Highlights
-
•
COVID-19 severe outcomes is associated with the respiratory failure and cytokine release syndrome with elevated IL-6 as a predicting parameter.
-
•
Chronic inflammation, associated with elevated inflammatory serum cytokines, including IL-6, may exacerbate SARS-CoV-2 induced pathology.
-
•
IL-6 is a promising therapeutic target for the anti-cytokine therapy of SARS-CoV-2 severe cases.
Keywords: IL-6, SARS-CoV-2, Cytokine release syndrome, Anti-cytokine therapeutics
Abstract
COVID-19 mortality is strongly associated with the development of severe pneumonia and acute respiratory distress syndrome with the worst outcome resulting in cytokine release syndrome and multiorgan failure. It is becoming critically important to identify at the early stage of the infection those patients who are prone to develop the most adverse effects. Elevated systemic interleukin-6 levels in patients with COVID-19 are considered as a relevant parameter in predicting most severe course of disease and the need for intensive care. This review discusses the mechanisms by which IL-6 may possibly contribute to disease exacerbation and the potential of therapeutic approaches based on anti-IL-6 biologics.
1. Introduction
At the end of 2019 and the beginning of 2020, first, China and then the rest of the world have been confronted with an outbreak of a new airborne transmitted coronavirus disease 2019 (COVID-19), a viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Just a few months later, there are already millions infected worldwide and with borders closed and strict travel bans imposed local transmission patterns are in place in most countries [1]. COVID-19 mortality rate appears to be in the range of 3,4–5,5% [2], which is significantly higher than that for seasonal flu caused by the influenza virus (1%), but lower than for both severe acute respiratory syndrome (SARS) (15 %) [3] and Middle East respiratory syndrome (MERS) (34 %) [4]. At the same time, the COVID-19 transmission rate is much greater than those of MERS or SARS, and poses a real threat to life for a large number of people worldwide, especially, in older patients with other co-morbidities [5]. Thus, in the absence of effective vaccines and treatments, early detection and the ability to define prognostic parameters predicting the course of the disease appear to be of particular interest.
2. COVID-19 pathogenesis and IL-6
Coronaviruses represent a large family of zoonotic respiratory viruses [6] that can cause both seasonal cold symptoms and fatal respiratory failure associated with severe inflammation of lower respiratory tract [7]. The major clinical symptoms of COVID-19 are similar to those experienced during a seasonal flu infection and include fever, dry cough, headache, myalgia and others. Co-morbidities such as cardiovascular diseases, diabetes, respiratory diseases, hypertension and age may exacerbate the disease manifestations [8,9]. Both moderate and severe COVID-19 infections cases may result in pneumonia with fluffy opacities on the chest computer tomographic scans, lung edema and accumulation of pleural fluid in the lungs [10,11]. Severe cases require invasive oxygen supply.
The exact molecular mechanisms of COVID-19-mediated pathogenesis are still under investigation. However, the lessons learned from SARS-CoV and MERS-CoV infections may uncover some key features of COVID-19-related pathologies, as well as molecular mediators and signaling pathways involved. The genetic sequence of SARS-CoV-2 [12], which was released almost simultaneously with the first reported cases [10] revealed that it belongs to the β‐coronavirus genus, with 79.0 % nucleotide identity to SARS‐CoV and 51.8 % identity to MERS-CoV. Inoculation with SARS-CoV-2 of human airway epithelial cells in vitro causes cytopathic effects [10] and cessation of the cilium beating of epithelial cells, similar to the cytopathic effect observed for SARS-CoV infection [13]. The initial step in viral infection was revealed by the crystal structure of SARS-CoV-2 spike receptor binding domain [14], which, just as SARS-CoV [15], binds to the host cell receptor angiotensin-converting enzyme 2 (ACE2). The presence of ACE2 on the cell membrane is crucial for virus virulence, as HeLa cells, lacking ACE2, are resistant to SARS-CoV-2 infection [16,17]. Structural analysis identified residues in the SARS-CoV-2 spike receptor binding domain that are critical for ACE2 binding, the majority of which either are highly conserved or share similar side chain properties with those of SARS-CoV. These similarities in virus entry between SARS-CoV-2 and SARS-CoV correlate with detectable cross-neutralizing activity of serum from SARS-CoV-recovered patients [18]. However, no available monoclonal antibodies targeting SARS-CoV receptor binding domain were able to prevent SARS-CoV-2 infecting the cells, highlighting unique intrinsic structure features of SARS-CoV-2 S-protein binding domain, including a much higher binding affinity than that of SARS-CoV S-protein [19]. In line with this, more recent study reports that human recombinant soluble ACE2 effectively, but not completely prevents SARS-CoV-2 infection, suggesting alternative mechanisms for viral entry [20].
Surface molecule CD147 (EMMPRIN or Basigin) is being considered as one alternative pathway for the virus to enter the host cells, since SARS-CoV-2 S-protein can bind CD147 as suggested by preliminary data [21]. CD147 is expressed on hematopoietic cells, including red blood cells, epithelial and neuronal cells [22]. Basigin is viewed as the molecular gate for plasmodium P.malariae [23]. Not surprisingly, CD147 is also associated with the HIV1 [24] and SARS-CoV [25] infections. In both cases, viral protein binds to the CD147 in complex with cyclophilin A (CyPA). SARS-CoV N-protein conjugates with CyPA inside ACE2-expressing infected host cells [25]. With this modification, newly assembled viral particles can infect CD147-positive cells. However, further studies are needed to evaluate possible impact of SARS-CoV-2 interaction with Basigin in the context of COVID-19.
ACE2, crucial for SARS-CoV-2 virulence, is expressed in the upper and the lower respiratory tract, most remarkably on lung alveolar epithelial cells, arterial and venous endothelial cells, as well as enterocytes of the small intestine, epithelial cells in the kidney. ACE2 expression is also detected in heart, pancreas, testis and brain [26]. Interestingly, ACE2 expression is not the highest in the upper respiratory tract [27,26], once again, supporting the hypothesis that increased transmissibility of SARS-CoV-2 as compared to SARS-CoV may be attributed to yet to be identified co-receptors or auxiliary factors adopted by SARS-CoV-2 [28]. Also, the fact that ACE2 is widely expressed in other tissues and organs explains a broad spectrum of adverse effects not limited just to the lungs. In addition, it was shown that SARS-CoV-2 directly infects ACE2-expressing tissue-resident CD169+ macrophages in the spleens and LNs, causing lymph follicle depletion, splenic nodule atrophy, histiocyte hyperplasia and lymphocyte reduction [29]. Thus, virus infection of macrophages, firstly, enhances viral spread and, secondly, triggers destructive events in the immune organs such as spleen and LNs. Recent data from the experiments using SARS-CoV-2 capsid or live virus infection of cultured T cell lines (MT-2 and A3.01) provides first evidence that SARS-CoV-2 could also infects T cells. However, expression level of ACE2 on T cells is low and, thus, CD147 is considered to mediate SARS-CoV-2 entry into T cells [17].
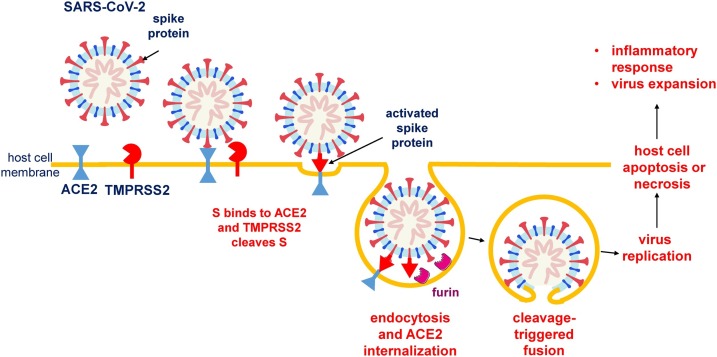
After virus binds to ACE2 (Fig. 1 ), serine protease, TMPRSS2, cleaves the viral spike protein. Then another protease, Furin, subsequently releases spike fusion peptide, and the virus enters the host cell through an endosomal pathway [18,30,31]. Following viral replication, assembly and release, the infected cells may undergo apoptosis or necrosis, triggering the inflammatory response with production of pro-inflammatory cytokines and activation of macrophages and Th1 cells, as well as production of IFNγ, IL-17A, IL-21, and IL-22 by neutrophils, Th17 and CD8+ cells. In turn, SARS-CoV-2 infection of recruited immune cells may increase their apoptosis and exacerbate lymphocytosis [32,33], and, finally, may lead in some patients to life-threatening conditions, such as respiratory distress syndrome, cytokine storm, and secondary hemophagocytic lymphohistiocytosis.
Fig. 1.
Schematic representation of SARS-CoV-2 interaction with a target cell.
Binding of virion to ACE2 is followed by serine protease, TMPRSS2, cleavage of the viral spike protein and induction of internalization of the complex with subsequent reduction of ACE2 surface availability. Then another protease, Furin, releases spike fusion peptide, and the virus enters the host cell through an endosomal pathway.
COVID-19 mortality is strongly associated with the development of severe respiratory distress syndrome, which requires invasive ventilation. It is important to identify those patients who are most likely to develop a severe form of the disease as early as possible. Based on the existing statistics, a number of clinical predictors of the disease deterioration and mortality, including the presence of secondary infections, lymphopenia [34], comorbidities such as cardiovascular and chronic respiratory diseases, diabetes, hypertension, obesity and cancer [35], increased cytokine production and serum ferritin [36] have been reported. The other study showed that the elevated serum creatinine, D-dimers, lactate dehydrogenase, C-reactive protein, procalcitonin, as well as increased white blood cell counts may indicate impending respiratory failure and the need for invasive oxygen supply [37]. Interestingly, in recently published reports elevated interleukin-6 (IL-6) level was proposed as a relevant parameter predicting the unwanted course of the disease and the need for mechanical ventilation [[38], [39], [40]]. These assumptions are consistent with data from a clinical trial in China that demonstrated on a small number of patients the efficacy of IL-6 neutralization during exacerbation of COVID-19 associated pneumonia [41] (Supplementary Table 1).
IL-6 is a cytokine with pleotropic functions ranging from hematopoiesis and metabolic regulation to inflammation, autoimmunity and acute phase response. IL-6 modulates host defense through a number of immune stimulating mechanisms: control of monocytes and their differentiation into macrophages [42], modulation of antigen-dependent B cell differentiation [43], increased IgG production by B cells [44], and promotion of Th2 response by inhibiting Th1 polarization [45]. Several studies revealed strong correlation between IL-6 levels in the serum and the upcoming respiratory failure [[46], [47], [48]]. It was shown, that even moderately elevated IL-6 levels above 80 pg/mL were sufficient to identify COVID-19 infected patients with a high risk of respiratory failure [37]. Moreover, serum SARS-CoV-2 nucleic acid (RNAaemia), which is strongly associated with cytokine storm, is closely correlated with extremely high IL-6 serum levels [47]. It was also suggested that serial measurement of circulating IL-6 might be important in identifying disease progression or, when evaluated immediately after COVID-19 diagnosis confirmation, may predict the upcoming respiratory failure or, alternatively, asymptomatic disease among SARS-CoV-2 infected patients [49].
