Abstract
Background
Because of the rapid spread of COVID-19, on March 8, 2020 Italy became a “protected area”: people were told not to leave their homes unless it was essential. The aim of this study was to evaluate the activity of our trauma center, relative to shoulder and elbow, in the 30 days starting from March 8, 2020, the first day of restrictions in Italy, and to compare it with the same days of 2019 to weigh the impact of COVID-19 on shoulder and elbow trauma.
Materials and methods
Patients managed in our trauma center between March 8, 2020, and April 8, 2020 (COVID period), for shoulder and elbow trauma were retrospectively included and compared to patients admitted in the same period of 2019 (no-COVID period). Clinical records of all participants were examined to obtain information regarding age, sex, mechanism of injury, and diagnosis.
Results
During the no-COVID period, 133 patients were admitted for a shoulder or elbow trauma; in the COVID period, there were 47 patients (65% less first aid). In the no-COVID and COVID period, patients with shoulder contusion totaled 60 (14.78% of all; male [M]: 34; female [F]: 26; mean age 51.8 years, range 18-88) and 11 (12.09% of all contusions; M: 7, F: 4; mean age 43 years, range 24-60), respectively. In the no-COVID period, 27 fractures (9.34% of all fractures) involved the shoulder, whereas 18 fractures (8.69%) were registered in the COVID period. In the no-COVID period, 14 elbow fractures were treated (4.8% of all fractures), compared with 4 in the COVID period. In the no-COVID and COVID periods, 6 patients (M: 5, F: 1; mean age 42 years, range 21-64) and 2 patients (M: 1, F: 1; mean age 29.5 years, range 24-35) reported having a feeling of momentary post-traumatic shoulder instability, and 0 and 1 patients (M: 1, F: 0; age 56 years), respectively, reported similar symptoms at the elbow. Finally, first or recurrent dislocations in the no-COVID period were 10, and in the COVID period, 7; elbow dislocations in the no-COVID period were 2, and in the COVID period, there were 3.
Conclusions
During the COVID period, we provided a reduced number of health services, especially for patients with low-energy trauma and for those who underwent sports and traffic accidents. However, during the COVID period, elderly subjects remain exposed to shoulder and elbow trauma due to low-energy (domestic) falls. The subsequent hospitalization of these patients has contributed to making it more difficult to manage the hospital wards that are partly occupied by COVID-19 patients.
Keywords: COVID-19 and shoulder trauma, proximal humerus fractures, radial head fractures, COVID-19 and traumatology, COVID-19 shoulder impact, shoulder and elbow trauma
On January 29, 2020, the Italian Authorities declared the first cases of Coronavirus in Italy: 2 Chinese tourists coming from Wuhan, China, who were hospitalized at Spallanzani Hospital, the reference center for infectious diseases in Rome. In addition, an Italian researcher from China with COVID-19 and a 17-year-old with flulike symptoms but negative for COVID-19, who had been stuck in Wuhan for a long time, were hospitalized at Spallanzani Hospital in the same period.
On January 30, the World Health Organization (WHO) declared a global state of emergency, and on February 11 gave a name to the new disease, COVID-19, and to the new virus, Sars-CoV-2.23
February 21 is a fundamental date in Italy: several cases of COVID-19 had emerged in the Lodi area in Lombardy (the most populated region of Italy); significantly, these were people who did not come from China. The affected cities were subsequently closed so that nobody could leave or enter them.
In the following days, the COVID-19 infections continued to rise, and on March 4 the Italian Government closed schools and universities. On this day, the positive cases totaled 2700.
On March 8, the decree that would isolate Lombardy, the most affected region, and 14 other provinces, was signed. All these areas became “red zones.” The same day, the Italian Prime Minister announces that the measures already taken for Lombardy and for the 14 other provinces have been extended to the whole country so that Italy becomes a “protected area.” People across Italy are told not to leave their homes unless it was essential. Smart working is imposed; movement is strictly limited, and on March 22, the Government cracks down further, forbidding unnecessary travel between towns. Travel is only allowed for “urgent, verifiable work situations and emergencies or health reasons.” People who have tested positive for COVID-19 must not leave their homes for any reason, and anyone with a fever or respiratory symptoms are strongly encouraged to stay at home and limit social contact, including with their family doctor. People are allowed to go outside for one of the following reasons:
-
•
an urgent, demonstrable work-related reason;
-
•
health reasons; or
-
•
situations of need (eg, to buy food).
