The new coronavirus disease 2019 (COVID-19) originated in Wuhan, China, which has expeditiously spread across the global [1,2]. It is currently not clear as to how to effectively reduce mortality in severe patients. The majority of evidence confirms a significant association between cardiac injury and mortality with influenza viral infection [3,4]. A later study (being published) reported creatine kinase (CK), lactate dehydrogenase (LDH), or high-sensitivity C-reactive protein (hs-CRP) might be associated with poor outcomes for patients infected with 2019-nCOV. Given the limitations of the current data, whether cardiac biomarkers are independent risk factors for mortality is not reported in those infected with 2019-nCOV. The objective is to emphasize and confirm the key role of cardiac biomarkers for mortality in hospitalized non-survivors with NCIP in this study.
All patients with NCIP enrolled in this study were confirmed according to the WHO interim guidance between January 10 and February 20, 2020 [2]. This retrospective study was approved by the institutional ethics board of The Fifth Hospital of Wuhan, Wuhan, China. For each case of non-survivors, two subjects (n = 70) were matched with cases on age, sex and date of admission among discharged adult inpatients at early stage of the outbreak of COVID-19. Using the 105 patient medical records sampled, two independent operators (J. Guo and X.L. Yang) conducted the study and analyzed the medical data of patients.
The median age was 60 years, 57% male. The average age of deceased subjects (n = 35) was 64.07 years, with 57% male. Nearly 70% of the deceased had combined cardiovascular risk factors (14.3% diabetes and 51.4% hypertension), and 34.3% with other comorbidities. Compared with survivors, non-survivors had statistically higher levels of creatinine kinase-myocardial band (CK-MB), CK, lactate dehydrogenase, myoglobin, and Troponin I. For every increase of 112 in serum myoglobin levels, mortality increased by 3.15% in generalized estimation equation analysis. A receiver operating characteristic (ROC) curve analysis showed that the optimal myoglobin cut-off value was 306.5 μg/L (Youden's index = 0.426). The area under the ROC curve was 0.81 (95%CI: 0.68–0.95, p = 0.003). The sensitivity was 60.6% while specificity was 82% (Fig. 1 ). In the subgroup analyses, the values of cardiac biomarkers in elderly subjects (>65 years) with cardiovascular disease were significantly higher than ones in elderly without cardiovascular disease and young patients. In the early period, serum levels of myoglobin and CK-MB had a strong negative correlation with hs-CRP. In the later period, these biomarkers had a moderate positive correlation.
Fig. 1.
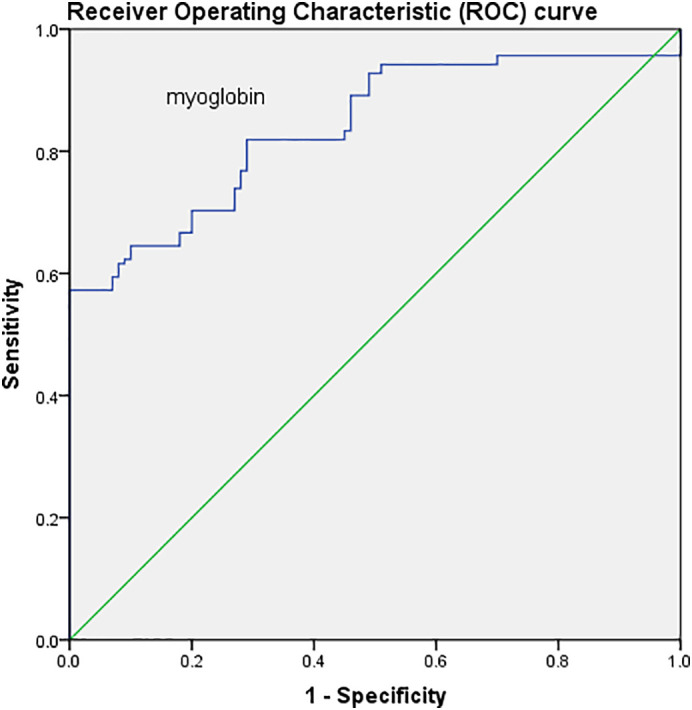
Prognostic predictive ability of myoglobin for hospitalized patients infected with 2019-novel coronavirus. The sensitivity and 1-specificity of myoglobin in prognostic prediction were estimated by receiver operating characteristic (ROC) curve.
To our knowledge, this is the first study to report the association between serum myoglobin and mortality in non-survivors with NCIP. Our results indicated that an elevated serum concentration of myoglobin (≥306.5 μg/L) was associated with an increased risk of hospitalization mortality in non-survivors, independent of elevation in CK-MB and Troponin I. We found that cut-off (≥306.5 μg/L) of myoglobin was high. In the context of 2019-nCOV, the deceased with NCIP usually had concurrent refractory hypoxia, hypotension and reduced renal perfusion, which may result in increased skeletal muscle and heart release of myoglobin [5]. Particularly, elderly (>65 years) non-survivor patients with cardiovascular diseases had more severe cardiac injury. Accordingly, we suggest that: firstly, in addition to the protection of the lungs first, the time window of therapeutic interventions about cardiac injury should be as early as possible for severe patients; secondly, inflammatory factor release should be blocked early, especially in elderly (>65 years) patients with cardiovascular diseases.
In conclusion, our study provides important documentation that in this single-center, an elevated serum concentration of myoglobin (≥306.5 μg/L) is associated with an increased risk of hospitalization mortality in non-survivor with NCIP, independent of elevation in CK-MB and Troponin I levels.
Declaration of competing interest
No conflict of interest exits in the submission of this manuscript.
Contributor Information
Meng-Jun Wu, Email: 2014982567@qq.com.
Wuquan Deng, Email: wuquandeng@gmail.com.
You-Sheng Yang, Email: 3400164739@qq.com.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lancet T. Emerging understandings of 2019-nCoV. Lancet. 2020;395:311. doi: 10.1016/S0140-6736(20)30186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao C., Wang Y., Gu X. Association between cardiac injury and mortality in hospitalized patients infected with avian influenza a (H7N9) virus. Crit Care Med. 2020 doi: 10.1097/CCM.0000000000004207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwong J.C., Schwartz K.L., Campitelli M.A. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 5.Spangenthal E., Ellis A. Cardiac and skeletal muscle myoglobin release after reperfusion of injured myocardium in dogs with systemic hypotension. Circulation. 1995;91:2635–2641. doi: 10.1161/01.cir.91.10.2635. [DOI] [PubMed] [Google Scholar]


