 8 | 4 | 2 | 1 | 16 (9) | 15 (4) |
| Lost to follow-up | 16 | 4 | 6 | 3 | 9 | 6 | 11 | 14 | 29 (16) | 40 (11) |
| Treatment failure | 3 | 0 | 5 | 4 | 1 | 0 | 0 | 0 | 12 (7) | 1 (0.3) |
| Not evaluated | 3 | 4 | 0 | 1 | 1 | 4 | 5 | 3 | 8 (4) | 13 (4) |
| Still on treatment | 0 | 0 | 0 | 0 | 0 | 0 | 1† | 9* | 0 | 10 (3) |
| Total cases evaluated | 63 | 34 | 43 | 45 | 74 | 62 | 111 | 133 | 185 | 380 |
Children with bone or spinal TB.
Child with MDR-TB.
TB = tuberculosis; MDR-TB = multidrug-resistant TB.
Figure A.
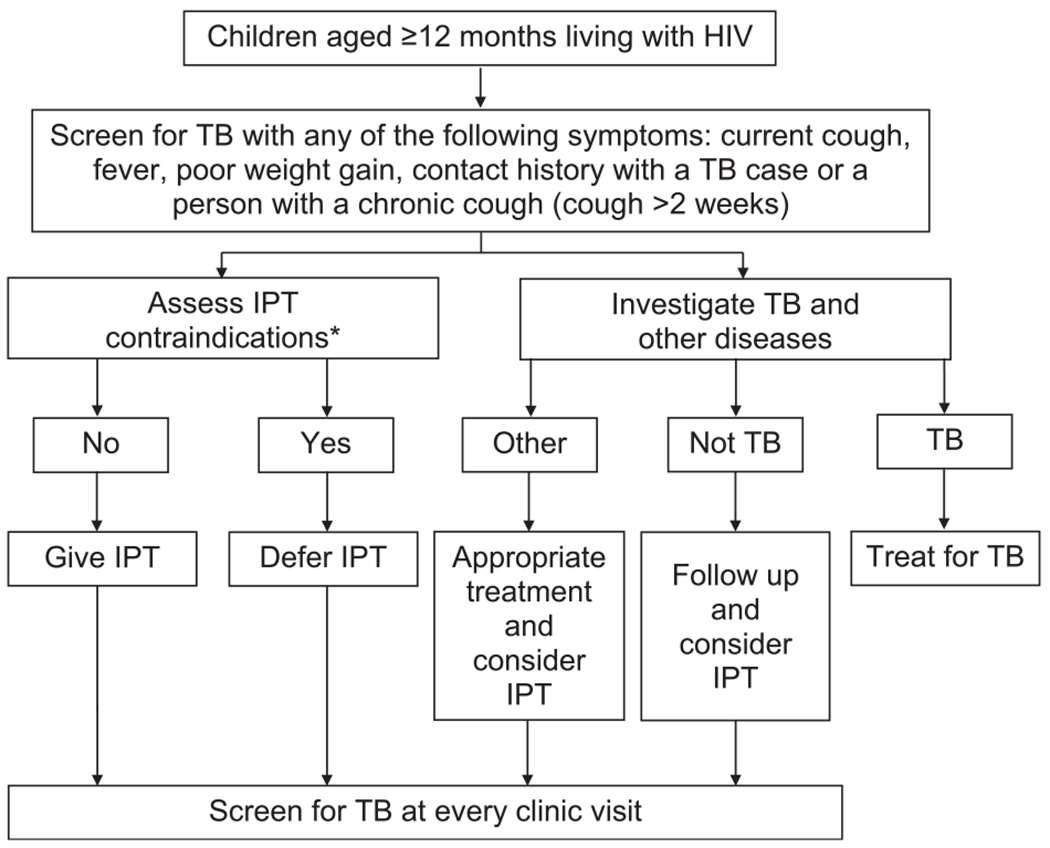
Uganda TB screening and IPT algorithm for children aged ⩾ 12 months. HIV = human immunodeficiency virus; TB = tuberculosis; IPT = isoniazid preventive therapy.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization. Global tuberculosis report, 2017. WHO/HTM/TB/2017.23. Geneva, Switzerland: WHO, 2017. http://www.who.int/tb/publications/global_report/en/ Accessed July 2018. [Google Scholar]
- 2.Donald PR. Childhood tuberculosis: the hidden epidemic. Int J Tuberc Lung Dis 2004; 8: 627–629. [PubMed] [Google Scholar]
- 3.Lestari T, Probandari A, Hurtig AK, Utarini A. High caseload of childhood tuberculosis in hospitals on Java Island, Indonesia: a cross sectional study. BMC Public Health 2011; 11: 784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graham SM, Sismanidis C, Menzies HJ, Marais BJ, Detjen AK, Black RE. Importance of tuberculosis control to address child survival. Lancet 2014; 383: 1605–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. WHO End TB Strategy. Geneva, Switzerland: WHO, 2015. http://www.who.int/tb/strategy/End_TB_Strategy.pdf Accessed July 2018. [Google Scholar]
- 6.Graham SM. The management of infection with Mycobacterium tuberculosis in young children post-2015: an opportunity to close the policy-practice gap. Expert Rev Respir Med 2017; 11: 41–49. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. 2nd ed. WHO/HTM/TB/2014.03 Geneva, Switzerland: WHO, 2014. [PubMed] [Google Scholar]
- 8.Stop TB Partnership. The paradigm shift 2016–2020. Global plan to end TB. Geneva, Switzerland: Stop TB Partnership, 2015. [Google Scholar]
- 9.World Health Organization. Glocal tuberculosis report, 2015 Vol 1 The effects of brief mindfulness intervention on acute pain experience: an examination of individual difference. WHO/HTM/TB/2015.22 Geneva, Switzerland: WHO, 2015. [Google Scholar]
- 10.Uganda Ministry of Health. Uganda national guidelines for tuberculosis infection control in health care facilities, congregate settings and households. Kampala, Uganda: MoH, 2011. [Google Scholar]
- 11.Jaganath D, Zalwango S, Okware B, et al. Contact investigation for active tuberculosis among child contacts in Uganda. Clin Infect Dis 2013; 57: 1685–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uganda Ministry of Health. NTLP annual report. Kampala, Uganda: MoH, 2016. [Google Scholar]
- 13.Uganda Bureau of Statistics. National Population and Housing Census 2014. Kampala, Uganda: UBS, 2014. http://documents.worldbank.org/curated/en/2013/02/17235637/opening-doors-gender-equality-development-middle-east-north-africa Accessed July 2018. [Google Scholar]
- 14.Young M, Wolfheim C, Marsh DR, Hammamy D. WHO/UNICEF joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. Am J Trop Med Hyg 2012; 87: 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maine D, Bailey P, Lobis S. Monitoring emergency obstetric care. J Obstet Gynaecol 2009; 30: 1–153. [Google Scholar]
- 16.International Union Against Tuberculosis and Lung Disease. The Union’s desk guide for diagnosis and management of TB in children. 3rd ed. Paris, France: The Union, 2016. [Google Scholar]