In addition, Italy's latest step in its coronavirus lockdown is to close down all productive activity throughout the territory that is not strictly necessary, crucial, or indispensable, to guarantee essential goods and services, starting from March 28. All this information can be extracted from the Italian Civil Protection website.22
The current restrictions have inevitably modified the Orthopedic practice, in particular those of our trauma center. Our aim was to evaluate the activity of a trauma center, relative to shoulder and elbow, serving a highly populated suburban area, in a 30-day period starting from March 8, 2020, the first day of restrictions in Italy, and to compare it with the same days of 2019 in order to weigh the impact of COVID-19 on shoulder and elbow trauma.
Materials and methods
All the skeletally mature (older than 18 years) patients managed in the emergency unit of our hospital between March 8, 2020, and April 8, 2020 (COVID period) for a shoulder and elbow trauma were retrospectively included and compared with patients admitted in the same period of 2019 (no-COVID period). Our country protects health as a fundamental right of the individual and community and guarantees free care.
Clinical records of all participants were examined by 2 of the authors in order to obtain information regarding age, sex, mechanism of injury, and diagnosis.
Four categories of diagnoses were distinguished: contusion, fracture, sprain/subluxation, and dislocation.
According to the mechanism of injury, we arbitrarily distinguished 6 subgroups: (1) accidental fall; (2) sports trauma; (3) high-energy trauma incurred by car, motorcycle, or public transport accident as occupant or as pedestrian involvement; (4) accident at work; (5) trauma due to assault or beatings; and (6) gunshot and stab wounds.
Statistical analysis
Continuous variables were expressed by the mean and standard deviation (SD) and were evaluated by Student t test or Mann Whitney U test. The categorical data were expressed as number and percentage (%) and were evaluated by chi-square or Fisher exact test. The level of significance was set at P < .05. SPSS, version 23.0, was used to perform all the tests (IBM, Armonk, NY, USA).
Results
In March-April 2019 (no-COVID period), in our trauma center, there were 1349 accesses; in the same month of the following year (COVID period), the accesses were 474, which was two-thirds less (P < .05). During the no-COVID time, 133 patients reported to our trauma center for a shoulder and/or elbow trauma; instead, patients treated during the COVID period for the same reasons were 47 (P < .05). Therefore, we performed 65% less first-aid shoulder/elbow services. Six and 1 patients, during the no-COVID and COVID period, respectively, underwent multiple fractures. Of them, no patients had shoulder and/or elbow fractures. No patients underwent shoulder/elbow trauma due to gunshot and stab wounds (subgroup 6); therefore, this subgroup is not mentioned in the tables.
In the no-COVID and COVID periods, patients who received a diagnosis of shoulder contusion were 60 (14.78% of the 406 contusions that occurred on the whole body; male [M]: 34, female [F]: 26; mean age 51.8 years, range 18-88) and 11 (12.09% of 91 contusions; M: 7, F: 4; mean age 43 years, range 24-60), respectively. Elbow contusions were 14 (3.4% of 406 contusions; M: 9, F: 5; mean age 50.2 years, range 18-80) in the no-COVID period and 1 (1.1% of 91 contusions; M: 1, F: 0; age 29 years) in the COVID period. Table I shows the traumatic mechanism responsible for shoulder and elbow contusion in the 2 examined periods.
Table I.