Therefore, it would be valuable to explore the potential contribution of IL-6 in the events occurring during SARS-CoV-2 infection. The next section will discuss the mechanisms by which IL-6 may possibly affect the disease exacerbation and the potential of therapeutic approaches based on anti-IL-6 biologics.
3. Controversy concerning IL-6 functions during viral lung infections
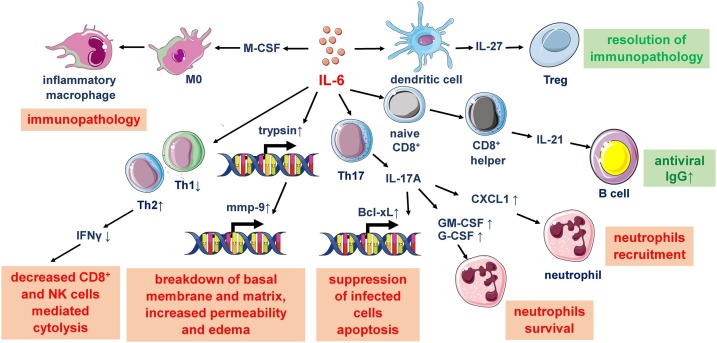
IL-6 is one of the key proinflammatory cytokines during infection onset, especially, at the mucosal sites [50]. However, the impact of IL-6 on the disease outcome may vary significantly (Fig. 2 ). On one hand, IL-6-dependent Th17 activation and differentiation are important for effective neutrophil migration, IL-6 together with IL-15 modulate cytolytic capacity of CD8+ T cells [51,52], and, finally, IL-6, as a pyrogenic cytokine, contributes to thermostatic regulation which is important for effective anti-viral response [53,54]. Studies, using IL-6-deficient mice, showed that IL-6 ameliorates acute lung injury in influenza A virus (IAV) infection [55]. IL-6-deficient mice infected with influenza virus exhibited higher lethality, as well as increased weight loss and fibroblast accumulation in the lungs associated with virus-induced apoptosis of lung epithelial cells and neutrophils [56] indicating that IL-6 may promote repair following virus-induced lung injury [57]. Finally, early IL-6 signaling promotes IL-27-dependent maturation of Treg cells in the lungs and resolution of viral immunopathology in mouse model of respiratory syncytial and influenza virus infection [58].
Fig. 2.
Role of IL-6 in respiratory viral infections.
IL-6 demonstrates opposing effects during the immune response to viral infections in the lungs. IL-6 promotes highly specific reaction of adaptive immunity by stimulating of CD8+ T cells and B cells, which is balanced by T regulatory cells. Also, IL-6 facilitates survival of phagocytic neutrophils. On the other hand, IL-6 can provide unfavorable Th2 and Th17 over Th1 helper differentiation and facilitate tissue injury by dysregulation of extracellular matrix and attraction of neutrophils and pro-inflammatory macrophages.
On the other hand, IL-6 has been implicated in the progression of viral infections. In this regard, IL-6 synergizes with IL-1b and TNF to upregulate trypsin expression, which activates matrix metalloproteinases and causes the breakdown of basal membrane and extracellular matrix, which, in turn, results in increased tissue permeability and edema [59]. Th1 cell-derived IFNγ is essential for effective antiviral immune response. However, IL-6 may inhibit Th1 polarization by stimulating CD4+ cells to differentiate into Th2 cells or by suppressing IFNγ expression [60,61]. Moreover, IL-6 promotes Th17 cell differentiation and IL-17A secretion, which, in turn, activates the expression of anti-apoptotic molecules, such as Bcl-XL, favoring survival of virus-infected cells in the model of persistent viral infection [62]. At the same time, IL-17 promotes the migration [63], and survival [64] of neutrophils which, in turn, contribute to the pathogenesis of COVID-19-driven ARDS [65]. Finally, in contrast to influenza virus infection, IL-6-deficient mice infected with murine pneumonia virus are characterized by better survival than WT mice with decreased lung edema and diminished neutrophil recruitment [66].
Taking into account that in several experimental models of viral lung infections IL-6 demonstrates either pathogenic [66] or protective [55] effects in vivo, the role of this cytokine in SARS-CoV-2 infection should be carefully evaluated. Moreover, the consequences of IL-6 induction in COVID-19 may vary depending on the infection stage and on the host immune status.
4. SARS-CoV-2-associated cytokine release syndrome
Patients with the most severe outcome of SARS-CoV-2 displayed high serum levels of proinflammatory cytokines responsible for cytokine storm induction [36,67]. Interestingly, the majority of severe COVID-19 cases with respiratory distress syndrome were associated with high systemic IL-1b, TNF and IL-6 levels, suggesting a direct connection between proinflammatory cytokine induction and adverse effects of COVID-19 [34]. As SARS-CoV-2 shows 79 % nucleotide identity to SARS-CoV, major pathogenic mechanisms, including cytokine storm and extensive lung damage during SARS and COVID-19 infection may be similar. Cytokine storm is a condition caused by extensive activation of the immune system, and, as a result, extremely high production of cytokines and chemokines. Since cytokine storm can lead to multiple organ failure, it is important to understand the mechanisms driving this condition.
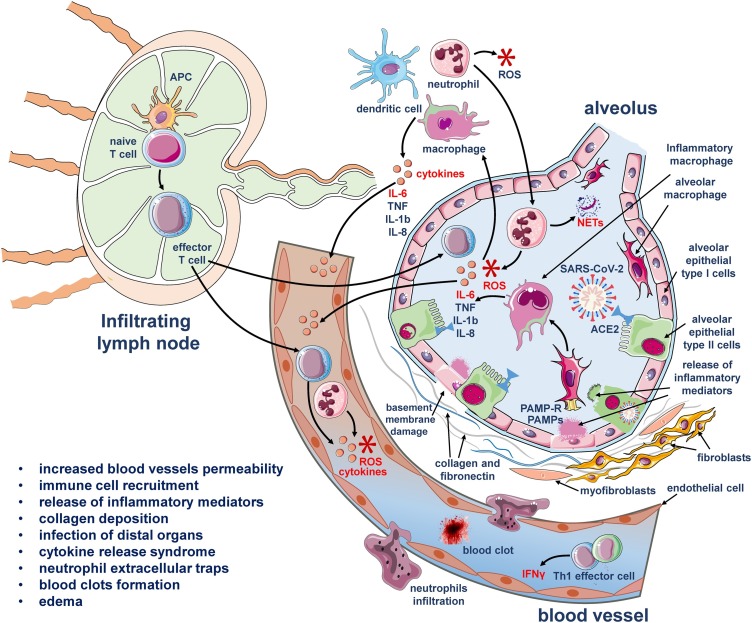
In lower respiratory tract SARS-CoV-2 infects predominantly type 2 alveolar epitheliocytes, the cell type which does not participate in active gas exchange. Following replication and disengagement of the lung epithelial layer, virus enters the underlying tissues and infects or is being captured by macrophages, dendritic cells and neutrophils, resulting in further viral spread [29] (Fig. 3 ). At the same time, damaged epitheliocytes release danger molecules which drive the activation of lung epithelium and resident immune cells. Thus, even at the early onset of viral infection, its penetration of the mucosa to the epithelial layer activates the innate immune response. Adaptive immunity is also activated during COVID-19, mainly by antigen presenting dendritic cells, which produce large amounts of cytokines, including IL-6, IL-1b and TNF and migrate to the regional lymph nodes to present viral antigen to naïve T cells, pushing their differentiation and migration into the affected tissue [68]. Specific humoral response represented by viral-specific antibody-producing B cells is also in place [69]. Replication of the virus results in further damage of affected organs together with self-boosting immune response manifesting to uncontrolled overexpression of inflammatory mediators in severe cases. Another mechanism driving cytokine storm during viral infections is increased blood vessel permeability which enables infiltration of effector cells, producing additional amounts of inflammatory molecules and exacerbating hyper cytokine production [70]. In addition, leakiness of blood vessels allows virus to spread to other tissues and organs, compromising their functions. Finally, under persistence of inflammatory factors, an increased number of inflammatory exudates and erythrocytes enter the alveoli, resulting in lung damage and respiratory failure syndrome.
Fig. 3.
Cytokine release syndrome in COVID-19.
SARS-CoV-2 replicates in alveolar epithelial cells. After the virions are released, they can infect or are being captured by macrophages, dendritic cells and neutrophils. At the same time, damaged epithelial cells produce alarmins, which are sensed by the neighboring epithelial and myeloid cells. All these events lead to release of proinflammatory cytokines, increase of alveolar vessel permeability and cell recruitment to the site of infection, forming positive loop for pathological activation of IL-6, IL-1, TNF and other proinflammatory cytokines. Due to high permeability of pulmonary vessels under inflammatory conditions, SARS-CoV-2 can inseminate distant ACE2-expressing tissues (intestine, kidney, pancreas), and trigger burst of inflammation at distant sites.
As mentioned above, severe COVID-19 induced pneumonia is marked by hyperactivation of the immune system and excessive production of IL-6 [36,67]. The main source of pathogenic IL-6 appears to be myeloid cells as their number is significantly increased among PBMC [69] and in BALF of severe COVID-19 patients [71]. Myeloid cell recruitment and activation in the lungs is associated with increased mortality and morbidity in SARS-CoV mouse model [72]. Human primary macrophages and dendritic cells can be infected, but they fail to support productive replication of SARS-CoV [73,74], unlike alveocytes, in which virus can replicate very quickly. At the same time, SARS-CoV and, apparently, SARS-CoV-2-infected macrophages demonstrate up-regulation of IL-6 production and low expression of interferons [29,73]. Interestingly, patients requiring intensive care and invasive lung ventilation display negative correlation between IL-6, TNF and IL-1b concentrations and CD4+ and CD8+ T cell counts [75], confirming previous studies in animal models, which suggested that cytokine storm actually dampens adaptive immunity against SARS-CoV infection [76]. Moreover, production of IFNγ by CD4+ T cells tended to be lower in severe as compared to moderate cases, suggesting that SARS-CoV-2 infection induces lymphopenia with the suppression of antiviral IFNγ production [36]. Furthermore, it has been suggested that this pathogenic IL-6 is likely to be produced by highly inflammatory macrophages [71], but not by alveolar macrophages, which are almost absent in the lung aspirates of severely affected patients [77]. At the same time, it should be noted that complete ablation of IL-6 at the very early stages of viral infection may result in depressed Tfh cell maturation and delayed antiviral antibody response [78].
