We read with interest the letter by Giustiniano et al.,1 who proposed a new approach for the echocardiographic assessment of patients with coronavirus disease 2019 (COVID-19) with acute respiratory distress syndrome (ARDS) during prone ventilation. Hemodynamic assessment using transthoracic echocardiography (TTE) is challenging in the prone position because acoustic windows are limited and difficult to obtain. Although the sole apical four-chamber view remains informative to evaluate central hemodynamics and identify ventricular dysfunction, it is intrinsically limited for the accurate identification of acute cor pulmonale (ACP), which affects about 20% of patients with ARDS.2 In contrast, transesophageal echocardiography (TEE) maintains its full diagnostic capacity and can be used safely for hemodynamic assessment during prone ventilation.3
Using TEE, we monitored five patients ventilated for severe COVID-19-related ARDS who were deemed at risk for hemodynamic instability at the time of prone positioning. Initially, the transesophageal probe was introduced under direct laryngoscopic guidance to perform a comprehensive hemodynamic assessment in the supine position. Subsequently, the patient was turned to the prone position, with particular attention to preventing any inadvertent dislodgement of both the endotracheal tube and the transesophageal probe.3 This allowed the assessment of potential hemodynamic consequences of body positioning due to abrupt changes in cardiac loading conditions and ventricular interactions. The transesophageal probe was removed in the presence of stable hemodynamics in the prone position. No complications were observed during or after transesophageal echocardiographic evaluations.
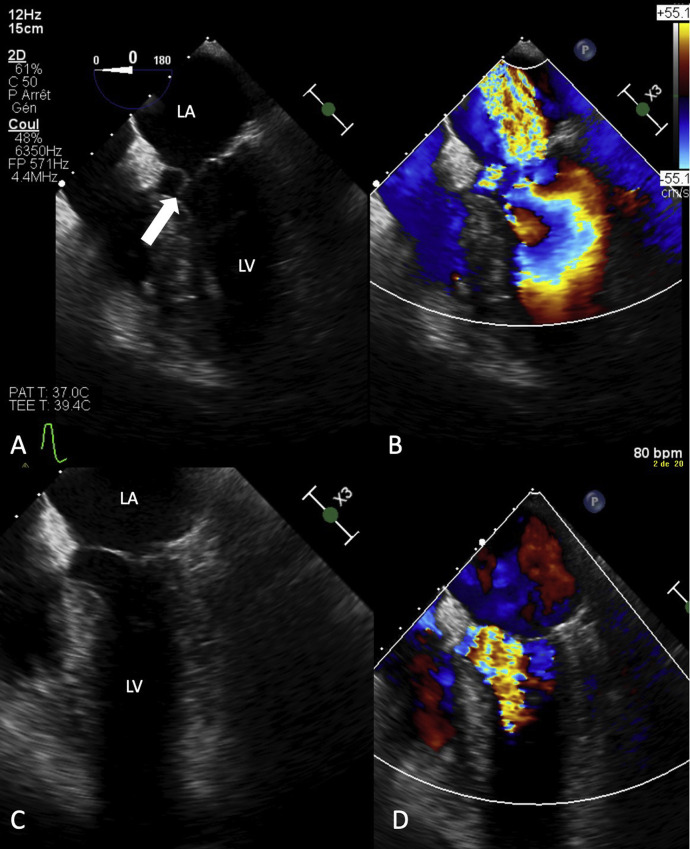
In 60% of these patients, image quality on TTE was suboptimal or poor in the semirecumbent supine position under high levels of positive end-expiratory pressure. ACP was depicted solely on TEE in one patient in the supine position. One hour after prone positioning, the eccentricity index measured in the transgastric short-axis view returned to normal, from 1.6 to 1.05. In another patient with severe hemodynamic instability at baseline, TTE was not contributory, while TEE depicted systolic anterior motion of the mitral valve associated with severe mitral regurgitation. Systolic anterior motion was ascribed to both hypovolemia and septal hypertrophy. A 1.5-L fluid loading resulted in reduction of the regurgitant volume, and both the systolic anterior motion and mitral regurgitation fully regressed in the prone position (Figure 1 ). The three remaining patients maintained a normal hemodynamic profile from the supine to the prone position during monitoring on TEE.
