Use of polypills combining multiple pharmacotherapies for cardiovascular disease prevention is a hot topic in cardiovascular medicine. In a low-resource, mostly black community in Alabama with an average 12% of 10-year cardiovascular disease risk, a pill combining a statin plus 3 antihypertensive medications that lowered blood pressure improved adherence and control of proximal risk factors.1 In Iran, a combination of aspirin, a statin, and 2 antihypertensive drugs reduced cardiovascular disease events in a mixed primary and secondary prevention population, including 11% individuals with established cardiovascular disease and 15% with diabetes, as compared to a “minimal care” intervention.2
These findings have resparked interest in scaling-up the use of polypills for cardiovascular prevention, from individual high-risk patients to entire populations at heterogeneous risk—the so-called polypill paradigm for population-level cardiovascular disease prevention.3 , 4 This was first proposed by Wald and Law in 2003, who projected that a pill combining 6 drugs could reduce the incidence of cardiovascular disease up to 80% in the United Kingdom.5 Multiple concerns were subsequently raised, including ethics issues, medicalization of prevention, potential for overtreatment of mostly low-risk individuals, pharmacological side effects, and costs. A few years later, Bittencourt et al demonstrated that implementation of the inclusion criteria of initial polypill population-level trials would define target populations comprising a majority of individuals unlikely to derive benefit.6
More recently, this paradigm has evolved to focus on “underserved populations” (ie, low-resource communities with poor access to health care that typically face higher rates of cardiovascular disease than those with more resources). The assumption is that treating the entire population of underserved communities with polypills could markedly curtail their rates of cardiovascular disease, potentially reducing disparities. This has been followed by a call for additional trials comparing population-level polypill-based interventions to more “precise” approaches.4 , 7
In our opinion, the use of pills combining various pharmacotherapies represents a promising approach with enormous potential to improve adherence and clinical outcomes in patients who require such medications. On the other hand, although we welcome any efforts aimed at improving the cardiovascular health of low-resource communities through interventions with the potential to improve equity, important conceptual issues arise when evaluating a population-level polypill paradigm for cardiovascular disease prevention. Importantly, although this approach is often confronted by precision medicine as its most intuitive counterargument,7 we pose that a social epidemiology perspective should also be brought into the conversation to fully characterize its strengths and weaknesses.
First, how would such an intervention be funded? Implementation would involve not only the production and distribution of millions of chronic polypills but also the development of a complex infrastructure aimed at ensuring trial-like long-term adherence in communities where poor adherence has traditionally represented a key barrier. Would current societal arrangements allowing communities to remain underserved in countries such as the United States be willing to fund such a costly intervention? Ensuring the necessary surveillance and treatment of pharmacological side effects would also prove challenging.
Our second concern relates to the conflation of polypill-based prevention interventions with Geoffrey Rose's “population-level” strategy.3 , 4 , 8 In his landmark Strategy of Preventive Medicine, Rose defined this as interventions aimed at reducing the incidence of disease in entire populations by addressing the fundamental factors (ie, mass influences, typically cultural and socioeconomic determinants) that cause some populations to have higher rates of disease than others.8 Rose's “population-level” interventions would not include scaled-up versions of high-risk individual approaches (such as the polypill)9 because these fail to address fundamental factors but, rather, proximal ones—for example, high cholesterol levels. Rose did not dismiss individual-level approaches but rather emphasized that their main benefit is on treating higher-risk individuals in whom the benefits outweigh the risks.8 On the other hand, from a population standpoint, the high-risk approach is akin to famine relief, which feeds the hungry in the short term but does not tackle the underlying causes that persist: “success is only palliative and temporary.”8
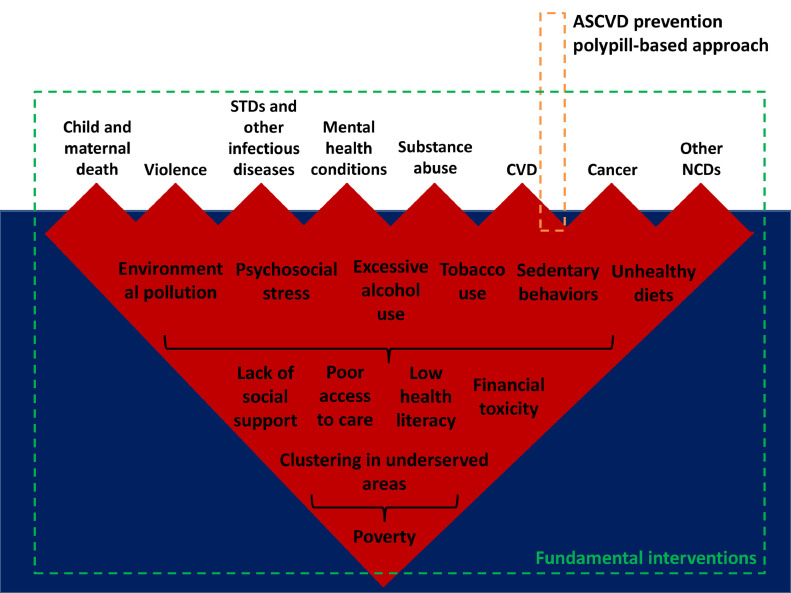
Third, in tackling the high burden of cardiovascular disease in underserved populations, there is a need to consider the underlying fundamental causes and their connection with other adverse health outcomes that disproportionately affect individuals of low socioeconomic status because this may be crucial to identify the most impactful and cost-effective interventions (Figure ). The association between poverty and these outcomes occurs through a variety of pathways and ultimately yields a markedly reduced quality of life and life expectancy. Consequently, ignoring fundamental causes and focusing on proximal factors may allow those fundamental causes to continue affecting health through other mechanisms. More radical, upstream approaches are likely to have a larger impact in the health of those communities.