It is known that acute inflammation and cytokine storm, as its extreme manifestation, can have a significant effect on hemodynamics and also on platelets and erythrocytes. The dysregulated coagulation cascade and the subsequent formation of intra-alveolar or systemic fibrin clots are prominent findings in previous zoonotic coronavirus infections (SARS and MERS) orchestrated by CRS [[79], [80], [81]]. COVID-19 patients also show significant changes in coagulative status (i.e. low platelet count, increased D-dimer, fibrinogen levels) and dysfunction of micro-vessels in pulmonary circulation [82,83], thus, thrombosis of the pulmonary capillaries is believed to contribute to rapidly developing hypoxia. The role of IL-6 in inflammatory hypercoagulation is controversial: IL-6 can increase the rate of fibrotic clot formation in whole blood, but the effect is less pronounced than it is shown for IL-1 or IL-8 [84]. On the other hand, IL-6 is important for thrombus formation being a regulator of MMPs and other thrombolysis-associated genes in macrophages [85].
Other characteristic feature of cytokine release syndrome is change in iron homeostasis and hyperferritinemia as indicated by high levels of serum ferritin [86]. In COVID-19 patients ferritin elevation correlated with poor prognosis [36], as it was an indication of hemolytic events caused by hypercoagulation and hemophagocytosis. In general, inadequate macrophage activation leads to pathologic phagocytosis of erythrocytes and reutilization of heme iron using ferritin [87]. In line with this, high systemic ferritin may serve as an indicator of developing macrophage activation syndrome, rather than a factor driving COVID-19 pathogenesis.
Another key proinflammatory cytokine, TNF, is also released abundantly during cytokine storm, caused by SARS-CoV-2 infection. Serum TNF levels were found to be elevated in severely affected COVID-19 patients [34]. Previously, it was shown for SARS-CoV that its spike protein is able to modulate TNF converting enzyme (TACE)-dependent shedding of the ACE2 ectodomain [88]. TACE expression is coupled to TNF production. Therefore, it is hypothesized that the use of TNF inhibitors may also show some efficacy in preventing viral entry [89], as well as in decreasing immunopathology associated mortality, as it was shown in preclinical studies in mice infected with severe respiratory syncytial virus [90]. Moreover, anti-TNF therapy was effective in decreasing the IL-6 and IL-1b serum levels in lethal bacteremia, suggesting that such treatment may provide complex anti-inflammatory effect [91]. Data obtained from COVID-19 infected patients with inflammatory bowel diseases undergoing anti-TNF therapy support safety of such intervention in the context of SARS-CoV-2 treatment [92,93]. These findings argue for a potentially protective effect of TNF inhibition in COVID-19 and further studies are needed to address this possibility.
5. ACE2 downregulation may induce IL-6 production in Angiotensin II-dependent manner
Hypertension has been suggested as a risk factor for severe COVID-19 outcomes [94]. Early data from the literature already assumed an association between blood pressure and circulating IL-6 levels in otherwise healthy individuals [95]. Moreover, several studies reported an increased IL-6 expression in patients with hypertension [96,97]. IL-6-transgenic mice, characterized by elevated plasma IL-6 levels, displayed pulmonary hypertension [98,99]. Taken together, this data suggest that IL-6 might be connected with increased risk of respiratory failure in hypertensive patients with COVID-19.
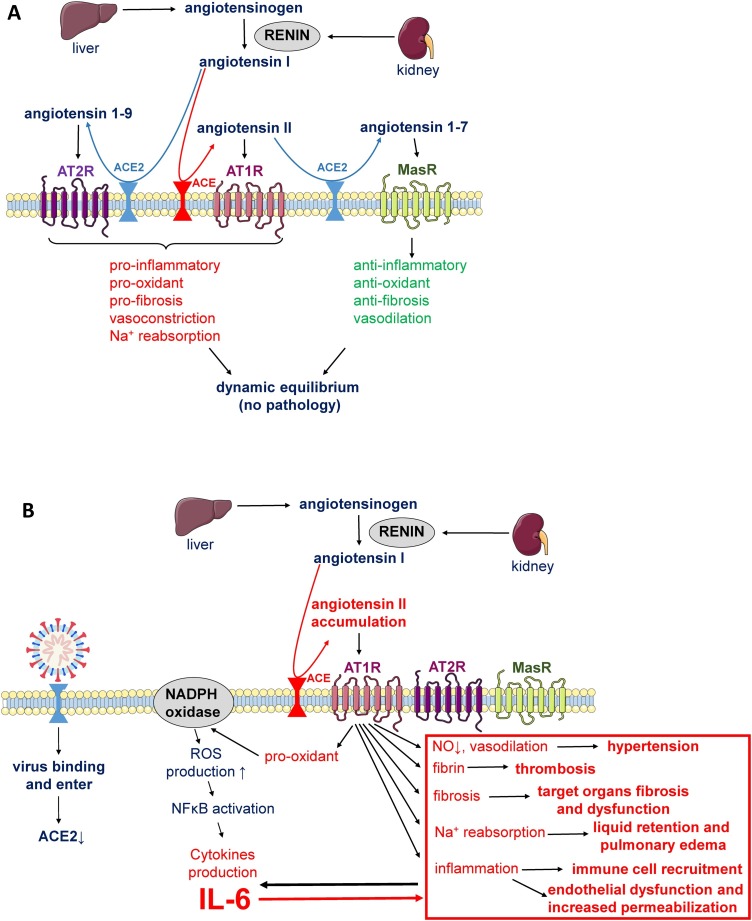
One of the mechanisms regulating blood pressure and electrolyte balance is angiotensin-renin system. It is comprised of two pathways, which are normally functioning in the state of dynamic equilibrium: ACE2-Angiotensin II–Angiotensin 1 Receptor axis, activating vasoconstriction and inflammatory response, and ACE2-Angiotensin 1–7-Mas receptor axis, supporting vasodilation and suppression of inflammation (Fig. 4 , A) [100]. Changes in renin-angiotensin system activity are related to the pathogenesis of hypertension and of inflammatory lung diseases, in particular, acute lung injury caused by viral infections [15,101].
Fig. 4.
ACE2 downregulation may drive IL-6 production in Angiotensin II-dependent manner.
A – in healthy state pro-inflammatory signaling of Angiotensin II via Angiotensin 1 receptor (AT1R) is stabilized by Angiotensin 1–7 (ACE2-Angiotensin I proteolysis product) signaling via Mas receptor (MasR) that has anti-inflammatory effect.
B – virus-mediated down-regulation of ACE2 leads to Angiotensin II accumulation in the absence of Angiotensin 1–7 and acceleration of its proinflammatory effect. AT1R downstream activation of NADPH oxidase results in elevated ROS directly promoting IL-6 expression. In its turn, IL-6 can positively regulate AT1R levels. Thus, by acting together these processes exacerbate hypertension, edema, infiltration of immune cells and inflammation in COVID-19 affected lungs.
SARS-CoV2 uses ACE2 as an entry site, thus, reducing ACE2 availability, promoting an imbalance between the ACE2-Angiotensin II–Angiotensin 1 receptor axis and the ACE2- Angiotensin 1–7-Mas receptor axis [15,102]. In line with this, recent studies have reported that COVID-19 patients have increased Angiotensin II compared to healthy individuals [103]. Altogether, the abovementioned data suggests that COVID-19 infection leads to imbalanced angiotensin conversion and a shift towards pro-inflammatory signaling mediated by Angiotensin 1 receptor axis [104] (Fig. 4, B).
Angiotensin II is known to significantly increase the expression of IL-6 in a dose-dependent manner [105] through pleiotropic activation of NF-kB transcription factors [106,107]. Angiotensin 1 receptor downstream activation of NADPH oxidase results in elevated oxidative stress, in particularly, superoxide that activates transcriptional mechanisms that directly promotes IL-6 gene expression. In turn, plasma IL-6 concentrations correlate with blood pressure, plasma Angiotensin II levels and vascular hypertrophy, suggesting an important role of IL-6 in the development and maintenance of hypertension, specifically, that mediated by Angiotensin II [108,109]. IL-6 promotes Angiotensin 1 receptor expression sensitizing the vascular wall to angiotensin II-dependent signaling mechanisms. Activated cells can release cytokines, including IL-6, which promote expression of adhesion molecules and induce endothelial activation, inflammatory cell infiltration and vascular inflammation [110]. This further drives oxidative stress and IL-6 expression. Therefore, it is plausible that IL-6 and Angiotensin II activate each other through a positive feedback mechanism. In support of this hypothesis, ACE2 protects against lethal avian influenza A H5N1 infection [111] through prevention of oxidative stress and acute respiratory distress syndrome. Moreover, it was recently reported that in COVID-19 patients with hypertension Angiotensin receptor blockade attenuated the inflammatory response, possibly through IL-6 inhibition [102,112]. Taking together, Angiotensin II accumulation due to SARS-CoV-2-mediated ACE2 downregulation may cause Angiotensin 1 receptor downstream activation of NADPH oxidase, which, in turn, leads to elevated ROS production and to induction of transcriptional mechanisms that directly promote IL-6 expression, implicated in inflammation-induced injury and immunopathology.
6. Risk factors associated with COVID-19
Chronic inflammation is the one common feature of hypertension, diabetes, obesity and age – the risk factors associated with COVID-19 severe outcomes. Elderly, obese and diabetic persons are affected by a low-grade chronic inflammation and are characterized by systemically increased levels of proinflammatory cytokines, which may contribute to and facilitate the cytokine storm, the main cause of COVID-19 mortality.
Among conditions, predisposing patients infected with SARS-CoV-2 to severe outcomes, diabetes is the most prominent. It is estimated that mortality rate of those with COVID-19 and diabetes is about 16 % [8] to 35 % [113]. IL-6 is known for its dual role in autoimmune diabetes, as it is involved in the development of insulin resistance and β-cell dysfunction and, at the same time, has anti-inflammatory effects and improves glucose metabolism [114]. Recent clinical data demonstrates significantly elevated systemic IL-6 in COVID-19 patients with diabetes as compared to those without diabetes [115]. COVID-19 may exacerbate the pre-existing diabetes, since its entry site, ACE2, is expressed in the pancreas, with a potential role in the development of insulin resistance and impaired insulin secretion [116]. IL-6 may be the link between diabetes and severe COVID-19 outcomes through its ability to modulate T cell response. Some indirect evidence to support this comes from mouse studies of closely related MERS-CoV infection demonstrating that abnormal elevation of IL-17A produced by IL-6-dependent Th17 cells exacerbates disease severity in diabetic mice [117]. Consistent with that finding, patients with COVID-19 have a higher proportion of Th17 cells in the blood [118], suggesting that diabetics due to improper activation of Th1 and Th17 cells may have a compromised anti-viral immune response [31].
Obese patients with COVID-19 are more likely to develop severe respiratory distress syndrome [119,120]. Just as diabetics, obese patients have higher concentration of proinflammatory cytokines both in steady state [121] and, apparently, during COVID-19 infection [8]. In addition to decreased anti-viral T cell response, enhanced IL-6 production by adipose tissue in obese patients [122] may alter innate anti-viral immune response by neutrophils [121] and cause uncontrolled replication of the virus at the early stages of infection.