- 17.World Health Organization & International Union Against Tuberculosis and Lung Disease. Childhood TB: training toolkit. Geneva, Switzerland: WHO, 2014. [Google Scholar]
- 18.International Union Against Tuberculosis and Lung Disease. Childhood TB for healthcare workers: an online course. Paris, France: The Union, 2015. https://childhoodtb.theunion.org/courses/CTB1/en/intro [Google Scholar]
- 19.Bonnet M, Kyakwera C, Kyomugasho N, et al. Prospective cohort study of the feasibility and yield of household child tuberculosis contact screening in Uganda. Int J Tuberc Lung Dis 2017; 21: 862–868. [DOI] [PubMed] [Google Scholar]
- 20.Uganda Ministry of Health, Uganda National Tuberculosis and Leprosy Control Programme. Manual for management and control of tuberculosis and leprosy in Uganda. Kampala, Uganda: MoH, 2017. [Google Scholar]
- 21.Oliwa JN, Karumbi JM, Marais BJ, Madhi SA, Graham SM. Tuberculosis as a cause or comorbidity of childhood pneumonia in tuberculosis-endemic areas: a systematic review. Lancet Respir Med 2015; 3: 235–243. [DOI] [PubMed] [Google Scholar]
- 22.Bonnet M, Nansumba M, Bastard M, et al. Outcome of children with presumptive tuberculosis in Mbarara, Rural Uganda. Pediatr Infect Dis J 2018; 37: 147–152. [DOI] [PubMed] [Google Scholar]
- 23.Rutherford ME, Hill PC, Triasih R, Sinfield R, van Crevel R, Graham SM. Preventive therapy in children exposed to Mycobacterium tuberculosis: problems and solutions. Trop Med Int Health 2012; 17: 1264–1273. [DOI] [PubMed] [Google Scholar]
- 24.Armstrong-Hough M, Turimumahoro P, Meyer AJ, et al. Drop-out from the tuberculosis contact investigation cascade in a routine public health setting in urban Uganda: a prospective, multi-center study. PLOS ONE 2017; 12: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nyirenda M, Sinfield R, Haves S, Molyneux EM, Graham SM. Poor attendance at a child TB contact clinic in Malawi. Int J Tuberc Lung Dis 2006; 10: 585–587. [PubMed] [Google Scholar]
- 26.Rutherford ME, Ruslami R, Anselmo M, et al. Management of children exposed to Mycobacterium tuberculosis: a public health evaluation in West Java, Indonesia. Bull World Heal Organ 2013; 91: 932–941A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hall C, Sukijthamapan P, dos Santos R, et al. Challenges to delivery of isoniazid preventive therapy in a cohort of children exposed to tuberculosis in Timor-Leste. Trop Med Int Health 2015; 20: 730–736. [DOI] [PubMed] [Google Scholar]
- 28.Rekha B, Jagarajamma K, Chandrasekaran V, Wares F, Sivanandham R, Swaminathan S. Improving screening and chemoprophylaxis among child contacts in India’s RNTCP: a pilot study. Int J Tuberc Lung Dis 2013; 17: 163–168. [DOI] [PubMed] [Google Scholar]
- 29.Tadesse Y, Gebre N, Daba S, et al. Uptake of isoniazid preventive therapy among under-five children: TB contact investigation as an entry point. PLOS ONE 2016; 11: e0155525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adjobimey M, Masserey E, Adjonou C, et al. Implementation of isoniazid preventive therapy in children aged under 5 years exposed to tuberculosis in Benin. Int J Tuberc Lung Dis 2016; 20: 1055–1059. [DOI] [PubMed] [Google Scholar]
- 31.Triasih R, Robertson CF, Duke T, Graham SM. A prospective evaluation of the symptom-based screening approach to the management of children who are contacts of tuberculosis cases. Clin Infect Dis 2015; 60: 12–18. [DOI] [PubMed] [Google Scholar]
- 32.Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis 2004; 8: 392–402. [PubMed] [Google Scholar]