Mechanisms of injury responsible for shoulder and elbow contusion in the 2 examined periods
| Accidental fall | Sports trauma | High-energy (traffic accident) | Accident at work | Assault/beatings | |
|---|---|---|---|---|---|
| Shoulder contusions | |||||
| No-COVID period | 36 | 6 | 14 | 2 | 2 |
| COVID period | 4 | 2 | 4 | 0 | 1 |
| Elbow contusions | |||||
| No-COVID period | 7 | 1 | 4 | 2 | 0 |
| COVID period | 1 | 0 | 0 | 0 | 0 |
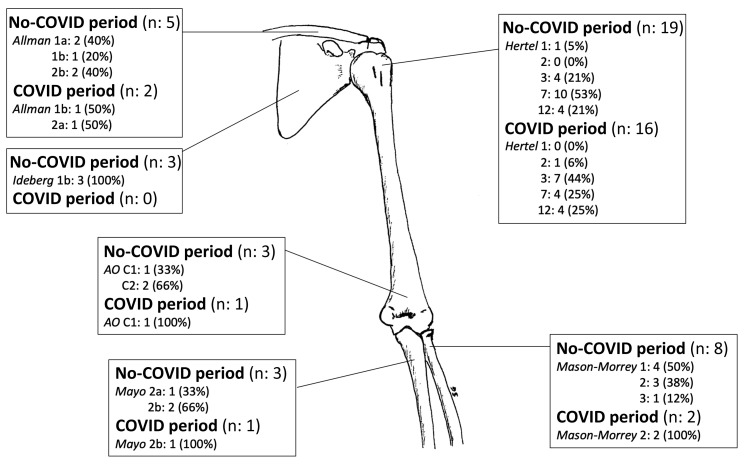
In the no-COVID time, we treated 289 fractures; 27 of them (9.34%) involved the shoulder girdle. In particular, 19 fractures (70.4% of shoulder fractures) involved the humeral head (M: 3, F: 16; mean age 71.8 years, range 35-85), 5 fractures (18.5%) the clavicle (M: 5; mean age 51 years, range 29-91), and 3 fractures (11.1%) the glenoid surface (M: 3; mean age 45.7 years , range 40-50). In the COVID period, we treated 207 fractures; 18 of them (8.69%) involved the shoulder: 16 humeral head fractures (88.9%; M: 3, F: 13; mean age 69.8 years, range 43-91), 2 clavicle fractures (11.1%; M: 2; mean age 60 years, range 39-81), and none involving the scapula (0%). Figure 1 shows the humeral, clavicular, and scapular fractures according to Hertel,3 Allman,1 and Ideberg10 classification, respectively, in the 2 examined periods. Table II shows the mechanism of injury of these fractures.
Figure 1.
Distribution of shoulder and elbow fractures in the no-COVID and COVID periods.
Table II.
Mechanisms of injury responsible for humeral head, clavicle, and glenoid surface fractures in the no-COVID and COVID periods
| Accidental fall | Sports trauma | High-energy (traffic accident) | Accident at work | Assault/ beatings | |
|---|---|---|---|---|---|
| Humeral head | |||||
| No-COVID period | 18 | 0 | 0 | 1 | 0 |
| COVID period | 16 | 0 | 0 | 0 | 0 |
| Clavicle | |||||
| No-COVID period | 1 | 3 | 1 | 0 | 0 |
| COVID period | 1 | 0 | 1 | 0 | 0 |
| Glenoid surface | |||||
| No-COVID period | 0 | 3 | 0 | 0 | 0 |
| COVID period | 0 | 0 | 0 | 0 | 0 |
Fourteen elbow fractures were treated in the no-COVID time (4.8% of all fractures). In particular, 3 affected the humerus (21.4%; M: 1, F: 2; mean age 67.3 years, range 46-84), 3 the ulna (21.4%; M: 1, F: 2; mean age 77.3 years, range 66-83), and 8 the radial head (57.1%; M: 2, F: 6; mean age 50.7 years, range 19-83). Of the 207 fractures that occurred during the COVID period, 4 (1.9%) involved the elbow; in particular, 1 affected the humerus (25%; F: 1; age 51 years), 1 the ulna (25%; M: 1; age 94 years), and 2 the radial head (50%; F: 2; mean age 66.5 years, range 64-69). Figure 1 and Table III show the treated elbow type fractures according to AO,19 Mayo,6 and Mason16 classification and the traumatic mechanism responsible for the fractures in the 2 examined periods.
Table III.
Mechanisms of injury responsible for distal humerus, proximal ulna, and radial head fractures in the 2 examined periods
| Accidental fall | Sports trauma | High-energy (traffic accident) | Accident at work | Assault/beatings | |
|---|---|---|---|---|---|
| Distal humerus | |||||
| No-COVID period | 3 | 0 | 0 | 0 | 0 |
| COVID period | 1 | 0 | 0 | 0 | 0 |
| Proximal ulna | |||||
| No-COVID period | 3 | 0 | 0 | 0 | 0 |
| COVID period | 1 | 0 | 0 | 0 | 0 |
| Radial head | |||||
| No-COVID period | 7 | 1 | 0 | 0 | 0 |
| COVID period | 1 | 0 | 1 | 0 | 0 |
In the no-COVID and COVID periods, 6 patients (M: 5, F: 1; mean age 42 years, range 21-64) and 2 patients (M: 1, F: 1; mean age 29.5 years, range 24-35) reported having a feeling of momentary post-traumatic shoulder instability (no previous episodes of true dislocations); patients with similar sensation, but at the elbow, were 0 and 1 (M: 1; age 56 years), respectively. Table IV shows the traumatic mechanism responsible for shoulder and elbow sprain/subluxation in the 2 examined periods.