From the very beginning of COVID-19 pandemic, age was identified as a risk factor [38], supporting the idea that ACE2 may be a marker of cell senescence [123]. Myofibroblasts, which increase in number with age, express high levels of ACE2 [124], thus, myofibroblasts are more susceptible to SARS-CoV-2, and elderly people, bearing higher proportion of myofibroblasts, might be more susceptible to COVID-19 infection (reviewed in [125]). IL-6 is a critical inflammatory regulator of senescence-associated secretory phenotype (SASP) [126]. Therefore, IL-6 overexpression may correlate both with senescent status of cells and tissues, as well as with increased expression of ACE2. In line with this idea, hydroxychloroquine, an anti-malaria drug, which is now approved in some countries for COVID-19 treatment, effectively reduced the salivary and serum levels of IL-6 in patients with Sjorgen’s syndrome [127]. Moreover, azithromycin, prescribed together with hydroxychloroquine, can target and selectively remove senescent cells [128] and, thus, provide anti-fibrotic activity by protecting the lungs from inflammation-induced injury [129,130].
Another issue facing elderly patients with COVID-19 is a compromised activation status of their effector T cells. These cells may display limited function during prolonged infection as a result of their exhaustion, associated with the surface expression of such immune-inhibitory factors as PD-1 [75]. Since aging itself is a process known to promote reorganization of the T cell landscape [131] and IL-6 is a SASP predictor and regulator, T cell exhaustion in the elderly patients with COVID-19 is much more evident due to higher basal concentration of IL-6, which can enhance the exhaustion process [132,133].
Smoking is another potential risk factor for SARS-CoV-2 infection. Smokers are more vulnerable to influenza virus infections [134,135] and are more likely to develop chronic obstructive pulmonary disease (COPD) [136]. Enhanced ACE2 expression had been reported in the lungs of healthy smokers [137,138]. In line with that, studies in mice have established that cigarette smoke can trigger the expansion of a subpopulation of respiratory epithelial cells that express ACE2 in a dose-dependent manner [139]. Patients with COPD, as well as active smokers, have increased ACE2 expression in the lungs [140], which may potentially explain a fourfold increased risk of adverse development and severe outcome of COVID-19 [141,142]. Taken together, these recent reports suggest that smokers may be at higher risk of infection. Examination of factors, predisposing to severe COVID-19 in Wuhan, China, revealed, that 19.2 % of patients with severe disease were smokers [143]. On the other hand, preliminary meta-analysis based on Chinese patients suggest that active smoking was not associated with the severity of COVID-19 [144], indicating that impact of smoking on COVID-19 progression is controversial and requires further assessment.
Intuitively, patients with pre-existing asthma should display higher proportion of COVID-19 severe cases. However, the prevalence of asthma in COVID-19 patients in Wuhan study was markedly lower (0,9%) than that reported in the adult population of Wuhan (6,4%) [143]. One possible explanation is a shift toward Th2-type immune response in asthmatics as opposed to Th1-associated inflammatory response induced by SARS-CoV-2 infection [118]. Recent study reveals that TMRSS2 expression in upper respiratory tract correlates positively with type 2 response genes, especially with IL-13, whereas ACE2 expression is suppressed by IL-13. Considering low numbers of cells co-expressing these proteases in the upper respiratory tract, it has been proposed that in the context of IL-13-dependent reduction in ACE2 expression allergy should promote resistance to infection [145]. In line with this, it was shown that ACE2 expression is decreased in nasal and bronchial epithelium of allergic individuals following allergen challenge, suggesting, that asthma-associated immune response actually protects from COVID-19-induced pathology [146]. Nevertheless, further studies are required to reveal the impact of COVID-19 severity in patients with preexisting asthma.
Meta-analysis studies of COVID-19 cases in China from December 2019 to February 2020 report lower incidence of the disease [147] and risk of death [35] in women than in men. Similar data on association of gender with poorer prognosis for males were obtained earlier for SARS-CoV [148,149], and MERS-CoV [150,151]. In connection to SARS-CoV-2, the X-linked ACE2 gene is of a particular interest. Significant fraction of genes encoded on the X chromosome undergo dosage compensation, however, ACE2 is located at Xp22, i.e. the area in which genes may escape from X chromosome inactivation [152], possibly contributing to gender disparity in disease susceptibility. Gender differences in immune responses are known to depend not only on genetic, but also on endocrine factors [153,154]. High doses of estradiol acting through estrogen receptors decrease production of proinflammatory cytokines via suppressing NF-kB signaling pathway [155]. In relation to COVID-19 the effects of estrogens on IL-6 and on disease progression is of particular interest. Estrogen may suppress LPS-mediated IL-6 expression in mouse macrophages by both blocking of NF-kB activation [155,156] and inhibiting p38 MAPK phosphorylation [156]. Furthermore, downregulation of IL-6 expression in Kupffer cells appears to be ERα-dependent [157]. Overall, immunomodulatory effects of estrogens may contribute to decreased susceptibility to SARS-CoV-2 infection in women and this question requires further study.
7. The aftermath of COVID-19 infection
One of the common complications from the respiratory viral infections, including SARS [158] and COVID-19 [159], is lung fibrosis. This is characterized by alveolar epithelial cell injury, recruitment and activation of fibroblasts and subsequent production of extracellular matrix (ECM) in the presence of specifically activated immune cells. Fibrosis develops as an exaggerated repair process following injury associated with abnormal immune response leading to chronic progressive disease [160]. Histological examination of lung biopsies from COVID-19 patients show massive apoptosis of pneumocytes, hyaline membrane formation, fibromyxoid exudates [161] which are manifestations that are characteristic for ARDS and represent key events preceding development of fibrosis (reviewed in [162]). Significant pro-fibrotic M2-like SPP1+macrophage infiltration was also described for COVID-19 correlating with the disease severity [71]. Damage to the epithelial layer caused by the virus further attracts various immune cells participating in inflammation-repair balance (monocytes, macrophages, granulocytes and T cells). In addition, some viral components, such as N-protein and papain-like protease, can directly stimulate production of TGF-β, one of the pro-fibrotic hallmarks in respiratory epithelium, similar to what has previously been reported for SARS-CoV [163,164].
The role of IL-6 had been extensively studied in bleomycin model of lung fibrosis in mice. Bleomycin is a chemotherapeutic antibiotic which causes damage of tissues lacking bleomycin hydrolase, predominantly, in the lungs [165]. Mice with genetic ablation of IL-6 were characterized by impaired fibrosis [166]. However, in the same model mice with pharmacological rather than genetic inhibition of IL-6 demonstrated opposing phenotypes depending on the phase of inflammation-repair cycle. Specifically, IL-6 neutralization at the early inflammatory phase (day 2 following bleomycin-induced lung injury) resulted in apoptosis of pneumocytes, which further contributed to pulmonary fibrosis, whereas IL-6 blockade at the early fibrotic stage (day 8 following bleomycin-induced lung injury) significantly ameliorated lung fibrosis [167]. Interestingly, treatment of mice with recombinant soluble gp130Fc at the late stage of chronic bleomycin model attenuated lung fibrosis, emphasizing the importance of sIL-6Ra and IL-6 trans-signaling in mediating this condition [168]. It was further suggested that M2-like infiltrating macrophages are the major source of soluble IL-6Ra in fibrotic foci, whereas pulmonary fibroblasts are the recipient cells, which proliferate and produce extracellular matrix under trans-IL-6 activation. Finally, overexpression of IL-6 in respiratory tract mediated by adenoviral vectors also resulted in the exacerbation of fibrosis and was associated with increased levels of M2-macrophages with pro-fibrotic features [169]. These pro-fibrotic macrophages are also characterized by increased IL-6Ra expression [168]. ACE2 expression is reported for lung, heart, kidney, intestine, liver and brain. Thus, similar fibrosis-associated complications should be expected, not just for respiratory tract, but also for other tissues and organs in correlation with viral load and severity of cytokine release syndrome. Summarizing the data available at the moment from infection-free experimental models of fibrosis, one can conclude that IL-6 may affect fibroblast proliferation and functions directly or through potentiation of a distinct macrophage phenotype. Taking into account the importance of this cytokine at the repair stage, anti-IL-6 therapy may prove beneficial not only in acute phase, but also in subacute proliferative phase of COVID-19-related ARDS.
SARS-CoV-2 tropism to neural system is of particular interest while neurological symptoms, such as dizziness, headache, ataxia and anosmia, are often found in mild COVID-19 patients and develop early in the infection [170]. ACE2 expression in CNS is attributed to the nuclei in brain stem and is associated with cardio‐respiratory control [171,172]. Recent study based on scRNA sequencing suggests co-expression of ACE2 and TMPRSS2 in olfactory epithelial cells, but not in mature olfactory sensory neurons, which were initially considered as the most obvious target population for the virus in CNS [173]. Even without the understanding of the exact mechanisms of SARS-CoV-2 penetration and distribution in CNS, it should be noted that as a result of the disseminated intravascular coagulopathy and cytokine storm caused by infection, blood-brain-barrier permeability is significantly increased, which can lead to negative consequences for CNS functioning [174,175].
8. Therapeutic potential of IL-6 inhibitors
An effective therapeutic approach should include a combination of specific antiviral drugs, which inhibit viral dissemination and limit direct virus-induced cytopathic effects coupled with anti-inflammatory therapeutics, directed against immunopathology induced by a viral infection [176]. SARS-CoV-2-induced immunopathology exhibits features of systemic hyper-inflammation reminiscent both of cytokine storm or macrophage activation syndrome and secondary haemophagocytic lymphohistocytosis [177]. Since overexpression of IL-6 appears to be associated with severe COVID-19 outcomes, neutralizing antibodies used to treat a number of autoimmune diseases by targeting exacerbated inflammatory immune response of the host may provide a life-saving approach by preventing the cytokine release syndrome. In line with that, patients responding to CD19 CAR T cell therapy experience cytokine release syndrome [178], which is well managed by IL-6 neutralizing antibodies [179]. In a non-randomized, open-label clinical trial, 21 patients with severe or critical COVID-19 were treated with a single dose of Tocilizumab, in addition to routine therapy [180]. 90 % of patients recovered, suggesting that anti-IL-6 might be a powerful potential rescue therapy in managing acute respiratory distress syndrome of COVID-19 and inhibiting the most adverse outcome. Peripheral mononuclear cell scRNA-seq profiling data obtained from these patients indicate that treatment with Tocilizumab does not reduce the number of cytotoxic CD8+ and plasma B cells, thus, does not interfere with robust adaptive immune response [69]. Preliminary data from 21 patients with COVID-19 who developed acute respiratory distress syndrome and participated in a compassionate-use program at Papa Giovanni XXIII hospital in Bergamo, Italy, indicate that intravenous introduction of Siltuximab reduced C-reactive protein level in all patients and significantly improved clinical conditions with a reduced need for ventilation in 33 % of patients. 43 % of patients showed stabilization of their conditions, and 24 % of patients experienced a worsening of the disease and required intubation [181].