Figure 1.
Transesophageal four-chamber view in a mechanically ventilated patient with COVID-19 for severe ARDS obtained in both the supine and prone positions. TTE was not contributive, because of poor image quality. (A) In the semirecumbent supine position, systolic anterior motion of the mitral valve was seen (white arrow). (B) This abnormality was associated with severe mitral insufficiency, as reflected by a large regurgitant jet using color Doppler mapping. (C) After 1.5-L fluid resuscitation to correct underlying overt hypovolemia, the systolic anterior motion disappeared. (D) Associated mitral regurgitation fully regressed in the prone position, whereas aliasing during color Doppler mapping indicated the persistence of a moderate left ventricular outflow tract obstruction related to localized septal hypertrophy. The left ventricular outflow tract obstruction measured in the deep transgastric five-chamber view using continuous-wave Doppler decreased from 121 to 36 mm Hg after both fluid loading and prone positioning.
The short-axis view of the heart is essential for the diagnosis of ACP,4 which is prognostic when severe,2 because paradoxical septal motion is challenging to identify and the eccentricity index is not measurable in the four-chamber view. In addition, the greater diagnostic ability of TEE4 remains operant in the prone position, as illustrated in our patient with dynamic severe mitral regurgitation. Finally, only TEE provides a constant window to the superior vena cava to assess preload responsiveness in ventilated patients,5 even in the prone position.3 Because assessment using TEE is more cumbersome to routinely perform than TTE, especially in the setting of COVID-19, TTE may be used to properly select those patients who require monitoring with TEE during prone ventilation.
In our experience, TEE is highly feasible, is safe, and allows unparalleled monitoring of hemodynamic changes induced by prone ventilation in patients with ARDS. Compared with TTE, only TEE provides short-axis images of the heart for the identification of ACP and maintains its full diagnostic capacity during prone ventilation.
Footnotes
Conflicts of interest: None.
References
- 1.Giustiniano E., Bragato R.M., Padua E., Negri K., Cecconi M. Echocardiography during prone-position mechanical ventilation in patients with COVID-19: a proposal for a new approach. J Am Soc Echocardiogr. 2020;33 doi: 10.1016/j.echo.2020.04.027. 906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mekontso Dessap A., Boissier F., Charron C., Bégot E., Repessé X., Legras A. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42:862–870. doi: 10.1007/s00134-015-4141-2. [DOI] [PubMed] [Google Scholar]
- 3.Mekontso Dessap A., Proost O., Boissier F., Louis B., Roche Campo F., Brochard L. Transesophageal echocardiography in prone position during severe acute respiratory distress syndrome. Intensive Care Med. 2011;37:430–434. doi: 10.1007/s00134-010-2114-z. [DOI] [PubMed] [Google Scholar]
- 4.Lhéritier G., Legras A., Caille A., Lherm T., Mathonnet A., Frat J.-P. Prevalence and prognostic value of acute cor pulmonale and patent foramen ovale in ventilated patients with early acute respiratory distress syndrome: a multicenter study. Intensive Care Med. 2013;39:1734–1742. doi: 10.1007/s00134-013-3017-6. [DOI] [PubMed] [Google Scholar]
- 5.Vignon P., Repessé X., Bégot E., Léger J., Jacob C., Bouferrache K. Comparison of echocardiographic indices used to predict fluid responsiveness in ventilated patients. Am J Respir Crit Care Med. 2017;195:1022–1032. doi: 10.1164/rccm.201604-0844OC. [DOI] [PubMed] [Google Scholar]