Table IV.
Mechanisms of injury responsible for shoulder and elbow sprains/subluxations in the no-COVID and COVID periods
| Accidental fall | Sports trauma | High-energy (traffic accident) | Accident at work | Assault/beatings | |
|---|---|---|---|---|---|
| Shoulder sprain/subluxations | |||||
| No-COVID period | 5 | 1 | 0 | 0 | 0 |
| COVID period | 1 | 0 | 0 | 1 | 0 |
| Elbow sprain/subluxations | |||||
| No-COVID period | 0 | 0 | 0 | 0 | 0 |
| COVID period | 0 | 0 | 0 | 1 | 0 |
Finally, first dislocation or recurrence episodes in the no-COVID period were 10 (58.8% of all joint dislocations that occurred in the same period; M: 5, F: 5; mean age 44.8 years, range 22-84); instead, in the COVID period, we treated 7 patients (53.8% of all joint dislocations; M: 4, F: 3; mean age 47.6 years, range 26-80). In the no-COVID period, elbow dislocations comprised 2 cases (2 terrible triads; 11.76% of all joint dislocations occurred in that time; M: 2; mean age 63.5, range 42-85); instead, in the COVID period, patients with elbow dislocation totaled 3 (2 terrible triads and 1 posteromedial instability; 23.08% of all joint dislocations occurred in that time; M: 2, F: 1; mean age 27.3 years, range 24-32). Table V shows the traumatic mechanism responsible for shoulder and elbow dislocations in the 2 examined periods.
Table V.
Mechanisms of injury responsible for shoulder and elbow dislocations in the 2 examined periods
| Accidental fall | Sports trauma | High-energy (traffic accident) | Accident at work | Assault/beatings | |
|---|---|---|---|---|---|
| Shoulder dislocations | |||||
| No-COVID period | 5 | 3 | 1 | 1 | 0 |
| COVID period | 6 | 0 | 0 | 1 | 0 |
| Elbow dislocations | |||||
| No-COVID period | 1 | 1 | 0 | 0 | 0 |
| COVID period | 3 | 0 | 0 | 0 | 0 |
Discussion
The measures adopted to deal with the COVID-19 global pandemic have led to a profound change in our daily habits. In Europe, ours was the first country to adopt restrictive measures that prevented citizens from leaving their homes, except for proven health reasons and for carrying out functions essential to the community. This made our streets free of traffic, left our sports facilities unused, and kept the public parks closed. Therefore, we wanted to verify the impact that these restrictions have had on the traumatic shoulder and elbow pathology. We, therefore, compared the epidemiologic data relating to the first-aid services inherent in these 2 anatomic districts, and that occurred in March-April 2020 (COVID period), with those of the same period of the year before (no-COVID period).
Because in the last 2 weeks, our government has granted people in some job categories the opportunity to resume work, although with the necessary precautions aimed at preventing transmission of the virus, we have deemed it unnecessary to extend the study period.
The reduction in services (less 65%) provided in our trauma center during the pandemic period is the most striking data of our investigation. The most evident decrease was observed in the percentage concerning the number of contusions (low-energy injuries) compared with all the health services provided. In the no-COVID time, this percentage was 30%; in the COVID period, it fell to 19%.
We believe that 4 causes have led to a drastic reduction in health services: (1) The restrictions imposed to stem the virus spread have reduced the circumstances that usually predispose to trauma: traffic accidents, sports injuries, accidental falls on the road, and direct frontal blow. (2) The fear of a possible infection in the hospital discouraged those who underwent mild trauma from reporting to our emergency department. (3) The fear of incurring fines for violating government restrictions has further discouraged patients with mild trauma. (4) A lot of elderly patients have been isolated, and they could not count on family assistance for transportation to the hospital. Therefore, even on this occasion, patients with mild trauma hesitated to come to the trauma center.