Sarilumab is a monoclonal antibody that works by inhibiting the IL-6 pathway through binding and blocking the IL-6 receptor. Recently, another clinical trial was initiated, which will evaluate the effects of Sarilumab in patients with severe COVID-19. This U.S.-based multi-center, double-blind, phase 2/3 trial will begin at medical centers in New York and is anticipated to enroll up to 400 patients [182].
The overview of initiated clinical trials of anti-IL-6 therapeutics in COVID-19 patients is presented in Supplementary Table 1. In summary, strong scientific evidence of the beneficial impact of IL-6 inhibitors in the modulation of the COVID-19 infection requires further clinical data.
9. Conclusion
In the face of a pandemic, affecting millions of people worldwide, the need to develop new approaches or reassess the existing ones in the treatment of severe viral infections is more pressing than ever. Despite the fact that humanity experienced viral infections causing deadly pneumonia twice in the past 20 years, there are still no drugs specific for coronaviruses. The evidence discussed in this review suggests that for patients with risk factors, especially those with high systemic levels of IL-6, clinically approved neutralizing antibodies against IL-6 or its receptor, IL-6R, in combination with standard treatment protocols may provide benefit. Gaining a deeper understanding of the factors that influence the immune response and providing a mechanistic link of these factors to disease severity is crucial for the successful clinical management of COVID-19 in severely affected patients.
Funding
This work was partially supported by the Ministry of Science and Higher Education of the Russian Federation (grant 075-15-2019-1660). Research on pharmacological cytokine inhibition is supported by the Russian Science Foundation (grant 19-75-30032).
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Acknowledgments
We thank Prof. S. A. Nedospasov and Dr. K.-S. N. Atretkhany for critical reading of the manuscript. We thank P.V. Matveev for assistance with figure preparation.
Biographies
Ekaterina O. Gubernatorova is aPhD student in Immunology at Lomonosov Moscow State University (MSU) and a junior staff scientist in the Laboratory of Molecular Mechanisms of Immunity, Engelhardt Institute of Molecular Biology, Russian Academy of Sciences (EIMB RAS). Ekaterina is working on several research projects in the areas of mucosal immunology. She is focused on the role of cell-specific IL-6 signaling in lung and gut homeostasis and inflammation.
Ekaterina A. Gorshkova is a PhD student in Immunology at Lomonosov MSU and a junior staff scientist in the Laboratory of Molecular Mechanisms of Immunity and Center for Precision Genome Editing and Genetic Technologies for Biomedicine, EIMB RAS. Ekaterina is involved in several research projects, including studying the role of pathological IL-6 overexpression in murine model of inflammatory diseases.
Almina I. Polinova is a Master's student in Immunology in Lomonosov MSU and a research assistant in the Laboratory of Molecular Mechanisms of Immunity, EIMB RAS . Almina received her bachelor training in the laboratory of Molecular Mechanisms of Immunity, participating in a project on the role of IL-6 in gut inflammation.
Marina S. Drutskaya, PhD, is a leading staff scientist in Laboratory of Molecular Mechanisms of Immunity and Center for Precision Genome Editing and Genetic Technologies for Biomedicine, EIMB RAS. Marina is studying proinflammatory cytokines, mainly TNF and IL-6, in several relevant autoimmune and inflammatory disease models in mice, with a focus on cytokine inhibition.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.cytogfr.2020.05.009.
Contributor Information
E.O. Gubernatorova, Email: ekaterina.gubernatorova412@gmail.com.
M.S. Drutskaya, Email: marinadru@gmail.com.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.World Health Organization . 2020. Coronavirus Disease (COVID-19) Outbreak Situation.https://www.who.int/docs/default-source/coronaviruse/situation-reports/ [Google Scholar]
- 2.Worldometer . 2020. COVID-19 Coronavirus Pandemic.https://www.worldometers.info/coronavirus/ [Google Scholar]
- 3.World Health Organization . 2003. Update 49 - SARS Case Fatality Ratio, Incubation Period.https://www.who.int/csr/sars/archive/2003_05_07a/en/ [Google Scholar]
- 4.World Health Organization . 2019. Middle East Respiratory Syndrome Coronavirus (MERS-CoV)https://www.who.int/emergencies/mers-cov/en/ [Google Scholar]
- 5.Ruan S. Likelihood of survival of coronavirus disease. Lancet Infect. Dis. 2019;2020 doi: 10.1016/S1473-3099(20)30257-7. March 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woo P.C., Lau S.K., Huang Y., Yuen K.Y. Coronavirus diversity, phylogeny and interspecies jumping. Exp. Biol. Med. (Maywood) 2009;234:1117–1127. doi: 10.3181/0903-MR-94. [DOI] [PubMed] [Google Scholar]
- 7.Weiss S.R., Leibowitz J.L. Coronavirus pathogenesis. Adv. Virus Res. 2011;81:85–164. doi: 10.1016/B978-0-12-385885-6.00009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo W., Li M., Dong Y., Zhou H., Zhang Z., Tian C. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 2020:e3319. doi: 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020;(382):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;(382):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu X., Yu C., Qu J., Zhang L., Jiang S., Huang D. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging. 2020;(47):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Z., Ren L., Zhao X., Hung T., Meng A., Wang J. Inhibition of severe acute respiratory syndrome virus replication by small interfering RNAs in mammalian cells. J. Virol. 2004;78:7523–7527. doi: 10.1128/JVI.78.14.7523-7527.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lan J., Ge J., Yu J., Shan S., Zhou H., Fan S. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 15.Kuba K., Imai Y., Rao S., Gao H., Guo F., Guan B. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ou X., Liu Y., Lei X., Li P., Mi D., Ren L. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat. Commun. 2020;11:1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang X., Xu W., Hu G., Xia S., Sun Z., Liu Z. SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion. Cell. Mol. Immunol. 2020:1–3. doi: 10.1038/s41423-020-0424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monteil V., Kwon H., Prado P., Hagelkruys A., Wimmer R.A., Stahl M. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181(4):905–913. doi: 10.1016/j.cell.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang K., Chen W., Zhou Y.-S., Lian J.-Q., Zhang Z., Du P. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv. 2020 doi: 10.1101/2020.03.14.988345. March 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grass G.D., Toole B.P. How, with whom and when: an overview of CD147-mediated regulatory networks influencing matrix metalloproteinase activity. Biosci. Rep. 2015;36:e00283. doi: 10.1042/BSR20150256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crosnier C., Bustamante L.Y., Bartholdson S.J., Bei A.K., Theron M., Uchikawa M. Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum. Nature. 2011;480:534–537. doi: 10.1038/nature10606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pushkarsky T., Zybarth G., Dubrovsky L., Yurchenko V., Tang H., Guo H. CD147 facilitates HIV-1 infection by interacting with virus-associated cyclophilin A. Proc. Natl. Acad. Sci. U. S. A. 2001;98:6360–6365. doi: 10.1073/pnas.111583198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen Z., Mi L., Xu J., Yu J., Wang X., Jiang J. Function of HAb18G/CD147 in invasion of host cells by severe acute respiratory syndrome coronavirus. J. Infect. Dis. 2005;191:755–760. doi: 10.1086/427811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamming I., Timens W., Bulthuis M.L., Lely A.T., Navis G., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bertram S., Heurich A., Lavender H., Gierer S., Danisch S., Perin P. Influenza and SARS-coronavirus activating proteases TMPRSS2 and HAT are expressed at multiple sites in human respiratory and gastrointestinal tracts. PLoS One. 2012;7:e35876. doi: 10.1371/journal.pone.0035876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lukassen S., Chua R.L., Trefzer T., Kahn N.C., Schneider M.A., Muley T. SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 2020:e105114. doi: 10.15252/embj.20105114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen Y., Feng Z., Diao B., Wang R., Wang G., Wang C. 2020. The Novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Directly Decimates Human Spleens and Lymph Nodes. medRxiv. March 27. [DOI] [Google Scholar]
- 30.Walls A.C., Park Y.J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181(2):281–292. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muniyappa R., Gubbi S. COVID-19 pandemic, corona viruses, and diabetes mellitus. Am. J. Physiol. Endocrinol. Metab. 2020;318(5):E736–E741. doi: 10.1152/ajpendo.00124.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020;e200994 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang X., Yu Y., Xu J., Shu H., Ja Xia, Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8:e26. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;(395):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Worldometer . 2020, February. Age, Sex, Existing Conditions of COVID-19 Cases and Deaths; p. 29. [Google Scholar]
- 36.Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H. Clinical and immunologic features in severe and moderate Coronavirus Disease 2019. J. Clin. Invest. 2020;130(5):2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Herold T., Jurinovic V., Arnreich C., Hellmuth J.C., von Bergwelt-Baildon M., Klein M. 2020. Level of IL-6 Predicts Respiratory Failure in Hospitalized Symptomatic COVID-19 Patients. medRxiv. April 1. [DOI] [Google Scholar]
- 38.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gao Y., Li T., Han M., Li X., Wu D., Xu Y. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J. Med. Virol. 2020 doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gong J., Dong H., Xia S.Q., Huang Y.Z., Wang D., Zhao Y. 2020. Correlation Analysis Between Disease Severity and Inflammation-Related Parameters in Patients With COVID-19 Pneumonia. medRxiv. February 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu X. 2020. A Multicenter, Randomized Controlled Trial for the Efficacy and Safety of Tocilizumab in the Treatment of New Coronavirus Pneumonia (COVID-19). ChiCTR.https://clinicaltrials.gov/ct2/show/NCT04335071 [Google Scholar]
- 42.Chomarat P., Banchereau J., Davoust J., Palucka A.K. IL-6 switches the differentiation of monocytes from dendritic cells to macrophages. Nat. Immunol. 2000;1:510–514. doi: 10.1038/82763. [DOI] [PubMed] [Google Scholar]
- 43.Urashima M., Chauhan D., Hatziyanni M., Ogata A., Hollenbaugh D., Aruffo A. CD40 ligand triggers interleukin-6 mediated B cell differentiation. Leuk. Res. 1996;20:507–515. doi: 10.1016/0145-2126(95)00098-4. [DOI] [PubMed] [Google Scholar]
- 44.Yang R., Masters A.R., Fortner K.A., Champagne D.P., Yanguas-Casas N., Silberger D.J. IL-6 promotes the differentiation of a subset of naive CD8+ T cells into IL-21-producing B helper CD8+ T cells. J. Exp. Med. 2016;213:2281–2291. doi: 10.1084/jem.20160417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Diehl S., Rincon M. The two faces of IL-6 on Th1/Th2 differentiation. Mol. Immunol. 2002;39:531–536. doi: 10.1016/s0161-5890(02)00210-9. [DOI] [PubMed] [Google Scholar]
- 46.Coomes E.A., Haghbayan H. medRxiv; 2020. Interleukin-6 in COVID-19: A Systematic Review and Meta-Analysis. March 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen X., Zhao B., Qu Y., Chen Y., Xiong J., Feng Y., Men D., Huang Q., Liu Y., Yang B., Ding J. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa449. April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang C., Wu Z., Li J.W., Zhao H., Wang G.Q. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int. J. Antimicrob. Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ulhaq Z.S., Soraya G.V. Interleukin-6 as a potential biomarker of COVID-19 progression. Med. Mal. Infect. 2020;50(4):382–383. doi: 10.1016/j.medmal.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rose-John S., Winthrop K., Calabrese L. The role of IL-6 in host defence against infections: immunobiology and clinical implications. Nat. Rev. Rheumatol. 2017;13:399–409. doi: 10.1038/nrrheum.2017.83. [DOI] [PubMed] [Google Scholar]
- 51.Cox M.A., Kahan S.M., Zajac A.J. Anti-viral CD8 T cells and the cytokines that they love. Virology. 2013;435:157–169. doi: 10.1016/j.virol.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bottcher J.P., Schanz O., Garbers C., Zaremba A., Hegenbarth S., Kurts C. IL-6 trans-signaling-dependent rapid development of cytotoxic CD8+ T cell function. Cell Rep. 2014;8:1318–1327. doi: 10.1016/j.celrep.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 53.Eskilsson A., Mirrasekhian E., Dufour S., Schwaninger M., Engblom D., Blomqvist A. Immune-induced fever is mediated by IL-6 receptors on brain endothelial cells coupled to STAT3-dependent induction of brain endothelial prostaglandin synthesis. J. Neurosci. 2014;34:15957–15961. doi: 10.1523/JNEUROSCI.3520-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Evans S.S., Repasky E.A., Fisher D.T. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat. Rev. Immunol. 2015;15:335–349. doi: 10.1038/nri3843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang M.L., Wang C.T., Yang S.J., Leu C.H., Chen S.H., Wu C.L. IL-6 ameliorates acute lung injury in influenza virus infection. Sci. Rep. 2017;7:43829. doi: 10.1038/srep43829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dienz O., Rud J.G., Eaton S.M., Lanthier P.A., Burg E., Drew A. Essential role of IL-6 in protection against H1N1 influenza virus by promoting neutrophil survival in the lung. Mucosal Immunol. 2012;5:258–266. doi: 10.1038/mi.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lauder S.N., Jones E., Smart K., Bloom A., Williams A.S., Hindley J.P. Interleukin-6 limits influenza-induced inflammation and protects against fatal lung pathology. Eur. J. Immunol. 2013;43:2613–2625. doi: 10.1002/eji.201243018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pyle C.J., Uwadiae F.I., Swieboda D.P., Harker J.A. Early IL-6 signalling promotes IL-27 dependent maturation of regulatory T cells in the lungs and resolution of viral immunopathology. PLoS Pathog. 2017;13:e1006640. doi: 10.1371/journal.ppat.1006640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Indalao I.L., Sawabuchi T., Takahashi E., Kido H. IL-1beta is a key cytokine that induces trypsin upregulation in the influenza virus-cytokine-trypsin cycle. Arch. Virol. 2017;162:201–211. doi: 10.1007/s00705-016-3093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Velazquez-Salinas L., Verdugo-Rodriguez A., Rodriguez L.L., Borca M.V. The role of interleukin 6 during viral infections. Front. Microbiol. 2019;10:1057. doi: 10.3389/fmicb.2019.01057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu W., Dietze K.K., Gibbert K., Lang K.S., Trilling M., Yan H. TLR ligand induced IL-6 counter-regulates the anti-viral CD8(+) T cell response during an acute retrovirus infection. Sci. Rep. 2015;5:10501. doi: 10.1038/srep10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hou W., Kang H.S., Kim B.S. Th17 cells enhance viral persistence and inhibit T cell cytotoxicity in a model of chronic virus infection. J. Exp. Med. 2009;206:313–328. doi: 10.1084/jem.20082030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chuammitri P., Wongsawan K., Pringproa K., Thanawongnuwech R. Interleukin 17 (IL-17) manipulates mouse bone marrow- derived neutrophils in response to acute lung inflammation. Comp. Immunol. Microbiol. Infect. Dis. 2019;67:101356. doi: 10.1016/j.cimid.2019.101356. [DOI] [PubMed] [Google Scholar]
- 64.Liu R., Lauridsen H.M., Amezquita R.A., Pierce R.W., Jane-Wit D., Fang C. IL-17 promotes neutrophil-mediated immunity by activating microvascular pericytes and not endothelium. J. Immunol. 2016;197:2400–2408. doi: 10.4049/jimmunol.1600138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barnes B.J., Adrover J.M., Baxter-Stoltzfus A., Borczuk A., Cools-Lartigue J., Crawford J.M. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J. Exp. Med. 2020:217. doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Percopo C.M., Ma M., Brenner T.A., Krumholz J.O., Break T.J., Laky K. Critical adverse impact of IL-6 in acute pneumovirus infection. J. Immunol. 2019;202:871–882. doi: 10.4049/jimmunol.1800927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Monteleone G., Sarzi-Puttini P.C., Ardizzone S. Preventing COVID-19-induced pneumonia with anticytokine therapy. Lancet Rheumatol. 2020;(April 6) doi: 10.1016/S2665-9913(20)30092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guo C., Li B., Ma H., Wang X., Cai P., Yu Q. Tocilizumab treatment in severe COVID-19 patients attenuates the inflammatory storm incited by monocyte centric immune interactions revealed by single-cell analysis. bioRxiv. 2020;(April 8) doi: 10.1101/2020.04.08.029769. [DOI] [Google Scholar]
- 70.Tisoncik J.R., Korth M.J., Simmons C.P., Farrar J., Martin T.R., Katze M.G. Into the eye of the cytokine storm. Microbiol. Mol. Biol. Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liao M., Liu Y., Yuan J., Wen Y., Xu G., Zhao J., Cheng L., Li J., Wang X., Wang F., Liu L. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat. Med. 2020;12(May):1–3. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- 72.Channappanavar R., Fehr A.R., Vijay R., Mack M., Zhao J., Meyerholz D.K. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tseng C.T., Perrone L.A., Zhu H., Makino S., Peters C.J. Severe acute respiratory syndrome and the innate immune responses: modulation of effector cell function without productive infection. J. Immunol. 2005;174:7977–7985. doi: 10.4049/jimmunol.174.12.7977. [DOI] [PubMed] [Google Scholar]
- 74.Law H.K., Cheung C.Y., Ng H.Y., Sia S.F., Chan Y.O., Luk W. Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells. Blood. 2005;106:2366–2374. doi: 10.1182/blood-2004-10-4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Diao B., Wang C., Tan Y., Chen X., Liu Y., Ning L., Chen L., Li M., Liu Y., Wang G., Yuan Z. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front. Immunol. 2020;11(May 1):827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhao J., Zhao J., Van Rooijen N., Perlman S. Evasion by stealth: inefficient immune activation underlies poor T cell response and severe disease in SARS-CoV-infected mice. PLoS Pathog. 2009;5:e1000636. doi: 10.1371/journal.ppat.1000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bost P., Giladi A., Liu Y., Bendjelal Y., Xu G., David E. Host-viral infection maps reveal signatures of severe COVID-19 patients. Cell. 2020 doi: 10.1016/j.cell.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Karnowski A., Chevrier S., Belz G.T., Mount A., Emslie D., D’Costa K. B and T cells collaborate in antiviral responses via IL-6, IL-21, and transcriptional activator and coactivator, Oct2 and OBF-1. J. Exp. Med. 2012;209:2049–2064. doi: 10.1084/jem.20111504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liu Z.H., Wei R., Wu Y.P., Lisman T., Wang Z.X., Han J.J. Elevated plasma tissue-type plasminogen activator (t-PA) and soluble thrombomodulin in patients suffering from severe acute respiratory syndrome (SARS) as a possible index for prognosis and treatment strategy. Biomed. Environ. Sci. 2005;18:260–264. [PubMed] [Google Scholar]
- 80.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Giannis D., Ziogas I.A., Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J. Clin. Virol. 2020;127 doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Han H., Yang L., Liu R., Liu F., Wu K.L., Li J. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin. Chem. Lab. Med. 2020 doi: 10.1515/cclm-2020-0188. [DOI] [PubMed] [Google Scholar]
- 83.Shi C., Wang C., Wang H., Yang C., Cai F., Zeng F. medRxiv; 2020. The Potential of Low Molecular Weight Heparin to Mitigate Cytokine Storm in Severe COVID-19 Patients: A Retrospective Clinical Study. March 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bester J., Matshailwe C., Pretorius E. Simultaneous presence of hypercoagulation and increased clot lysis time due to IL-1beta, IL-6 and IL-8. Cytokine. 2018;110:237–242. doi: 10.1016/j.cyto.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 85.Nosaka M., Ishida Y., Kimura A., Kuninaka Y., Taruya A., Ozaki M. Crucial involvement of IL-6 in Thrombus resolution in mice via macrophage recruitment and the induction of proteolytic enzymes. Front. Immunol. 2019;10:3150. doi: 10.3389/fimmu.2019.03150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sackett K., Cunderlik M., Sahni N., Killeen A.A., Olson A.P. Extreme hyperferritinemia: causes and impact on diagnostic reasoning. Am. J. Clin. Pathol. 2016;145:646–650. doi: 10.1093/ajcp/aqw053. [DOI] [PubMed] [Google Scholar]
- 87.Crayne C.B., Albeituni S., Nichols K.E., Cron R.Q. The immunology of macrophage activation syndrome. Front. Immunol. 2019;10:119. doi: 10.3389/fimmu.2019.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Haga S., Yamamoto N., Nakai-Murakami C., Osawa Y., Tokunaga K., Sata T. Modulation of TNF-alpha-converting enzyme by the spike protein of SARS-CoV and ACE2 induces TNF-alpha production and facilitates viral entry. Proc. Natl. Acad. Sci. U. S. A. 2008;105:7809–7814. doi: 10.1073/pnas.0711241105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Feldmann M., Maini R.N., Woody J.N., Holgate S.T., Winter G., Rowland M. Trials of anti-tumour necrosis factor therapy for COVID-19 are urgently needed. Lancet. 2020 doi: 10.1016/S0140-6736(20)30858-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hussell T., Pennycook A., Openshaw P.J. Inhibition of tumor necrosis factor reduces the severity of virus-specific lung immunopathology. Eur. J. Immunol. 2001;31:2566–2573. doi: 10.1002/1521-4141(200109)31:9<2566::aid-immu2566>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 91.Fong Y., Tracey K.J., Moldawer L.L., Hesse D.G., Manogue K.B., Kenney J.S. Antibodies to cachectin/tumor necrosis factor reduce interleukin 1 beta and interleukin 6 appearance during lethal bacteremia. J. Exp. Med. 1989;170:1627–1633. doi: 10.1084/jem.170.5.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brenner E.J., Ungaro R.C., Colombel J.F., Kappelman M.D. 2020. SECURE-IBD Database Public Data Update. April 30. [Google Scholar]
- 93.Neurath M.F. Covid-19 and immunomodulation in IBD. Gut. 2020 doi: 10.1136/gutjnl-2020-321269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 95.Chae C.U., Lee R.T., Rifai N., Ridker P.M. Blood pressure and inflammation in apparently healthy men. Hypertension. 2001;38:399–403. doi: 10.1161/01.hyp.38.3.399. [DOI] [PubMed] [Google Scholar]
- 96.Gibas-Dorna M., Nowak D., Piatek J., Pupek-Musialik D., Krauss H., Kopczynski P. Plasma ghrelin and interleukin-6 levels correlate with body mass index and arterial blood pressure in males with essential hypertension. J. Physiol. Pharmacol. 2015;66:367–372. [PubMed] [Google Scholar]
- 97.Naya M., Tsukamoto T., Morita K., Katoh C., Furumoto T., Fujii S. Plasma interleukin-6 and tumor necrosis factor-alpha can predict coronary endothelial dysfunction in hypertensive patients. Hypertens. Res. 2007;30:541–548. doi: 10.1291/hypres.30.541. [DOI] [PubMed] [Google Scholar]
- 98.Suematsu S., Matsuda T., Aozasa K., Akira S., Nakano N., Ohno S. IgG1 plasmacytosis in interleukin 6 transgenic mice. Proc. Natl. Acad. Sci. U. S. A. 1989;86:7547–7551. doi: 10.1073/pnas.86.19.7547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Steiner M.K., Syrkina O.L., Kolliputi N., Mark E.J., Hales C.A., Waxman A.B. Interleukin-6 overexpression induces pulmonary hypertension. Circ. Res. 2009;104:236–244. doi: 10.1161/CIRCRESAHA.108.182014. 28p following 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hampl V., Herget J., Bibova J., Banasova A., Huskova Z., Vanourkova Z. Intrapulmonary activation of the angiotensin-converting enzyme type 2/angiotensin 1-7/G-protein-coupled Mas receptor axis attenuates pulmonary hypertension in Ren-2 transgenic rats exposed to chronic hypoxia. Physiol. Res. 2015;64:25–38. doi: 10.33549/physiolres.932861. [DOI] [PubMed] [Google Scholar]
- 101.Yang P., Gu H., Zhao Z., Wang W., Cao B., Lai C. Angiotensin-converting enzyme 2 (ACE2) mediates influenza H7N9 virus-induced acute lung injury. Sci. Rep. 2014;4:7027. doi: 10.1038/srep07027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Meng J., Xiao G., Zhang J., He X., Ou M., Bi J. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg. Microbes Infect. 2020;9:757–760. doi: 10.1080/22221751.2020.1746200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang X., Khaidakov M., Ding Z., Mitra S., Lu J., Liu S. Cross-talk between inflammation and angiotensin II: studies based on direct transfection of cardiomyocytes with AT1R and AT2R cDNA. Exp. Biol. Med. (Maywood) 2012;237:1394–1401. doi: 10.1258/ebm.2012.012212. [DOI] [PubMed] [Google Scholar]
- 105.Funakoshi Y., Ichiki T., Ito K., Takeshita A. Induction of interleukin-6 expression by angiotensin II in rat vascular smooth muscle cells. Hypertension. 1999;34:118–125. doi: 10.1161/01.hyp.34.1.118. [DOI] [PubMed] [Google Scholar]
- 106.Han Y., Runge M.S., Brasier A.R. Angiotensin II induces interleukin-6 transcription in vascular smooth muscle cells through pleiotropic activation of nuclear factor-kappa B transcription factors. Circ. Res. 1999;84:695–703. doi: 10.1161/01.res.84.6.695. [DOI] [PubMed] [Google Scholar]
- 107.Sano M., Fukuda K., Sato T., Kawaguchi H., Suematsu M., Matsuda S. ERK and p38 MAPK, but not NF-kappaB, are critically involved in reactive oxygen species-mediated induction of IL-6 by angiotensin II in cardiac fibroblasts. Circ. Res. 2001;89:661–669. doi: 10.1161/hh2001.098873. [DOI] [PubMed] [Google Scholar]
- 108.Gomolak J.R., Didion S.P. Angiotensin II-induced endothelial dysfunction is temporally linked with increases in interleukin-6 and vascular macrophage accumulation. Front. Physiol. 2014;5:396. doi: 10.3389/fphys.2014.00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ala Y., Palluy O., Favero J., Bonne C., Modat G., Dornand J. Hypoxia/reoxygenation stimulates endothelial cells to promote interleukin-1 and interleukin-6 production. Effects of free radical scavengers. Agents Actions. 1992;37:134–139. doi: 10.1007/BF01987902. [DOI] [PubMed] [Google Scholar]
- 110.Liu P.P., Blet A., Smyth D., Li H. The science underlying COVID-19: implications for the cardiovascular system. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 111.Zou Z., Yan Y., Shu Y., Gao R., Sun Y., Li X. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat. Commun. 2014;5:3594. doi: 10.1038/ncomms4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yang G., Tan Z., Zhou L., Yang M., Peng L., Liu J. Angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors usage is associated with improved inflammatory status and clinical outcomes in COVID-19 patients with hypertension. medRxiv. 2020;(March 31) doi: 10.1101/2020.03.31.20038935. [DOI] [PubMed] [Google Scholar]
- 113.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 114.Akbari M., Hassan-Zadeh V. IL-6 signalling pathways and the development of type 2 diabetes. Inflammopharmacology. 2018;26:685–698. doi: 10.1007/s10787-018-0458-0. [DOI] [PubMed] [Google Scholar]
- 115.Zhu L., She Z.G., Cheng X., Qin J.J., Zhang X.J., Cai J. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020 doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bindom S.M., Lazartigues E. The sweeter side of ACE2: physiological evidence for a role in diabetes. Mol. Cell. Endocrinol. 2009;302:193–202. doi: 10.1016/j.mce.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kulcsar K.A., Coleman C.M., Beck S.E., Frieman M.B. Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection. JCI Insight. 2019;4 doi: 10.1172/jci.insight.131774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang J.J., Dong X., Cao Y.Y., Yuan Y.D., Yang Y.B., Yan Y.Q. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 119.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Huang J.F., Wang X.B., Zheng K.I., Liu W.Y., Chen J.J., George J. Obesity hypoventilation syndrome and severe COVID-19. Metabolism. 2020 doi: 10.1016/j.metabol.2020.154249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Richard C., Wadowski M., Goruk S., Cameron L., Sharma A.M., Field C.J. Individuals with obesity and type 2 diabetes have additional immune dysfunction compared with obese individuals who are metabolically healthy. BMJ Open Diabetes Res. Care. 2017;5:e000379. doi: 10.1136/bmjdrc-2016-000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Maachi M., Pieroni L., Bruckert E., Jardel C., Fellahi S., Hainque B. Systemic low-grade inflammation is related to both circulating and adipose tissue TNFalpha, leptin and IL-6 levels in obese women. Int. J. Obes. Relat. Metab. Disord. 2004;28:993–997. doi: 10.1038/sj.ijo.0802718. [DOI] [PubMed] [Google Scholar]
- 123.Song J., Hu B., Qu H., Wang L., Huang X., Li M. Upregulation of angiotensin converting enzyme 2 by shear stress reduced inflammation and proliferation in vascular endothelial cells. Biochem. Biophys. Res. Commun. 2020;525:812–818. doi: 10.1016/j.bbrc.2020.02.151. [DOI] [PubMed] [Google Scholar]
- 124.Guy J.L., Lambert D.W., Turner A.J., Porter K.E. Functional angiotensin-converting enzyme 2 is expressed in human cardiac myofibroblasts. Exp. Physiol. 2008;93:579–588. doi: 10.1113/expphysiol.2007.040139. [DOI] [PubMed] [Google Scholar]
- 125.Sargiacomo C., Sotgia F., Lisanti M.P. COVID-19 and chronological aging: senolytics and other anti-aging drugs for the treatment or prevention of corona virus infection? Aging (Albany NY) 2020;12(8):6511–6517. doi: 10.18632/aging.103001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mosteiro L., Pantoja C., de Martino A., Serrano M. Senescence promotes in vivo reprogramming through p16(INK)(4a) and IL-6. Aging Cell. 2018;17 doi: 10.1111/acel.12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tishler M., Yaron I., Shirazi I., Yaron M. Hydroxychloroquine treatment for primary Sjogren’s syndrome: its effect on salivary and serum inflammatory markers. Ann. Rheum. Dis. 1999;58:253–256. doi: 10.1136/ard.58.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ozsvari B., Nuttall J.R., Sotgia F., Lisanti M.P. Azithromycin and Roxithromycin define a new family of "senolytic" drugs that target senescent human fibroblasts. Aging (Albany NY) 2018;10:3294–3307. doi: 10.18632/aging.101633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tang F., Li R., Xue J., Lan J., Xu H., Liu Y. Azithromycin attenuates acute radiation-induced lung injury in mice. Oncol. Lett. 2017;14:5211–5220. doi: 10.3892/ol.2017.6813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mosquera R.A., De Jesus-Rojas W., Stark J.M., Yadav A., Jon C.K., Atkins C.L. Role of prophylactic azithromycin to reduce airway inflammation and mortality in a RSV mouse infection model. Pediatr. Pulmonol. 2018;53:567–574. doi: 10.1002/ppul.23956. [DOI] [PubMed] [Google Scholar]
- 131.Elyahu Y., Hekselman I., Eizenberg-Magar I., Berner O., Strominger I., Schiller M. Aging promotes reorganization of the CD4 T cell landscape toward extreme regulatory and effector phenotypes. Sci. Adv. 2019;5 doi: 10.1126/sciadv.aaw8330. eaaw8330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kato T., Nishida T., Murase M., Ito Y., Murata M., Naoe T. Correlation of serum IL-6 level with exhaustion of cytomegalovirus-specific t cells after hematopoietic stem cell transplantation. Blood. 2011;118:360. doi: 10.1016/j.cellimm.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 133.Naseem S., Manzoor S., Javed A., Abbas S. Interleukin-6 rescues lymphocyte from apoptosis and exhaustion induced by chronic hepatitis C virus infection. Viral Immunol. 2018;31:624–631. doi: 10.1089/vim.2018.0045. [DOI] [PubMed] [Google Scholar]
- 134.Lawrence H., Hunter A., Murray R., Lim W.S., McKeever T. Cigarette smoking and the occurrence of influenza - systematic review. J. Infect. 2019;79:401–406. doi: 10.1016/j.jinf.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 135.Han L., Ran J., Mak Y.W., Suen L.K., Lee P.H., Peiris J.S.M. Smoking and influenza-associated morbidity and mortality: a systematic review and meta-analysis. Epidemiology. 2019;30:405–417. doi: 10.1097/EDE.0000000000000984. [DOI] [PubMed] [Google Scholar]
- 136.Ji W., Lim M.N., Bak S.H., Hong S.H., Han S.S., Lee S.J. Differences in chronic obstructive pulmonary disease phenotypes between non-smokers and smokers. Clin. Respir. J. 2018;12:666–673. doi: 10.1111/crj.12577. [DOI] [PubMed] [Google Scholar]
- 137.Cai G., Bosse Y., Xiao F., Kheradmand F., Amos C.I. Tobacco smoking increases the lung gene expression of ACE2, the receptor of SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020 doi: 10.1164/rccm.202003-0693LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Brake S.J., Barnsley K., Lu W., McAlinden K.D., Eapen M.S., Sohal S.S. Smoking upregulates angiotensin-converting enzyme-2 receptor: a potential adhesion site for novel coronavirus SARS-CoV-2 (Covid-19) J. Clin. Med. 2020;9 doi: 10.3390/jcm9030841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Smith J.C., Sausville E.L., Girish V., Yuan M.L., John K.M., Sheltzer J.M. Cigarette smoke exposure and inflammatory signaling increase the expression of the SARS-CoV-2 receptor ACE2 in the respiratory tract. Dev. Cell. 2020;(May 16) doi: 10.1016/j.devcel.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Leung J.M., Yang C.X., Tam A., Shaipanich T., Hackett T.L., Singhera G.K. ACE-2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur. Respir. J. 2020;55(5:2000688) doi: 10.1183/13993003.00688-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhao Q., Meng M., Kumar R., Wu Y., Huang J., Lian N. The impact of COPD and smoking history on the severity of Covid-19: a systemic review and meta-analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wang B., Li R., Lu Z., Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12:6049–6057. doi: 10.18632/aging.103000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020 doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lippi G., Henry B.M. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19) Eur. J. Intern. Med. 2020;(75):107–108. doi: 10.1016/j.ejim.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sajuthi S.P., DeFord P., Jackson N.D., Montgomery M.T., Everman Jamie L., Rios C.L. Type 2 and interferon inflammation strongly regulate SARS-CoV-2 related gene expression in the airway epithelium. bioRxiv. 2020 doi: 10.1101/2020.04.09.034454. April 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Jackson D.J., Busse W.W., Bacharier L.B., Kattan M., O’Connor G.T., Wood R.A. Association of respiratory allergy, asthma and expression of the SARS-CoV-2 receptor, ACE2. J. Allergy Clin. Immunol. 2020 doi: 10.1016/j.jaci.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Li L.Q., Huang T., Wang Y.Q., Wang Z.P., Liang Y., Huang T.B. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Karlberg J., Chong D.S., Lai W.Y. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am. J. Epidemiol. 2004;159:229–231. doi: 10.1093/aje/kwh056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Leong H.N., Earnest A., Lim H.H., Chin C.F., Tan C., Puhaindran M.E. SARS in Singapore--predictors of disease severity. Ann Acad Med Singapore. 2006;35:326–331. [PubMed] [Google Scholar]
- 150.Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int. J. Infect. Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Alghamdi I.G., Hussain I.I., Almalki S.S., Alghamdi M.S., Alghamdi M.S., El-Sheemy M.A. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int. J. Gen. Med. 2014;7:417–423. doi: 10.2147/IJGM.S67061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Burrell L.M., Harrap S.B., Velkoska E., Patel S.K. The ACE2 gene: its potential as a functional candidate for cardiovascular disease. Clin. Sci. 2013;124:65–76. doi: 10.1042/CS20120269. [DOI] [PubMed] [Google Scholar]
- 153.Klein S.L., Flanagan K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016;16:626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 154.La Vignera S., Cannarella R., Condorelli R.A., Torre F., Aversa A., Calogero A.E. Sex-specific SARS-CoV-2 mortality: among hormone-modulated ACE2 expression, risk of venous thromboembolism and hypovitaminosis D. Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21082948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Biswas D.K., Singh S., Shi Q., Pardee A.B., Iglehart J.D. Crossroads of estrogen receptor and NF-kappaB signaling. Sci. STKE. 2005;2005:pe27. doi: 10.1126/stke.2882005pe27. [DOI] [PubMed] [Google Scholar]
- 156.Liu L., Zhao Y., Xie K., Sun X., Jiang L., Gao Y. Estrogen inhibits LPS-induced IL-6 production in macrophages partially via the nongenomic pathway. Immunol. Invest. 2014;43:693–704. doi: 10.3109/08820139.2014.917095. [DOI] [PubMed] [Google Scholar]
- 157.Naugler W.E., Sakurai T., Kim S., Maeda S., Kim K., Elsharkawy A.M. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science. 2007;317:121–124. doi: 10.1126/science.1140485. [DOI] [PubMed] [Google Scholar]
- 158.van den Brand J.M., Haagmans B.L., van Riel D., Osterhaus A.D., Kuiken T. The pathology and pathogenesis of experimental severe acute respiratory syndrome and influenza in animal models. J. Comp. Pathol. 2014;151:83–112. doi: 10.1016/j.jcpa.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Xu Y.H., Dong J.H., An W.M., Lv X.Y., Yin X.P., Zhang J.Z. Clinical and computed tomographic imaging features of novel coronavirus pneumonia caused by SARS-CoV-2. J. Infect. 2020;80:394–400. doi: 10.1016/j.jinf.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Florez-Sampedro L., Song S., Melgert B.N. The diversity of myeloid immune cells shaping wound repair and fibrosis in the lung. Regeneration (Oxf.) 2018;5:3–25. doi: 10.1002/reg2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cabrera-Benitez N.E., Laffey J.G., Parotto M., Spieth P.M., Villar J., Zhang H. Mechanical ventilation-associated lung fibrosis in acute respiratory distress syndrome: a significant contributor to poor outcome. Anesthesiology. 2014;121:189–198. doi: 10.1097/ALN.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhao X., Nicholls J.M., Chen Y.G. Severe acute respiratory syndrome-associated coronavirus nucleocapsid protein interacts with Smad3 and modulates transforming growth factor-beta signaling. J. Biol. Chem. 2008;283:3272–3280. doi: 10.1074/jbc.M708033200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Li S.W., Yang T.C., Wan L., Lin Y.J., Tsai F.J., Lai C.C. Correlation between TGF-beta1 expression and proteomic profiling induced by severe acute respiratory syndrome coronavirus papain-like protease. Proteomics. 2012;12:3193–3205. doi: 10.1002/pmic.201200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Liu T., De Los Santos F.G., Phan S.H. The bleomycin model of pulmonary fibrosis. Methods Mol. Biol. 2017;1627:27–42. doi: 10.1007/978-1-4939-7113-8_2. [DOI] [PubMed] [Google Scholar]
- 166.Saito F., Tasaka S., Inoue K., Miyamoto K., Nakano Y., Ogawa Y. Role of interleukin-6 in bleomycin-induced lung inflammatory changes in mice. Am. J. Respir. Cell Mol. Biol. 2008;38:566–571. doi: 10.1165/rcmb.2007-0299OC. [DOI] [PubMed] [Google Scholar]
- 167.Kobayashi T., Tanaka K., Fujita T., Umezawa H., Amano H., Yoshioka K. Bidirectional role of IL-6 signal in pathogenesis of lung fibrosis. Respir. Res. 2015;16:99. doi: 10.1186/s12931-015-0261-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Le T.T., Karmouty-Quintana H., Melicoff E., Le TT Weng T., Chen N.Y. Blockade of IL-6 Trans signaling attenuates pulmonary fibrosis. J. Immunol. 2014;193:3755–3768. doi: 10.4049/jimmunol.1302470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ayaub E.A., Dubey A., Imani J., Botelho F., Kolb M.R.J., Richards C.D. Overexpression of OSM and IL-6 impacts the polarization of pro-fibrotic macrophages and the development of bleomycin-induced lung fibrosis. Sci. Rep. 2017;7:13281. doi: 10.1038/s41598-017-13511-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Mao L., Wang M., Chen S., He Q., Chang J., Hong C. Neurological Manifestations of hospitalized Patients with COVID-19 in Wuhan, China: a retrospective case series study. JAMA Neurol. 2020;(April 10) doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yamazato M., Yamazato Y., Sun C., Diez-Freire C., Raizada M.K. Overexpression of angiotensin-converting enzyme 2 in the rostral ventrolateral medulla causes long-term decrease in blood pressure in the spontaneously hypertensive rats. Hypertension. 2007;49:926–931. doi: 10.1161/01.HYP.0000259942.38108.20. [DOI] [PubMed] [Google Scholar]
- 172.Feng Y., Yue X., Xia H., Bindom S.M., Hickman P.J., Filipeanu C.M. Angiotensin-converting enzyme 2 overexpression in the subfornical organ prevents the angiotensin II-mediated pressor and drinking responses and is associated with angiotensin II type 1 receptor downregulation. Circ. Res. 2008;102:729–736. doi: 10.1161/CIRCRESAHA.107.169110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Brann D.H., Tsukahara T., Weinreb C., Lipovsek M., Van den Berge K., Gong B. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. bioRxiv. 2020;(March 25) doi: 10.1101/2020.03.25.009084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Clark I.A., Vissel B. The meteorology of cytokine storms, and the clinical usefulness of this knowledge. Semin. Immunopathol. 2017;39:505–516. doi: 10.1007/s00281-017-0628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yokota S., Imagawa T., Miyamae T., Ito S., Nakajima S., Nezu A. Hypothetical pathophysiology of acute encephalopathy and encephalitis related to influenza virus infection and hypothermia therapy. Pediatr Int. 2000;42:197–203. doi: 10.1046/j.1442-200x.2000.01204.x. [DOI] [PubMed] [Google Scholar]
- 176.Stebbing J., Phelan A., Griffin I., Tucker C., Oechsle O., Smith D. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect. Dis. 2020;20:400–402. doi: 10.1016/S1473-3099(20)30132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.McGonagle D., Sharif K., O’Regan A., Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun. Rev. 2020:102537. doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Teachey D.T., Lacey S.F., Shaw P.A., Melenhorst J.J., Maude S.L., Frey N. Identification of predictive biomarkers for cytokine release syndrome after chimeric antigen receptor T-cell therapy for acute lymphoblastic leukemia. Cancer Discov. 2016;6:664–679. doi: 10.1158/2159-8290.CD-16-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Agarwal S., June C.H. Harnessing CAR t cell insights to develop treatments for hyperinflammatory responses in COVID-19 patients. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-20-0473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Xu X., Han M., Li T., Sun W., Wang D., Fu B. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. U. S. A. 2020;117(20):10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Gritti G., Raimondi F., Ripamonti D., Riva I., Landi F., Alborghetti L. Use of siltuximab in patients with COVID-19 pneumonia requiring ventilatory support. medRxiv. 2020;(April 1) doi: 10.1101/2020.04.01.20048561. [DOI] [Google Scholar]
- 182.Sanofi . 2020. Sanofi and Regeneron Begin Global Kevzara® (sarilumab) Clinical Trial Program in Patients With Severe COVID-19.http://www.news.sanofi.us/2020-03-16-Sanofi-and-Regeneron-begin-global-Kevzara-R-sarilumab-clinical-trial-program-in-patients-with-severe-COVID-19 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.