To the Editors:
On December 31, 2019, the World Health Organization (WHO) was alerted about a cluster of pneumonia cases of unknown etiology in Wuhan, China [1]. By January 12, 2020, China had shared the genetic sequence of a novel coronavirus [2], later named severe acute coronavirus syndrome 2 (SARS-CoV-2), the etiological agent of Coronavirus Disease 2019 (COVID-19) [3]. Until today, the virus has spread to more than 200 countries, causing over 1.5 million cases and over 100,000 deaths [4]. COVID-19 was declared first a Public Health Emergency of International Concern (PHEIC) [5] and later a pandemic disease [6] by the WHO.
While recent published evidence describes the physical health impacts of COVID-19, there is paucity of research [7] regarding COVID-19–related mental health outcomes. Previously, quarantine measures had led to post-traumatic stress symptoms, confusion, and anger [8]. Although it is likely that COVID-19–related mental health impacts will only be manifested in the future, we can act today to prevent exposed adolescents and young adults (i.e., youths) from carrying mental health complications for decades after COVID-19. In the following paragraphs, we will explore the unique mental health risk and protective factors of Nepalese youths, who have been in complete lockdown since March 23 [9].
Risk Factors
The following are some COVID-19–related mental health risk factors in Nepalese youths: (1) deficient youth mental health services funding; (2) social media use; (3) a suddenly-imposed lockdown; (4) lack of understanding of lockdown restrictions; (5) sudden work/student life changes; (6) abrupt postponement of the Secondary Education Examination (SSE); and (7) exposure to devastating earthquakes in 2015.
In Nepal, there is insufficient funding of youth mental health services [10]. Underfunded mental health services may lead to increased negative mental health outcomes.
Access to Internet and social media has increased in recent years in Nepal. Social media use has been correlated with negative mental health outcomes such as stress and depression [11]. In addition, social media may become a source of health-related information during crises [12]. Youths might not have the capacity to handle the frequency or to analyze the accuracy [7] of information shared via social media. Recency [12] and sender (i.e., echo chambers [13]) of information may play an unbalanced role in assessing credibility, which may lead to misinformation and related stress/anxiety.
The implementation of a lockdown mandate with only a few hours of notice in Nepal left people unprepared for a long-term restriction on mobility. In addition, the social distancing and isolation that accompanies long-term lockdowns might be a risk factor for anxiety, mood disorders, and addictive and thought disorders [14].
Working youths cannot continue their work, either because their places of employment are closed or because they lack resources (i.e., computers) at home. For students, engagement in schools, in colleges, and with peers, which is a protective factor against adverse mental health outcomes [15], was suddenly interrupted.
Previous and multiple experiences of Nepali “lockdowns” (i.e., strikes or bandha and curfews) may have created a false expectation of “life-as-usual” activities during evenings. Conflicting information is associated with higher stress [7]. Misplaced expectations (arguably a type of conflicting information) may lead to anxiety and/or depression if and when authorities enforce the COVID-19 lockdown more strictly.
The SEE, a national examination that is commonly associated with stress/anxiety [16], was also postponed just hours before the scheduled time [17]. This abrupt cancellation and lack of information about SEE's future course left everyone involved in confusion and stress.
Nepalese youths experienced negative post-2015-earthquake mental health outcomes, including post-traumatic stress disorder [18]. A new emergency/crisis scenario may exacerbate those negative outcomes or generate new ones. Post-traumatic stress symptoms have been reported in Wuhan in the middle of the COVID-19 outbreak [19] in addition to adverse COVID-19 mental health outcomes associated with vicarious exposures [20].
Protective Factors
Mental health protective factors in Nepal may include the following: (1) cultural acceptance of facemasks; (2) family structure; (3) school space repurposing; and (4) availability of free counseling.
Facemasks are a common sight in Nepalese urban centers due to air pollution [21]. In the wake of COVID-19, traditional tailors (suchikar) have been sewing and gifting cloth masks. Altogether, these habits/measures may facilitate the implementation of CDC facemasks recommendations [22].
Joint and extended families are common in Nepal, which provide youths with a support system. As a result, youths are reconnecting with their family values and cultural identity. Increased support from friends and family have been reported in the context of COVID-19 [23].
School campuses are being used as potential quarantine and food collection sites, instilling a sense of social responsibility and community support that may negate adverse mental health outcomes [24]. Finally, trained counselors and psychologists are offering suggestions and psychological first aid (mostly free) via the Internet.
Conclusions
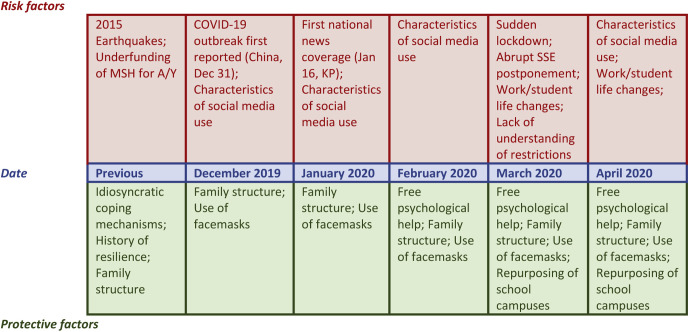
COVID-19 pandemic challenges are likely to lead to negative mental health outcomes among youths, especially in Nepal. Table 1 offers an analysis of risk/protective factors by levels of the socio-ecological model, whereas Figure 1 maps the chronological order on which risk/protective factors occurred (Figure 1).
Table 1.
Risk and protective factors for negative COVID-19–related mental health outcomes among adolescents and youths in Nepal by levels of action or interaction within the SEM
| SEM level | Risk factors | Protective factors |
|---|---|---|
| Individual | 1. Lack of understanding of lockdown restrictions 2. Exposure to 2015 earthquakes |
1. Personal coping strategies 2. History of resiliency in previous stressful situations |
| Relationship | 1. Social media | 1. Family structure |
| Community | 1. Work/sudent life changes | 1. Free psychological help |
| Societal | 1. Funding of MHS for A/Y 2. Sudden lockdown 3. Abrupt SSE postponement |
1. Cultural use of facemasks 2. Repurposing of school campuses |
A/Y = adolescents and youths; MHS = mental health services; SEM = socio-ecological model; SSE = secondary education examination.
Figure 1.
Chronological order of events related to risk and protective factors for COVID-19–related negative mental health outcomes among adolescents and youths in Nepal. A/Y = adolescents and youths; MHS = mental health services; SSE = secondary education examination.
References
- 1.WHO Pneumonia of unknown cause – China (5 January 2020) https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ Available at:
- 2.WHO Novel coronavirus – China (12 January 2020) https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ Available at:
- 3.WHO Naming the Coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it Available at:
- 4.WHO Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at:
- 5.WHO Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) Available at:
- 6.WHO WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 (11 March 2020) https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 7.Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020915212. 20764020915212. [DOI] [PubMed] [Google Scholar]
- 8.Brooks S.K., Webster R.K., Smith L.E. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Government of Nepal. Ministry of Health and Population ‘Situation report of COVID-19 #43’. https://drive.google.com/file/d/1z6XBao8nCS9OTmhlY-nU6sg15WUV4L-R/view Available at:
- 10.Chaulagain A., Kunwar A., Watts S. Child and adolescent mental health problems in Nepal: A scoping review. Int J Ment Health Syst. 2019;13:53. doi: 10.1186/s13033-019-0310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim K., Ryu E., Chon M.Y. Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: A questionnaire survey. Int J Nurs Stud. 2006;43:185–192. doi: 10.1016/j.ijnurstu.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Westerman D., Spence P.R., Van Der Heide B. Social media as information source: Recency of updates and credibility of information. J Computer-Mediated Commun. 2014;19:171–183. [Google Scholar]
- 13.Choi D., Chun S., Oh H. Rumor propagation is amplified by echo chambers in social media. Sci Rep. 2020;10:310. doi: 10.1038/s41598-019-57272-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sani G., Janiri D., Di Nicola M. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci. 2020 doi: 10.1111/pcn.13004. [DOI] [PubMed] [Google Scholar]
- 15.Bond L., Butler H., Thomas L. Social and school connectedness in early secondary school as predictors of late teenage substance use, mental health, and academic outcomes. J Adolesc Health. 2007;40 doi: 10.1016/j.jadohealth.2006.10.013. 357.e9–18. [DOI] [PubMed] [Google Scholar]
- 16.Bhattarai Y.B. Carleton University; Ottawa, ON, Canada: 2014. The school leaving certificate (SLC) examination of Nepal: Exploring negative consequences. [master’s thesis] [Google Scholar]
- 17.‘Notification about postponement of SEE exams’. The Government of Nepal. National Examination Board. https://www.see.gov.np/uploads/news/6uKFy6hDlnxstnju.pdf Available at:
- 18.Schwind J.S., Formby C.B., Santangelo S.L. Earthquake exposures and mental health outcomes in children and adolescents from Phulpingdanda village, Nepal: A cross-sectional study. Child Adolesc Psychiatry Ment Health. 2018;12:54. doi: 10.1186/s13034-018-0257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu N., Zhang F., Wei C. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Z., Ge J., Yang M. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gurung A., Bell M.L. Exposure to airborne particulate matter in Kathmandu Valley, Nepal. J Expo Sci Environ Epidemiol. 2012;22:235–242. doi: 10.1038/jes.2012.14. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention Recommendation regarding the use of cloth face coverings, especially in areas of significant community-based transmission. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html Available at: Accessed April 12, 2020.
- 23.Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wickrama K., Bryant C.M. Community context of social resources and adolescent mental health. J Marriage Fam. 2003;65:850–866. [Google Scholar]