Shoulder contusions drastically reduced in the COVID period (60 no-COVID period cases vs. 11 COVID period cases); however, their prevalence with respect to the total number of contusions remained almost unchanged (14.7% vs. 12.09%). This did not occur for elbow contusions, which decreased by 3.44%, compared with all contusions in the no-COVID time, at 1.09% in the COVID time. Once again, the decrease is due to the reduction or absence of high-energy trauma (traffic accidents and sports injuries).
Proximal humeral fractures are the seventh most frequent fractures in adults.21 The prevalence varies from 4%-10% of all fractures according to several studies performed in different countries and populations.2 , 4 , 9 , 14 , 18 , 21 In the 2 studied periods, humeral head fractures were 6.57% (no-COVID period) and 7.72% (COVID period) of all the fractures managed at our emergency department. The average age of these patients (72 years, no-COVID period; 70 years, COVID period) and the traumatic mechanism responsible for the fracture (accidental fall for all patients but 1) explain why the pandemic did not change the prevalence of this fracture. In fact, traumas, in both periods, occurred in the home environment and acted on an osteoporotic bone. The data seem to be in line with the results of Carbone et al,7 who observed that 72% of patients with humeral head fractures were markedly osteoporotic and that most of these patients were elderly women sustaining low-energy trauma.
Postacchini et al20 in an epidemiologic study observed that clavicle fractures represent 2.6% of all fractures and that traffic accidents, falls, and sports injury were the most common causes responsible for the fracture. During the COVID period, we have managed only 2 patients (0.96% of all fractures). The most plausible explanation for this obvious decrease in clavicle fractures is the drastic decline in traffic accidents and the absence of patients with fractures from sports injuries. Similar assumptions can be made to explain the absence of cases with a scapula/glenoid fracture during the COVID period. In fact, in the no-COVID period, we had treated 3 male patients aged between 40 and 50 years (no bony Bankart). Two of these patients had sustained the fracture following a traffic accident. These percentages are in line with the Ideberg et al10 series regarding the prevalence of glenoid fractures in the general population.
Radial head fractures are the most common fractures around the elbow.5 Kaas et al12 observed that the mean age of female patients (52.8 years) was significantly higher than that of male patients (40.5 years). Gender influences the mechanism of injury; female patients commonly sustain their fracture following a low-energy fall.8 Our patients with radial head fracture managed during the COVID period differ from those of the no-COVID period in size (decreased), gender prevalence (females only), average age (drastically increased), and traumatic mechanism (accidental falls only). Obviously, the absence of sports injuries and traffic accidents, which usually involve young males, explains the epidemiologic difference between the 2 examined periods. Similar considerations can be made for distal humerus fractures and proximal ulna fractures.
Patients included in the sprain/subluxation shoulder group are those who never had a true dislocation, but who probably had asymptomatic joint hyperlaxity. Of the 8 managed patients (6 belonged to the no-COVID period and 2 to the COVID period), 6 underwent sprain/subluxation following a low-energy trauma. The joint hyperlaxity makes the prevalence of this pathologic condition independent of the restrictive measures imposed to limit COVID-19 viral spread. The only patient we counted in the elbow sprain/subluxation group had no associated fractures, nor any clinical signs of joint instability. The diagnosis was formulated on the basis of what the patient said (he reported having a feeling of momentary post-traumatic elbow instability). No conclusions can be advanced from a single patient.
Shoulder instability is a common orthopedic condition, especially in a young active population.13 , 15 , 17 In our trauma center, primary dislocations and recurrences were 58% of all dislocations managed in the no-COVID period and 53% of those in the COVID period. Compared with the no-COVID period, the patient number decreased because there were no dislocations following sports injuries or traffic accidents.
In an epidemiologic study,11 178 elbow dislocations that occurred during the studied 12 years had been prevalently attributed to sports injury. We managed 2 elbow dislocations in the no-COVID period and 3 in the COVID period. Surprisingly, in all cases, the dislocations had occurred following an accidental fall, therefore regardless of the new lifestyle imposed by the quarantine.
Conclusions
During the COVID period, in our trauma center, we provided a reduced number of health services, compared with the same time the previous year, especially for those patients with low-energy trauma (contusions) and for those who underwent sports injuries and traffic accidents (clavicle, scapular and elbow fractures, and shoulder dislocations), which disappeared following government restrictions imposed to limit COVID-19 spread. However, during the COVID period, elderly subjects remain exposed to shoulder and elbow trauma due to low-energy (domestic) falls.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this study.
