To the Editor:
During the coronavirus disease 2019 (COVID-19) pandemic, many patients have developed severe acute respiratory distress syndrome (ARDS), often requiring prone positioning. Despite “lung-protective” ventilation, the pulmonary vascular dysfunction associated with COVID-19-related ARDS1 can lead to right ventricular (RV) dilatation and dysfunction, both associated with poor outcomes. RV global longitudinal strain (GLS) assessed on transthoracic echocardiography was recently found to predict mortality more accurately than RV fractional area change (FAC) in patients with COVID-19.2 However, during prone positioning, the assessment of RV function using transthoracic echocardiography can be very challenging,3 and transesophageal echocardiography is often necessary. To date, RV FAC is still considered the best parameter for assessing RV systolic function on transesophageal echocardiography,4 but like RV GLS, it requires that the entire endocardium be clearly visible, which is sometimes difficult in the setting of acute cor pulmonale related to mechanical ventilation.
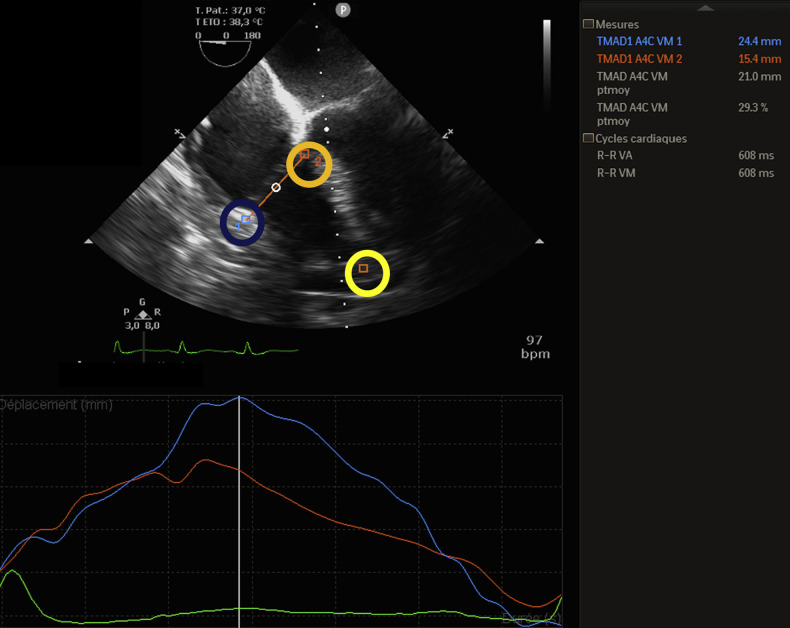
Tricuspid longitudinal annular displacement (TMAD) is an emerging bidimensional strain echocardiographic parameter, tracking tricuspid annular tissue motion toward the RV apex (Figure 1), allowing an objective quantitative assessment of RV systolic function.5 TMAD is also angle independent, but its main advantage compared with RV GLS is that it is unaffected by endocardial definition.
Figure 1.
TMAD on transesophageal echocardiography. In a midesophageal four-chamber view, the user-defined anatomic landmarks lateral point (blue circle) and septal point (orange circle) were placed at the bottom of the RV free wall and the bottom of the interventricular septum, and another point was placed at the apex (yellow circle). TMADlat, TMAD at the at the interventricular septum, and RV longitudinal shortening (%) are displayed.
Our objective was to assess the feasibility of TMAD and RV GLS and to evaluate their respective performance to diagnose RV dysfunction (defined as RV FAC < 35%) during prone positioning for severe ARDS related to COVID-19. TMAD measurements were performed in the apical four-chamber view, as recommended. Three points were placed, and the software (QLAB CMQ; Philips Medical Systems, Andover, MA) automatically tracked and calculated TMAD at the RV free wall (TMADlat) and at the interventricular septum. RV longitudinal shortening was also calculated.5 This was an ancillary study of a cohort of critically ill patients with COVID-19 (ClinicalTrials.gov identifier NCT04354558).
During the COVID-19 outbreak, 54 patients requiring mechanical ventilation were admitted to our intensive care unit for COVID-19-related ARDS (diagnosed by reverse transcriptase polymerase chain reaction), and 17 (32%) needed prone positioning for severe hypoxia. Transesophageal echocardiography was feasible in prone positioning for the 17 patients, with no related side effects. RV FAC, TMAD, and RV GLS measurements were attainable in all patients. Ten patients (83%) presented moderate acute cor pulmonale under mechanical ventilation, and seven patients (41%) had RV dysfunction (RV FAC < 35%). Median TMADlat was 23.5 mm (19.0 to 27.9 mm), median TMAD at the interventricular septum was 8.9 mm (7.0 to 11.0 mm), median RV longitudinal shortening was 28.1% (22.2% to 32.6%), median RV GLS was −24.7% (−22.6% to −28.5%), and median RV FAC was 43.6% (33.3% to 52.8%). TMADlat had the higher area under the curve (0.88 [0.73 to 1.00; P = .008] vs only 0.66 [0.38 to 0.92; P = .28] for RV GLS) for identifying RV systolic dysfunction, with a cutoff value of 18.5 mm (sensitivity, 0.8; specificity, 0.7). Intraobserver reproducibility of TMADlat was excellent (intraclass correlation coefficient = 0.98 [0.93 to 0.99]).
TMAD appears to be a feasible and reproducible strain parameter for assessing RV systolic function during prone positioning in ARDS related to COVID-19. Even if RV FAC and RV GLS were achievable in all patients, these measurements can be challenging in the setting of mechanical ventilation and prone positioning. Therefore, the use of a simple and effective angle-independent tool, such as TMAD, which is not affected by endocardial definition, may be of interest. Further larger studies investigating the prognostic impact of TMAD in patients with COVID-19 are mandatory.
Footnotes
Conflicts of interest: None.
References
- 1.Mahjoub Y., Rodenstein O.D., Jounieaux V. Severe Covid-19 disease: rather AVDS than ARDS? Crit Care. 2020 doi: 10.1186/s13054-020-02972-w. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Y., Li H., Zhu S., Xie Y., Wang B., He L. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. https://imaging.onlinejacc.org/content/early/2020/04/20/j.jcmg.2020.04.014 JACC Cardiovasc Imaging. Available at: Accessed June 2, 2020. [DOI] [PMC free article] [PubMed]
- 3.Giustiniano E., Bragato R.M., Padua E., Negri K., Cecconi M. Echocardiography during prone-position mechanical ventilation in COVID-19 patients: a proposal for a new approach. J Am Soc Echocardiogr. 2020;33 doi: 10.1016/j.echo.2020.04.027. 906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anavekar N.S., Gerson D., Skali H., Kwong R.Y., Kent Yucel E., Solomon S.D. Two-dimensional assessment of right ventricular function: an echocardiographic MRI correlative study. Echocardiography. 2007;24:452–456. doi: 10.1111/j.1540-8175.2007.00424.x. [DOI] [PubMed] [Google Scholar]
- 5.Li Y., Wang Y., Yang Y., Liu M., Meng X., Shi Y. Tricuspid annular displacement measured by 2-dimensional speckle tracking echocardiography for predicting right ventricular function in pulmonary hypertension: a new approach to evaluating right ventricle dysfunction. Medicine. 2018;97:e11710. doi: 10.1097/MD.0000000000011710. [DOI] [PMC free article] [PubMed] [Google Scholar]