Figure.
Poverty, health, and potential reach of polypill-based versus fundamental preventive interventions. ASCVD = atherosclerotic cardiovascular disease; CVD = cardiovascular disease; NCDs = noncommunicable diseases; STD = sexually transmitted diseases.
Another conceptual concern relates to the frequent comparison of the nature and potential benefits of a polypill approach with those of vaccines.4 In the absence of socioeconomic interventions that can prevent the occurrence of some viral outbreaks, such as the recent novel coronavirus 2019 pandemic, widespread vaccination becomes crucial to reduce the contagion of vulnerable persons through individual and, especially, herd immunity. Conversely, cardiovascular disease has well-established proximal risk factors and upward determinants, most of which are addressable. Moreover, polypills would provide only limited individual “immunity” and no herd protection. We humbly believe that avoidance of this analogy would help prevent misconceptions.
From a research standpoint, there have been calls for further trials as means to characterize the potential benefits of the polypill approach even further.4 , 7 Importantly, the control arm of a randomized trial should mimic the best currently existing intervention. According to the United Nations, “everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services.” In a recent trial in rural Pakistan, access to high-quality public health care curtailed mortality by more than 30% in just 24 months.10 With these recommendations and evidence already available, any future randomized trial of polypill in underserved communities in which at least 1 of the study arms does not include optimal access to health care (ie, tackles the status of “underserved”) would seem ethically questionable.
But do we need more trials in underserved communities? Access to care is already known to have indisputable, broad health benefits. More generally, interventions aimed at improving basic life conditions are tremendously powerful.8 For most, it would seem counterintuitive to fund a trial comparing water sanitation to an intervention based on the widespread use of chronic preventive antibiotic therapy. Or, as Rose put it: “[The high risk strategy] is analogous to vaccinating a population against cholera rather than improving their water supply.”8 An argument in favor of the use of polypills builds on the low feasibility of interventions tackling the status of underserved. For the same reason, should we devote millions of dollars to evaluate or implement large-scale pharmacological-based prevention approaches, or should those resources be invested in improving basic life conditions and access to care among underserved areas? The latter would likely reduce the incidence and case-fatality rates not only of cardiovascular disease but also of many other conditions in those communities.
Finally, we pose that discussions of interventions with the potential to affect large populations should be enriched with additional perspectives,8 including ethics, social values and priorities, and feasibility considerations. Civic society leaders, patient representatives, medical humanists, health systems managers, and even philosophers should be involved for further context and reflection. Albeit crucial, data alone falls short capturing the variety of considerations that need to be leveraged when building healthier and better societies. More importantly, we already have plenty of data demonstrating the benefits of improved life conditions and more equitable health care; we just need the will to implement them.
Footnotes
Funding: None.
Conflicts of Interest: None.
Authorship: Both authors had access to the data and a role in writing this manuscript.
References
- 1.Muñoz D, Uzoije P, Reynolds C. Polypill for cardiovascular disease prevention in an underserved population. N Engl J Med. 2019;381:1114–1123. doi: 10.1056/NEJMoa1815359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roshandel G, Khoshnia M, Poustchi H. Effectiveness of polypill for primary and secondary prevention of cardiovascular diseases (PolyIran): a pragmatic, cluster-randomised trial. Lancet. 2019;394:672–683. doi: 10.1016/S0140-6736(19)31791-X. [DOI] [PubMed] [Google Scholar]
- 3.The New York Times. This daily pill cut heart attacks by half. Why isn't everyone getting it? Available online at:https://www.nytimes.com/2019/08/22/health/heart-disease-iran-study.html. Accessed March 15, 2020.
- 4.Muñoz D, Wang TJ. The polypill revisited: why we still need population-based approaches in the precision medicine era. Circulation. 2019;140:1776–1778. doi: 10.1161/CIRCULATIONAHA.119.043491. [DOI] [PubMed] [Google Scholar]
- 5.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% BMJ. 2003;326:1419. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bittencourt MS, Blaha MJ, Blankstein R. Polypill therapy, subclinical atherosclerosis, and cardiovascular events-implications for the use of preventive pharmacotherapy: MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2014;63:434–443. doi: 10.1016/j.jacc.2013.08.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joyner MJ, Paneth N. Cardiovascular disease prevention at a crossroads: precision medicine or polypill? [e-pub ahead of print] JAMA. doi: 10.1001/jama.2019.19026. Accessed March 15, 2020. [DOI] [PubMed]
- 8.Rose G. Oxford University Press; Oxford: 1992. The Strategy of Preventive Medicine. [Google Scholar]
- 9.Frohlich KL. Commentary: what is a population-based intervention? Returning to Geoffrey Rose. Int J Epidemiol. 2014;43:1292–1293. doi: 10.1093/ije/dyu111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jafar TH, Gandhi M, de Silva HA. A community-based intervention for managing hypertension in rural South Asia. N Engl J Med. 2020;382:717–726. doi: 10.1056/NEJMoa1911965. [DOI] [PubMed] [Google Scholar]