References
- 1.Allman F.L., Jr. Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–784. [PubMed] [Google Scholar]
- 2.Baron J.A., Karagas M., Barrett J., Kniffin W., Malenka D., Mayor M., et al Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Bastian J.D., Hertel R. Initial post-fracture humeral head ischemia does not predict development of necrosis. J Shoulder Elbow Surg. 2008;17:2–8. doi: 10.1016/j.jse.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 4.Buhr A.J., Cooke A.M. Fracture patterns. Lancet. 1959;1:531–536. doi: 10.1016/s0140-6736(59)92306-2. [DOI] [PubMed] [Google Scholar]
- 5.Burkhart K.J., Wegmann K., Müller L.P., Gohlke F.E. Fractures of the radial head. Hand Clin. 2015;31:533–546. doi: 10.1016/j.hcl.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Cabanela M.E., Morrey B.F. Fractures of the olecranon. In: Morrey B.F., editor. The elbow and its disorders. WB Saunders Co; Philadelphia, PA: 2000. [Google Scholar]
- 7.Carbone S., Mezzoprete R., Papalia M., Arceri V., Carbone A., Gumina S. Radiographic patterns of osteoporotic proximal humerus fractures. Eur J Radiol. 2018;100:43–48. doi: 10.1016/j.ejrad.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 8.Duckworth A.D., Clement N.D., Jenkins P.J., Aitken S.A., Court-Brown C.M., McQueen M.M. The epidemiology of radial head and neck fractures. J Hand Surg Am. 2012;37:112–119. doi: 10.1016/j.jhsa.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 9.Horak J., Nilsson B.E. Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res. 1975;112:250–253. [PubMed] [Google Scholar]
- 10.Ideberg R., Grevsten S., Larsson S. Epidemiology ofscapular fractures. Incidence and classification of 338 fractures. Acta Orthop Scand. 1995;66:395–397. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 11.Josefsson P.O., Nilsson B.E. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57:537–538. doi: 10.3109/17453678609014788. [DOI] [PubMed] [Google Scholar]
- 12.Kaas L., van Riet R.P., Vroemen J.P., Eygendaal D. The epidemiology of radial head fractures. J Shoulder Elbow Surg. 2010;19:520–523. doi: 10.1016/j.jse.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Kraeutler M.J., Currie D.W., Kerr Z.Y., Roos K.G., McCarty E.C., Comstock R.D. Epidemiology of shoulder dislocations in high school and collegiate athletics in the United States: 2004/2005 through 2013/2014. Sports Health. 2018;10:85–91. doi: 10.1177/1941738117709764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leyshon R.L. Closed treatment of fractures of the proximal humerus. Acta Orthop Scand. 1984;55:48–51. doi: 10.3109/17453678408992310. [DOI] [PubMed] [Google Scholar]
- 15.Magnuson J.A., Wolf B.R., Cronin K.J., Jacobs C.A., Ortiz S.F., Kuhn J.E., et al, MOON Shoulder Group Surgical outcomes in the frequency, etiology, direction, and severity (FEDS) classification system for shoulder instability. J Shoulder Elbow Surg. 2020;29:784–793. doi: 10.1016/j.jse.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mason M.L. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–132. doi: 10.1002/bjs.18004217203. [DOI] [PubMed] [Google Scholar]
- 17.Owens B.D., Agel J., Mountcastle S.B., Cameron K.L., Nelson B.J. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750–1754. doi: 10.1177/0363546509334591. [DOI] [PubMed] [Google Scholar]
- 18.Passaretti D., Candela V., Sessa P., Gumina S. Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg. 2017;26:2117–2124. doi: 10.1016/j.jse.2017.05.029. [DOI] [PubMed] [Google Scholar]
- 19.Pollock J.W., Faber K.J., Athwal G.S. Distal humerus fractures. Orthop Clin North Am. 2008;39:187–200. doi: 10.1016/j.ocl.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Postacchini F., Gumina S., De Santis P., Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 21.Roux A., Decroocq L., El Batti S., Bonnevialle N., Moineau G., Trojani C., et al Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98:715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 22.www.governo.it/it/coronavirus-misure-del-governo
- 23.www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports