Abstract
Using the integrative model (IM), we developed and tested messages to encourage adults to accompany their parent to a memory doctor for a cognitive evaluation. We conducted in-depth interviews (n=60) with African American and White adults with a parent age 65+ to identify key beliefs. Next, we carried out an IM-based telephone survey with a representative sample of the target population (n=541). Analyses revealed that attitudes varied depending on the gender of the parent. Resulting messages featuring mothers countered the fear of hearing bad news and the belief that mother does not want to be accompanied to the doctor’s office. Messages featuring fathers highlighted the belief that attending a doctor’s visit will provide father emotional support. We subsequently tested messages with focus group participants (n=48) and refined them. This study advances our understanding of opportunities to communicate about memory loss, including Alzheimer’s disease and dementia, in ways that encourage a behavioral action that will benefit older adults and their families.
Cognitive impairment among older adults is among the 21st century’s most significant public health challenges. Dementia affects approximately 8.8% of US adults age 65 and older (Langa et al., 2017). An estimated 5.7 million people in the US have Alzheimer’s disease, the most common cause of dementia, and over 16 million family members and friends provide unpaid care for them (Alzheimer’s Association, 2018a). In addition, other progressive neurodegenerative diseases such as Parkinson’s disease and Lewy Body Dementia, and non-neurodegenerative diseases such as vascular disease, sleep apnea, kidney failure, delirium and depression, as well as medications, can cause cognitive impairment (Plassman et al., 2008). Regardless of the cause, the challenges of cognitive impairment are serious. They include obstacles to living independently, such as in managing medications, using transportation, and making financial decisions, and an increased risk of physical disability (Auyeung et al., 2008; Centers for Disease Control and Prevention, 2013; Sabatino, 2011). It is no surprise, then, that Americans fear Alzheimer’s disease more than cancer (Alzheimer’s Association, 2014).
In 2005, the Centers for Disease Control and Prevention inaugurated the Healthy Brain Initiative and created a “National Public Health Road Map to Maintaining Cognitive Health” (Centers for Disease Control and Prevention & the Alzheimer’s Association, 2007). The second road map “The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships, 2013–2018” specifies actions; among them, Action Item E01 is to “Identify and promote culturally appropriate strategies designed to increase public awareness about dementia, including Alzheimer’s disease, to reduce conflicting messages, decrease stigma, and promote early diagnosis” (Alzheimer’s Association & Centers for Disease Control and Prevention, 2013). Doing so means recognizing the diversity of audiences (e.g., older adults, caregivers, policy makers, providers) and the disparities that exist in both risk and awareness. In 2011, President Obama signed the National Alzheimer’s Project Act into law, which launched the US National Alzheimer’s Plan, whose goals include enhancing public awareness and engagement and the prevention of Alzheimer’s disease by 2025 (US Department of Health and Human Services, 2012). Notably, the Plan uses the term “Alzheimer’s” to cover the many causes of cognitive impairment in older adults such as Parkinson’s and Lewy Body diseases.
Typically, the first people to observe changes in an older adult’s cognitive functioning are family members, such as a spouse or an adult child (Carpentier, Bernard, Grenier, & Guberman, 2010). Because people with cognitive problems typically either underestimate or underreport the presence and severity of these problems (Turró-Garriga et al., 2016), clinicians routinely rely on these observers to serve as “knowledgeable informants.” An informant provides history and context about an older adult’s cognitive changes. Knowledgeable informants are essential to making an accurate diagnosis and staging the severity of cognitive impairment (Briggs & O’Neill, 2016). These informants may also then serve as caregivers who enact the care plan.
Motivating adults who are observing declines in a loved one’s memory to take action is critical to assure that older adults experiencing cognitive decline receive diagnosis and care. An early diagnosis is critical to identifying the causes of cognitive impairment, determining what interventions are needed, and putting in place a care plan that will facilitate a better quality of life (Dubois, Padovani, Scheltens, Rossi, & Dell’Agnello, 2015). Despite these benefits of early diagnosis, less than 20% of older adults experiencing increased memory loss or confusion have discussed these symptoms with a health care provider (Centers for Disease Control and Prevention, 2013).
Unfortunately, while a close family member may be concerned about a relative who is experiencing memory loss, they may not know about the importance of accompanying their relative to the doctor. That is, they may not know about the need to serve as a knowledgeable informant. And, even if they do, accompanying their relative to the doctor visit is an unusual behavior, especially for persons who are not a spouse or partner and so do not have the regular and consistent contact and ease to accompany their relative to a doctor visit.
However, the need for non-spousal knowledgeable informants is clear. While more than half of community-dwelling older adults live with a spouse or partner (including same-sex partners), this proportion decreases with age, especially for women. Only 34% of women age 75 and older live with a spouse or partner, and overall 13.6 million older adults live alone (Administration on Aging, 2016). Studies of caregivers of older adults with cognitive impairment show that about one quarter or fewer of caregivers are spouses, while more than 50% are adult children or children in law (Friedman, Shih, Langa, & Hurd, 2015; National Alliance for Caregiving and the Alzheimer’s Association, 2017; Rabarison et al., 2018). Adult children, therefore, are an important demographic for ensuring early detection and diagnosis of cognitive decline in older adults.
Public health messaging can address the need for someone to accompany an older adult with cognitive problems to a clinical assessment. Mass media campaigns to promote healthy behaviors have become a major tool of public health practitioners. Campaigns have played a role in raising awareness about a host of public health issues, including healthy nutrition practices (Jordan, Piotrowski, Bleakley, & Mallya, 2012), drug abuse prevention (Fishbein et al., 2002), and cancer screening (Jorgensen, Gelb, Merritt, & Seeff, 2001). However, we know of no US based messages that encourage adult children with concerns about an aging parent’s memory to attend a visit with a health care provider and serve as a “knowledgeable informant.” Carefully crafted and culturally sensitive messages aimed at this audience may be an effective addition to efforts to promote healthy aging.
Theoretical Framework
Although there are many theories in the realm of health behavior change, there are “only a limited number of variables that must be considered in predicting and understanding any given behavior” (Fishbein & Cappella, 2006, p.S3). Fishbein used these variables, shown in Figure 1, to create an “integrative model of behavior change” (commonly abbreviated as “IM”) (Fishbein, 2000). This IM approach, also called the “reasoned action approach,” has been widely used in communication, public health, advertising, and psychology (Montano & Kasprzyk, 2015). In essence, it suggests that that one’s intention to perform a specific behavior (the “target behavior”) is the best predictor of behavior. Intention is a function of three key factors that must be understood as shaping intention, including one’s favorableness towards personally performing the behavior (attitudes), perceptions about what others think and do with regards to performing the behavior (norms), and beliefs about the ability to perform the behavior assuming that one wanted to do so (self-efficacy and control) (Fishbein & Azjen, 2010).
Figure 1.
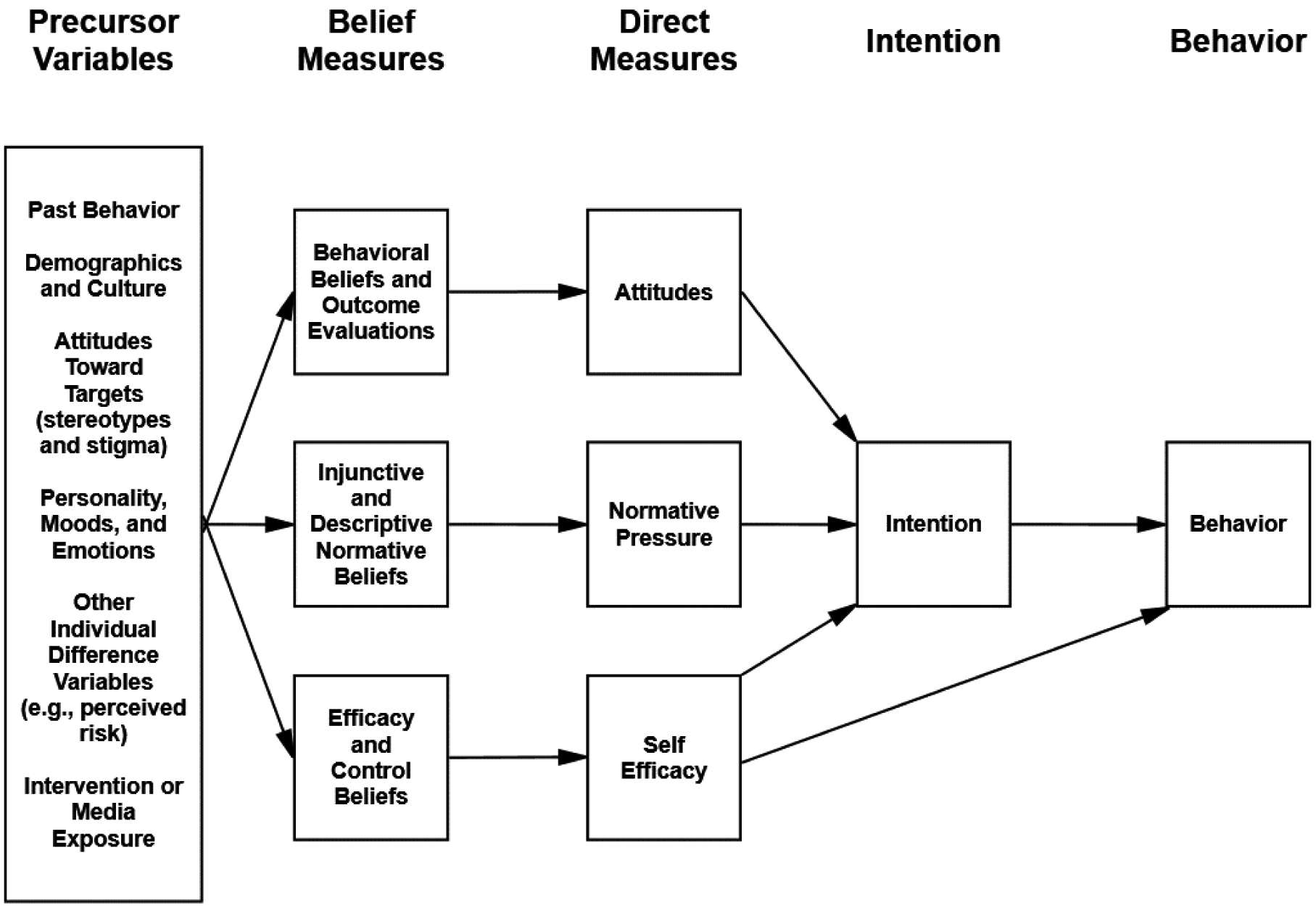
Integrative Model (IM) of Behavior
In this study, we used the IM to develop and test campaign messages targeted to encourage adult children to become knowledgeable informants for parents, stepparents, or parents-in-law with cognitive decline. This behavior reflects the key role that a knowledgeable informant has in the diagnosis and care of an older adult with cognitive impairments. We selected our target audiences based on the racial and ethnic makeup of our local community, the county of Philadelphia, which is 42.9% African American, and 35.3% non-Hispanic white (US Census Bureau, 2018).
Following the steps outlined by the IM, we used a qualitative research approach to identifying the salient beliefs of the target population, and then used these data to inform questionnaire development that incorporates the key concepts of the IM as illustrated in Figure 1. By understanding the beliefs associated with intention to act as a knowledgeable informant, we then designed prototypical messages that reflect these beliefs and tested them with members of the target population. This three phase approach has been successfully used in the design of quite diverse health communication campaigns (e.g., Jordan, Bleakley, Hennessy, & Vaala, 2015; Montano, Kasprzyk, Hamilton, Tshimanga, & Gorn, 2014).
Methods
Our project aimed to develop and test messages that encouraged adult children with concerns about an aging parent’s memory to visit a memory specialist for a cognitive assessment. For this study, we define a “memory specialist” as a physician or other health care professional with expertise in diagnosing, providing counsel, and treating an individual with the symptoms of memory loss, recognizing that the physician (MD or DO) or practice equivalent professions (NP) with skills in internal medicine, geriatrics, neurology, or psychiatry. In the interest of creating culturally relevant communication, we focused on one geographic region (Philadelphia) and the two predominant races that make up the population of this region (African American and non-Latino White). In the first phase, we conducted 60 open-ended interviews with members of the target population to elicit key beliefs about the behavior. We used the findings from the elicitation interviews for phase two: a closed ended, theory-based telephone survey conducted with a representative sample of adult children with an aging parent. Phase 3 involved the development, focus group testing, and refinement of messages designed for specific audiences that incorporated the salient beliefs associated with intention. All procedures and protocol were approved by the University of Pennsylvania Institutional Review Board. The research was carried out between June 2015 and July 2016.
Phase 1: Elicitation Interviews
An essential step in applying the IM to understanding health behaviors is conducting formative research to understand how members of the target population think about this behavior and whether and how these beliefs may differ along demographic or other dimensions. We therefore conducted interviews with members of the target population -- non-Latino White and African American adults with a parent, stepparent, or parent-in-law age 65 or older living in the Philadelphia metropolitan area. The interviews were designed to elicit key beliefs associated with accompanying a parent to a visit with a memory specialist for a cognitive evaluation. Participants were recruited through a variety of methods, including flyers disseminated in public places, postings on local Facebook groups and email lists, word of mouth, and an online research registry. Interviews were semi-structured and explored attitudes toward the behavior (e.g., good and bad things that would happen), perceived normative pressure (e.g., those who would approve or disapprove of the behavior), and self-efficacy and control (e.g., whether they feel the behavior is something they can do). Interviews lasted 15 – 20 minutes and were conducted either over the phone or in person by members of the research team. Participants received a gift card worth $20 as compensation for their time.
Interviews focused on one living parent, stepparent, or parent-in-law age 65 or older, who had not been already diagnosed with Alzheimer’s disease, dementia, or mild cognitive impairment, and who they had not already accompanied to an appointment for a memory evaluation. If more than one parent was eligible, participants were asked which parent they wished to focus on in the interview (target parent). Participants noted that they selected the target parent due either to the closeness of the relationship, their concerns about the parent’s memory, or that the target parent did not have others available to serve in this role. Participants were then asked if they had memory concerns about the target parent. If they had no concerns about the target parent’s memory, they were asked to imagine a scenario in which they did.
The interviews were designed to elicit beliefs about accompanying a parent to visit a memory doctor. To assess attitudes, for example, we asked “What do you see as the advantages (or good things that would happen) if you were to attend a doctor’s appointment with [name of target parent] to talk to a specialist about your concerns about his/her memory? Please list as many advantages as you can.” To assess norms, for example, we asked, “Who might approve or support you if you were to attend a doctor’s appointment to discuss your concerns about [target parent’s] memory?” We also asked about the kinds of things that would make it easy or difficult to attend a memory specialist with their parent. The interviews were transcribed verbatim and thematically coded by two to three coders to identify the most frequent beliefs to incorporate into the phase 2 IM survey.
Slightly more than half (52%) of the participants focused on the mother as the target parent and one-third (33%) focused on the father. The remaining discussed their stepfather, father-in-law, or mother-in-law. Of the 60 participants, 36 were White (60%) and 24 were African American (40%). Nearly three quarters (73%) were female. The average age of the participants was 43 (range 27 to 71) and the average age of the target parent was 73 (range 65–88). More than two thirds of participants (68%, n=41) reported having at least some concerns about the target parent’s memory and thinking. The interviews were conducted in between June and August 2015.
The elicitation interviews provided insight into key beliefs, referent others, barriers and facilitators that could then be used in a quantitative Integrative Model (IM) telephone survey. Beliefs were included in the IM survey if they were mentioned by more than 10% (n=6) of the interview participants. By way of example, the interviews elicited a number of “good” and “bad” things that participants perceived might happen if they visited a memory specialist with their parent.
On the high end, 43% of the interviewees mentioned that an advantage of attending a doctor’s appointment is the ability to get accurate information. A white female participant noted, “I could get perspective on how he is actually doing as opposed to how I perceive he is doing” and an African American male participant said, “They can tell me what I can do and how I can fix it or help fix it and it will help me out a lot, you know, because they’re the expert. You know, you don’t know everything.” Many (38%) worried that the parent would not want them to attend. One African American female participant, for instance, said that it would be hard to attend a visit with her mother due to “her attitude about me babysitting her on a visit to the doctor.” Others (37%) noted the opportunity to provide emotional support for their parent. A white female participant said, “I think [me being there] might make my mom more comfortable maybe…and less nervous.” On the low end, 18% mentioned that a disadvantage of attending would be that a parent might not feel comfortable sharing information in front of their adult child. A white female participant said that, if she attended with her mother, “She might be less willing to really open up about the severity… of her cognitive issues and her forgetfulness. I’m her kid and your parents always want to put a good face on things and protect you from stress.” See Table 1 for the most frequently mentioned beliefs.
Table 1.
Most frequently mentioned beliefs from the elicitation interviews (Phase 1)*
| Type of Belief | Belief | N (%) |
|---|---|---|
| Behavioral Beliefs | ||
| Advantage | Get accurate information | 26 (43%) |
| Advantage | Hear directly from physician | 25 (42%) |
| Advantage | Provide support to parent | 22 (37%) |
| Advantage | Face-to-face communication, personal connection | 21 (35%) |
| Advantage | Provide additional information to physician | 9 (15%) |
| Advantage | Ask questions directly to physician | 8 (13%) |
| Disadvantage | Parent is resistant | 21 (35%) |
| Disadvantage | Presence might inhibit parent sharing with physician | 11 (18%) |
| Normative Beliefs | ||
| Norm - Approve | Siblings | 32 (53%) |
| Norm - Approve | Spouse | 24 (40%) |
| Norm - Approve | Participant’s other parent/ Target parent’s spouse | 19 (32%) |
| Norm - Approve | Family (general) | 10 (17%) |
| Norm - Approve | Target parent | 10 (17%) |
| Norm - Disapprove | Target parent | 23 (38%) |
| Norm - Disapprove | Participant’s siblings | 9 (15%) |
| Self-Efficacy Beliefs | ||
| Barrier | Logistics | 41 (68%) |
| Barrier | Scheduling | 28 (47%) |
| Barrier | Distance | 19 (32%) |
| Barrier | Others’ attitudes | 12 (20%) |
| Facilitators | Logistics | 32 (53%) |
| Facilitators | Scheduling | 20 (33%) |
| Facilitators | Others’ attitudes | 9 (15%) |
| Facilitators | Getting information | 8 (13%) |
Beliefs were included if mentioned by >10% of sample.
Phase 2: Integrative Model Telephone Survey
A 15-minute telephone survey, conducted by the survey research firm Social Science Research Solutions (SSRS), was carried out with the target audience of Philadelphia area residents 18 years or older with a parent or parental figure at least 65 years old in December 2015 and January 2016. We worked with SSRS, a Philadelphia based survey research firm with expertise in conducting research within the Philadelphia region. We provided SSRS with the interview protocol and they pretested it with 12 participants. Team members listened to recordings of the interviews conducted by SSRS interviewers and subsequently refined the flow and wording of questions prior to the launch of the survey. SSRS provided updates throughout data collection, discussed challenges in recruiting certain segments of the population, and strategies for overcoming these challenges. The sample was designed to be representative of the greater Philadelphia area, but with an oversample of African American respondents to allow for comparison. To achieve an oversample of at least 200 African American respondents we used randomly generated phone numbers from landline and cell phone sampling frames, along with supplementary samples. Sample stratification was designed to efficiently complete interviews with a minimum of 200 African American eligible respondents. For this study, the Philadelphia area was defined as Philadelphia County and adjacent counties in Pennsylvania and New Jersey. The final combined response rate from all sources was 15%.
Sample
Respondent demographic characteristics and target parent characteristics are shown in Table 2. Slightly more than half of the participants were female (56%) and a majority were aged 45 to 64 (61.9%). More participants were White (51.7%) or African American (37.6%). More than half were married (55.8%) and nearly half (47.5%) were college educated. Slightly more than one-third of respondents reported a family history of Alzheimer’s disease. Nearly one third (30%) expressed concern about the target parent’s memory. The target parents referred to throughout the survey were also mostly female (67.1%), White (54.3%) or African American (37.9%) about evenly either married (44.9%) or divorced/separated/widowed (48.2%), and were the respondents’ mothers (50.7%). The majority (58%) said they never attend doctor’s visits with the target parent.
Table 2.
Summary statistics for the underlying behavioral, normative, and efficacy beliefs (Phase 2) (n=541)
| Behavioral (Attitudinal) Beliefs | % Likely |
|---|---|
| If I attended a doctor’s visit to a memory specialist with [TP], it would…. (1 Unlikely, 2 Neither, 3 Likely) | |
| it would make [TP] uncomfortable | 36.4% |
| it would give me a chance to ask the doctor questions | 88.7% |
| it would provide me with accurate information about [TP]’s health | 87.1% |
| it would provide emotional support to [TP] | 80.4% |
| It would inhibit [TP] from being completely honest with the doctor | 29.6% |
| it would negatively affect my relationship with [TP] | 9.1%% |
| Normative Beliefs | Mean (SD) |
| Injunctive: Do the people listed below think you should or should not attended a doctor’s visit to a memory specialist with [TP]? 1- Should not attend 7 Should attend | |
| Siblings (n=499) | 5.65 (2.0) |
| Spouse/partner (n=299) | 5.70 (1.93) |
| TP (n=535) | 4.99 (2.26) |
| TP’s spouse (n=238) | 5.34 (2.18) |
| Descriptive: About how many people in each of the groups listed below do you think have attended a doctor’s visit to a memory specialist with their parent? 1-None to 5-All | |
| Women with aging parents | 3.79 (.85) |
| Men with aging parents | 3.04 (1.00) |
| Female relatives | 3.75 (1.02) |
| Male relatives | 3.07 (1.15) |
| Efficacy/Control Beliefs | Mean (SD) |
| Please indicate how sure you are that you could attend a doctor’s visit with TP in the following circumstances: 1- Sure I could not 7 Sure I could not quit | |
| if the doctor’s office was far away | 5.88 (1.80) |
| if it was scheduled at an inconvenient time | 5.55 (1.93) |
| if [TP] didn’t want me there | 4.36 (2.39) |
| if I was afraid of hearing bad news | 6.29 (1.55) |
| if I knew there was no treatment for the problem | 5.88 (1.93) |
Measures
The IM measures used for this study were consistent with standard approaches used in previous studies as outlined by Fishbein & Azjen (2010). Both direct measures and underlying beliefs specific to going to a memory doctor with an aging parent were assessed. All measures were asked with regard to the specific “target parent” (TP) identified by the respondent, similar to the procedure for elicitation interviews. To select the target parent, participants were asked to focus on the parent who lived closest to them. If the closest living parent was not eligible, participants were then directed to focus on the next closest living parent, and so on.
Intention.
The intention measure asked “How likely is it that you will attend a doctor’s visit with [your TP] to discuss your concerns about (his/her/their) memory? Please answer on a scale of 1 to 5 with 1 being very unlikely and five being extremely likely” [M=3.40, SD=1.65].
Attitude.
Attitudes towards the behavior were measured using three semantic differential items on a scale from 1 to 7: bad/good, foolish/wise, and harmful/beneficial. For example, respondents were asked how they “would feel about attending a visit with a memory specialist with [your TP] to discuss concerns about (his/her) memory. Would this be bad or good? Please answer on a scale from 1 to 7, with one being bad and 7 being good.” The three items were averaged to create an overall attitude measure [M= 4.08 SD=.82; Alpha=0.74].
Perceived normative pressure.
Normative pressure was measured through injunctive and descriptive norms. On a 7-point scale, the injunctive normative item asked about whether the respondent thought “most people important to you think you should not (1) or should (7) attend the visit with [TP] to a memory specialist” [M=5.47 SD=2.07]. The descriptive norm asked whether “most people like you would or would not attend the visit” (1= would not attend; 7 = would attend; M=5.97 SD=1.71). Injunctive and descriptive norm means with values near 6 suggest that respondents feel high normative pressure. That is, respondents feel strongly that the people who are most important to them think they should attend and that people who are like them would themselves attend (although a SD of 2 indicates considerable variation).
Self-efficacy.
The self-efficacy measure asked the respondent to indicate agreement, on a 7-point scale from strongly disagree to strongly agree, with the statement: “If I really wanted to, I am certain that I could attend an appointment with a memory specialist with [my TP]” [M=6.14 SD=1.63]. The high mean for self-efficacy and the distribution of responses indicate that most respondents had strong beliefs about their confidence in being able to attend an appointment with their parent. For the analyses, we dichotomized self-efficacy based on the strong negative skew; strongly agree (69.6%) versus all other responses (30.4%).
Behavioral beliefs.
Respondents were asked how likely they thought it was that the following outcomes would happen if they attended a doctor’s visit to a memory doctor with their aging parent: (1) it would make [TP] uncomfortable, (2) it would provide accurate information about [TP]’s health, (3) it would provide emotional support to [TP]; (4) it would inhibit [TP] from being completely honest with the doctor; (5) it would give me a chance to ask the doctor questions, and (6) it would negatively affect my relationship with [TP]. Beliefs were measured on a 3-point scale, (1) Unlikely, (2) Neither likely nor unlikely, (3) Likely.
Normative beliefs.
Injunctive normative beliefs measured perceived normative pressure for attending or not the doctor the visit (1, Should not attend to 7, Should attend) for 4 specific types of people in their life: siblings, spouse/partner, the TP, and the TP’s spouse. Respondents were also given the option of “I don’t have this type of person in my life.” Descriptive normative belief items asked respondents their perception of whether the following referent groups have attended a memory doctor visit with their parent: women with aging parents, men with aging parents, female relatives, and male relatives. Response categories ranged from (1) None to (5) All.
Self-efficacy beliefs.
Respondents indicated on a 7-point scale how sure they could not (1) or could (7) attend the doctor’s visit in the following circumstances: 1. if the doctor’s office was far away, 2. if it was scheduled at an inconvenient time, 3. if [TP] didn’t want me there, 4. if I was afraid of hearing bad news, and 5. if I knew there was no treatment for the problem.
Descriptive statistics for the belief items are in Table 2.
Background variables.
Several variables were included as background variables in the IM model. They included gender of participant and parent, education, income, family history of Alzheimer’s disease, and concern about TP’s cognitive health.
Statistical Analysis
Descriptive statistics were generated for all variables. The IM analysis was conducted in two steps. The first step was to determine which constructs were most relevant to one’s intention to visit a memory specialist with an aging parent. To accomplish this aim, we used structural equation modeling to estimate the extent to which attitudes, normative pressure, and self-efficacy were associated with intention to visit the memory doctor. Age, gender, education level, income, family history of Alzheimer’s disease, and concern about TP’s cognitive health were treated as background variables. Next, moderating analyses were conducted by race (African American, White, and Hispanic/Other) and by participants’ relationship to the target parent. The paths from the background variables to attitudes, normative pressure, and efficacy were constrained to be equal across groups since we have no hypotheses about group differences or the effect of the background variables. Thus, only the paths from the mediating variables to intention could vary. Differences between the groups were calculated using Wald tests. We then analyzed the beliefs of the relevant constructs to determine which beliefs would be good candidates for inclusion in health messages (details below). All analyses were conducted in Stata 14.0.
Survey Results
Integrative Model Analysis
Table 3 shows the correlations among the model variables. The results of the path analysis are depicted in Figure 2. The model fit was good: χ2=11.95, p=.04; RMSEA=0.052; CFI=0.99; TLI=0.91. The model explains 20.4% of the variance in intention. Intention to visit a memory specialist with one’s target parent was driven by attitudes, injunctive norms (what they believe others want them to do), and self-efficacy. Descriptive norms (what they believe others like them are doing) were not associated with intention. Marital status (being married or other) was negatively associated with all four mediators. That is, the respondent being married was associated with less favorable attitudes about accompanying an aging parent to visit a memory doctor, lower perceived approval about going from important others, lower perceptions of peers performing the behavior, and lower beliefs about their ability to go to a visit. Income was also negatively associated with attitudes, and increased concern about TP’s memory was associated with lower self-efficacy. No other covariates were related to attitude, norms, or self-efficacy.
Table 3.
Correlation matrix of Integrative Model variables (Phase 2)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Intention | |||||||||
| 2. Attitude | .40 | ||||||||
| 3. Injunctive norms | .50 | .48 | |||||||
| 4. Descriptive norms | .32 | .35 | .57 | ||||||
| 5. Self-efficacy | .45 | .40 | .63 | .50 | |||||
| 6. College educated | −.10 | .02 | −.03 | .01 | −.08 | ||||
| 7. Married | .07 | −.11 | −.01 | −.00 | −.002 | −.41 | |||
| 8. Income | −.26 | −.20 | −.18 | −.15 | −.22 | .32 | −.32 | ||
| 9. Concern of TP’s memory | −.12 | −.02 | −.08 | −.11 | −.17 | −.02 | .22 | −.04 | |
| 10. Family history of Alzhiemer’s | −.07 | −.02 | −.04 | −.02 | .07 | .17 | −.07 | .22 | .02 |
Correlations are polychoric for dichotmous and ordinal variables and Pearson for continuous variables.
Figure 2.
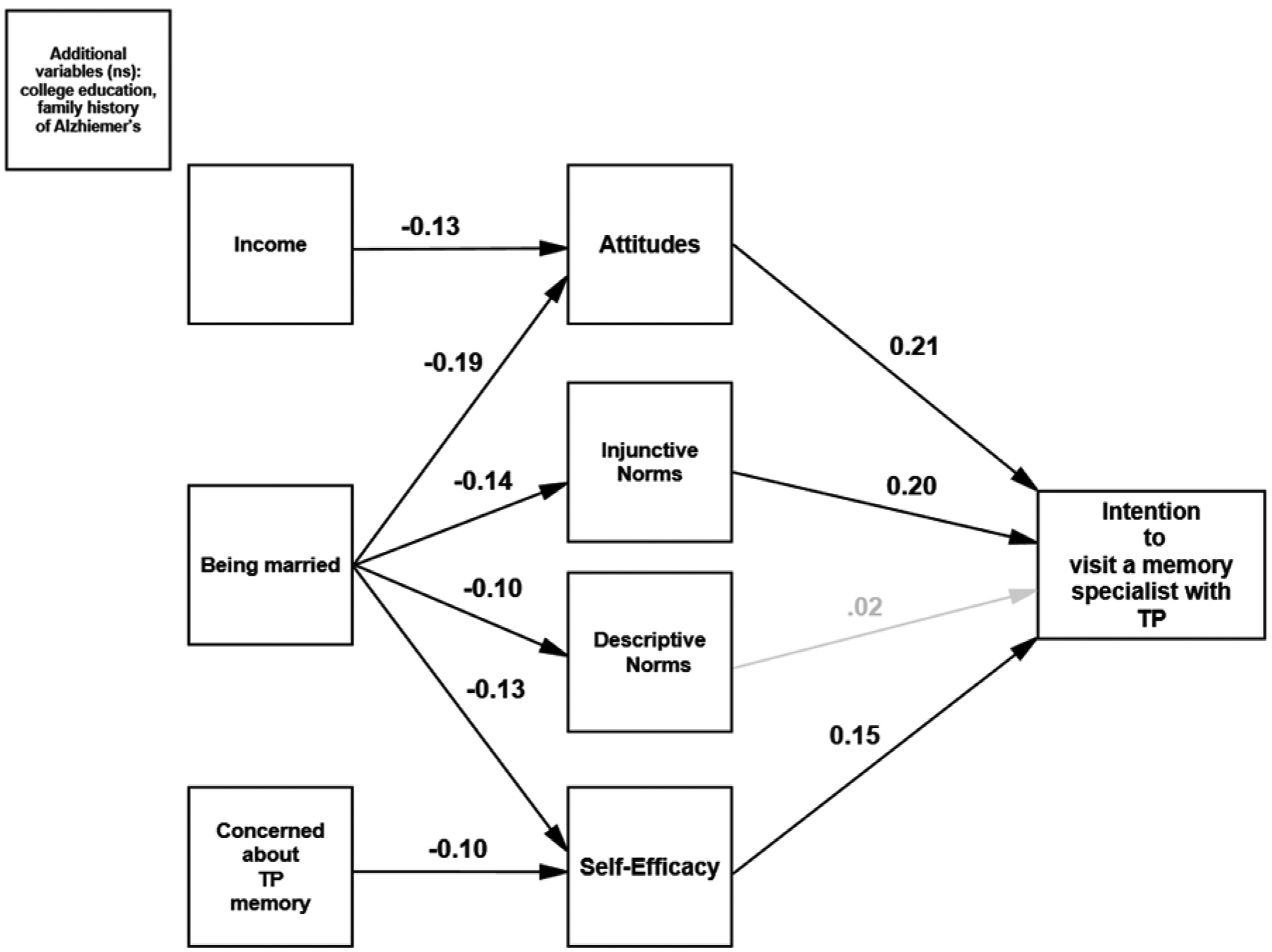
Predicting intention using the Integrative Model (Phase 2)
N=513; Standardized coefficients reported. Bold paths significant at least p<.05. Gray paths are not significant. Error terms of the mediating variables are correlated but not shown for clarity.
Moderation analyses
We conducted moderation analyses using two potential moderators: race (African American, White, Hispanic/other) and relationship to target parent (mother, father, other). As mentioned earlier, the path from the background variables to the mediators were constrained to be the same across groups. There were no differences by racial/ethnic group in the path coefficients of any of the mediating variables to intention. Model fit was excellent: χ2=56.05, p=.89; RMSEA=.00; CFI=1; TLI=1.04.
There were group differences, however, by relationship type. Again, model fit was good: χ2=89.85, p=.06; RMSEA=0.041; CFI=0.96; TLI=0.94. Table 4 presents the coefficients for each group, and differences between the groups are indicated by superscripts. Notably, respondents’ attitudes were significantly related to intention only when the parent was either one’s father or other (i.e., in-law/step-parent), and self-efficacy was only associated to intention when the parent was one’s mother. The difference in the path from self-efficacy to intention for mothers was significantly different only from the coefficient for fathers, but not others. This finding is notable because the literature on gender and caregiving shows that women, as opposed to men, are more likely to serve as caregivers, and also tend to provide more intensive and complex care; struggle to balance caregiving with other responsibilities; and suffer from poor physical and mental health as a result of caregiving (Erol, Brooker, & Peel, 2015). Therefore, we expected to find differences based on the gender of the interviewee (or potential caregiver), which we did not find, and we were surprised to instead observe differences based on the gender of the parent to whom the interviewee was referring.
Table 4.
Regression coefficients by relationship to target parent
| All | Mother | Father | Other | Wald test | |
|---|---|---|---|---|---|
| Mediators | |||||
| Attitude | 0.05a | 0.29b | 0.46b | χ2=15.68, p<.01 | |
| Injunctive norms | 0.24 | 0.15 | 0.06 | χ2=3.04, ns | |
| Descriptive norms | 0.03 | −0.01 | −0.07 | χ2=0.718, ns | |
| Self-efficacy | 0.25a | −0.03b | 0.12a,b | χ2=6.491, p<.05 | |
| Covariates | - | - | - | ||
| College education | 0.01 | - | - | - | |
| Income | −0.10 | - | - | - | |
| Married | −0.13 | - | - | - | |
| Concern about TP’s memory | −0.05 | - | - | - | |
| Family history of Alzheimer’s | 0.03 | - | - | - |
N=512. Standardized regression coefficients. Bolded coefficients significant at p<.01. Coefficients for covariates constrained to be equal across groups.
Beliefs analyses
Beliefs that are strongly held by those who intend to accompany a parent to a memory doctor and less so by non-intenders are those that may be most persuasive in media messages (Fishbein & Yzer, 2003). The relationships of the beliefs to intention were assessed to identify potentially modifiable beliefs. Descriptive beliefs were not analyzed because `general descriptive norms were not associated with intention. Respondents were divided into intenders (somewhat likely or likely; n=314) and non-intenders (very unlikely, somewhat unlikely, or neither; n=225). First, each belief was correlated with intention to attend a visit to a memory specialist (see Table 5). Because the importance of attitudes, norms, and efficacy varied by the relationship to the TP, we also present the belief-intention correlations within each relationship group: mothers, fathers, and others. Finally, the beliefs were dichotomized into those who answered affirmatively (i.e., “likely” for the behavioral beliefs; “should attend”, values 5–7, for injunctive beliefs; and “agree”, values 5–7, for efficacy beliefs). Differences between intenders and non-intenders were assessed using Chi-square statistics.
Table 5.
Correlations of beliefs with intention among “intenders” and “non-intenders” (Phase 2)
| Behavioral Beliefs | (Polychoric) Correlation with intention n=547 | (Polychoric) Correlation with intention [TP is mother] n=272 | (Polychoric) Correlation with intention [TP is father] n=137 | (Polychoric) Correlation with intention [TP is other] n=127 | % “Likely” for non- intenders | % “Likely” for intenders |
|---|---|---|---|---|---|---|
| It would make TP uncomfortable. | −.21* | −.10 | −.27* | −.20 | 44.2% | 30.6%* |
| It would provide me with accurate information about TP’s health. | .29* | .35* | .24 | .20 | 81.6% | 91.0%* |
| It would provide emotional support to TP. | .30* | .16 | .44* | .32* | 73.0% | 85.5%* |
| It would inhibit TP from being completely honest with the doctor. | −.08 | −.05 | −.05 | −.08 | 34.7% | 25.7%* |
| It would give me a chance to ask the doctor questions. | .35* | .29* | .35* | .38* | 81.8% | 93.6%* |
| It would negatively affect my relationship with TP. | −.13 | −.04 | −.23 | −.12 | 13.3% | 6.1%* |
| Normative beliefs (Injunctive) | ||||||
| Your siblings | .34* | .34* | .22* | .29* | 63.4% | 87.3%* |
| Your spouse/partner | .34* | .31* | .30* | .28* | 65.0% | 89.6%* |
| TP | .38* | .38* | .18* | .41* | 46.2% | 78.7%* |
| TP’s spouse | .34* | .37* | .23* | .30* | 54.3% | 83.3%* |
| Efficacy Beliefs | ||||||
| The doctor’s office was far away. | .25* | .24* | .11 | .27* | 73.7% | 87.7%* |
| It was scheduled at an inconvenient time. | .24* | .26* | .08 | .26* | 67.0% | 82.6%* |
| TP didn’t want me there. | .30* | .28* | .18* | .25* | 37.8%% | 65.0%* |
| I was afraid of hearing bad news. | .19* | .16* | .06 | .22* | 85.3% | 92.6%* |
| I knew there was no treatment for the problem. | .27* | .30* | .16 | .23* | 72.0%% | 88.5%* |
As shown in Table 5, there were several potential beliefs that were correlated with intention and that were different between intenders and non-intenders. We also considered the belief’s potential for messaging in terms of its appeal and resonance. Details on the beliefs chosen for the messages are described below.
Phase 3: Message Creation and Focus Group Testing
The results of the IM survey revealed the importance of recognizing distinct audience segments and developing messages that reflect the beliefs that are associated with intention. As noted above, a clear trend was observed in whether the target parent was the respondent’s mother or father (or mother-/father-like person in their life).
We therefore developed a series of 14 print messages that were specific to the gender of the target parent in order to leverage the distinct beliefs that were observed to drive intention. Working with a professional photographer/graphic designer, we created three sets of messages: 1) those featuring fathers or father-type figures, 2) those featuring mothers or mother-type figures, and 3) those featuring both. The IM survey suggested that messages featuring a father or father-type person should emphasize the belief that accompanying a parent to a memory specialist would provide emotional support. The IM survey data also pointed to efficacy beliefs negatively associated with intention to visit a memory specialist with one’s mother. In this case, the messages should counter-argue the fear of hearing bad news and should address the concern that she does not want her adult child to attend the visit with her. Thus, we believed that an effective message would be “You might think she doesn’t want you there, but she needs you there.” Finally, we assessed whether there is a belief that cuts across both parent genders. Our data suggested leveraging the normative belief that the family will support attending the visit together. See Table 6 for descriptions of all messages and the IM constructs they targeted.
Table 6.
Campaign messages and the IM constructs they reflect (Phase 3)
| Campaign Message Presented to Focus Groupsa | Parent featured | Final Campaign Messageb | IM constructs | |
|---|---|---|---|---|
| 1 | “Together make a visit; together make a plan. Visit a memory specialist with your mother. Get answers to all your questions.” | Mom | N/A | Behavioral beliefs: provide accurate info; chance to ask the doctor questions |
| 2 | “Together make a visit; together make a plan. You might not think your mother wants you to visit a memory specialist with her, but she needs you there.” | Mom | “Together make a visit; together make a plan. You might think your mother/loved one doesn’t want you to visit a memory doctor with her, but she needs you there.” | Behavioral beliefs: provide accurate info Efficacy: Parent didn’t want me to go |
| 3 | “Help the doctor help her. Going with your mother to a memory specialist means you get answers to all the questions she may forget.” | Mom | “There is something you can do. Going with your mother/loved one to a memory doctor means you get answers to all the questions she may forget.” | Behavioral beliefs: chance to ask the doctor questions Efficacy: no treatment available (final version only) |
| 4 | “Be there for him now, like he was there for you then. Is your father experiencing memory loss that disrupts his daily life? Visit a memory specialist with your father.” | Dad | “Is your father/loved one experiencing memory loss or confusion that disrupts his daily life? Be there for him now, like he was there for you then. Go with him to see a memory doctor.” | Behavioral beliefs: give emotional support |
| 5 | “He was there for you, now be there for him. Is your father experiencing memory loss that disrupts his daily life? Visit a memory specialist with your father.”c | Dad | “Is your father/loved one experiencing memory loss or confusion that disrupts his daily life? He was there for you, now be there for him. Go with him to see a memory doctor.” | Behavioral beliefs: give emotional support |
| 6 | “”Is your mom or dad having memory problems? There is something you can do. Visit a memory specialist together. Your family will thank you” | Both | N/A | Normative beliefs: family approval Efficacy: no treatment available |
The messages presented to African-American and White focus groups were identical in text. Images matched the race of the focus group participants.
Final messages included versions of both African-American and White individuals, and versions were made featuring daughters and sons for each message within each race, with the exception of message 4, in which only one African-American version was created. The gender of the child in the image was not obvious.
Two messages were presented with this text to each focus group: one featuring an image of a father with an adult daughter and one featuring an image of a father with an adult son.
Messages were identical except for the race of the featured characters, such that we had one set of messages for African Americans and one set of messages for Whites. We also varied the gender of the adult child pictured in the message to be either a son or daughter. Social cognitive theory argues that identification is key to persuasion, and we reasoned that audiences would more closely identify with the scenarios if they see themselves in the pictures (Kelder, 2015).
We tested messages in focus groups stratified by race. Recruitment of focus group participants occurred through a variety of methods, including flyers posted and distributed in public places, at events such as local health fairs, and through community partners such as local churches; postings on local Facebook groups, Craigslist, and email lists; word of mouth; and an online research registry. As with the previous two phases of the research, participants were from the Philadelphia metropolitan area, at least 18 years old, and had a living with parent or parent-in-law age 65 or older. They ranged in age from 23 to 73 with an average age of 46. A trained moderator, whose race was matched to the participants, led the groups. The focus group protocol allowed us to elicit individual and group feedback on the messages, the taglines, and the call to action (i.e., attend a visit with your parent to a doctor for their memory problems). Participants were able to examine messages in binders they could examine individually at their seat, and on enlarged poster size boards to discuss collectively as a group.
We held a total of 6 focus groups (3 African American, 3 White) with 48 participants. Focus groups lasted, on average, 75 minutes. Participants received a gift card worth $50 as compensation for their time and refreshments.
In our analysis of the focus group data, we were most interested in whether participants felt that this is a behavior that they are willing to perform, whether there are aspects of the messages that are successful or unsuccessful in persuading them, and whether the images and word choices are relevant to their lives. Our goal was to use these criteria to identify the most effective messages and, based on the composition of the group members (race and gender), revise the messages to make them as culturally relevant to the audiences as possible.
We found that most focus group participants expressed a willingness and ability to attend a visit with a memory specialist with their parent. For example, one white male participant noted, “As an adult, I wouldn’t expect anyone to go with me to the doctor, I’m a grown up, I go by myself. This is getting into a new territory, I think, for aging adults where it is important and can be very helpful to involve other family member. Yes, they’re an adult but it’s helpful to do it together as this is strongly emphasized here.” An African American female participant said, “It makes you stop and think, “Well, hey, maybe I do need to take mother or father, do [this] together with them.” Just so … it’s like, okay, we’re together. And cause it gives … make the parent think, “Okay, they’re interested and they care about me.”
Participants suggested changes in the type of pictures used. They preferred images that clearly featured an older parent and adult child. They wanted the images to look “real” and for the individuals featured to appear in a situation (i.e., in a doctor’s office, not a holiday or vacation) and with a demeanor (i.e., not overly happy) that fit the topic of memory loss and the message. They noted the relevance, or lack of relevance, to their community. One African American male participant said, in reference to the message featuring an African American family at a barbeque, “I like the picture because one, we need something to get our group, African Americans, to focus in on this issue. So often we see others in the pictures about memory problems. I think the picture is good for me because we’re trying to get more awareness in our community.”
Participants also discussed the placement and font of the text. They suggested that the most prominent text should make the focus on memory clear, for instance, leading with “Is your loved one experiencing memory loss or confusion…” rather than “Together make a visit. Together make a plan,” which seemed less specific. They wanted fewer words overall, text that was large and easy to read, and a “soft” font that did not come across as too bold or aggressive.
Most importantly, participants discussed how the wording of the messages should change and how the emphasis of the action should be adjusted. Several felt strongly that that we replace the term “visit” with a phrase that would establish a greater sense of partnership. The discussion led to a more acceptable term: “go with” a parent to visit a memory doctor. One white female participant stated, “I do like the “go with him,” more than “visit a memory specialist.” I think it’s more of a “support him in this stage” than a “you have to do this.” You know, visit a memory specialist. So I do like the “go with him,” wording part.”
The tagline “Help the doctor help her” did not resonate with participants. One white male participant noted, “Help the doctor help her is such a stock phrase. It’s like “help me help you.” It doesn’t really say anything to me. I just felt the whole thing didn’t really … like I said, my eyes just glazed over when I saw all the text. I didn’t want to pay attention.” Similarly, a white female participant stated, “I would take out “help the doctor help her,” I don’t even know what … that I know what that means.” Participants suggested instead that we use the tagline: “There is something you can do,” which participants responded positively to and which targeted the self-efficacy belief about no treatment or intervention being available. A white female participant said, “I want something to tell me that yeah, it’s worth it to maybe get people a little bit upset, a little bit wrangled, but get in and get some professional attention.”
In our messages we referred to a “memory specialist” as the health care provider who would do the cognitive assessment. Participants felt that this was confusing, and preferred the term “memory doctor.” One African American male participant noted, “You can go see a memory specialist, but what does the memory specialist do?” A white female participant stated, “It makes me think of more of something like speech therapist or something like that, where it’s not a neurologist it’s not necessarily an Alzheimer’s specialist doctor. It’s someone who sort of is more of a helping function.”
One key difference between African American and white focus group participants was over the terms “mother” and “father” used in the messaging. African American focus group participants felt that this would exclude important older adults in their lives with whom they have strong connections. “I’m a caregiver for an aunt and an uncle and a mother. That’s a lot of variables, so would that make me, like I’m thinking, would that [message] make me think of all of the other ones as well?” asked one African American female participant. Overall they felt that “loved one” would be a more suitable term. Several participants stated their agreement when one African American female participant suggested, “I think instead for her saying mother, just say family member, or parent, or loved one.” This observation did not emerge in focus groups with White participants.
Based on the focus group participants’ feedback, the four messages that were most appealing to the focus group participants were refined and redesigned to address their suggestions for improvement. See Figure 3 for a sample of the messages that were adjusted to reflect the focus group participants’ feedback.
Figure 3:
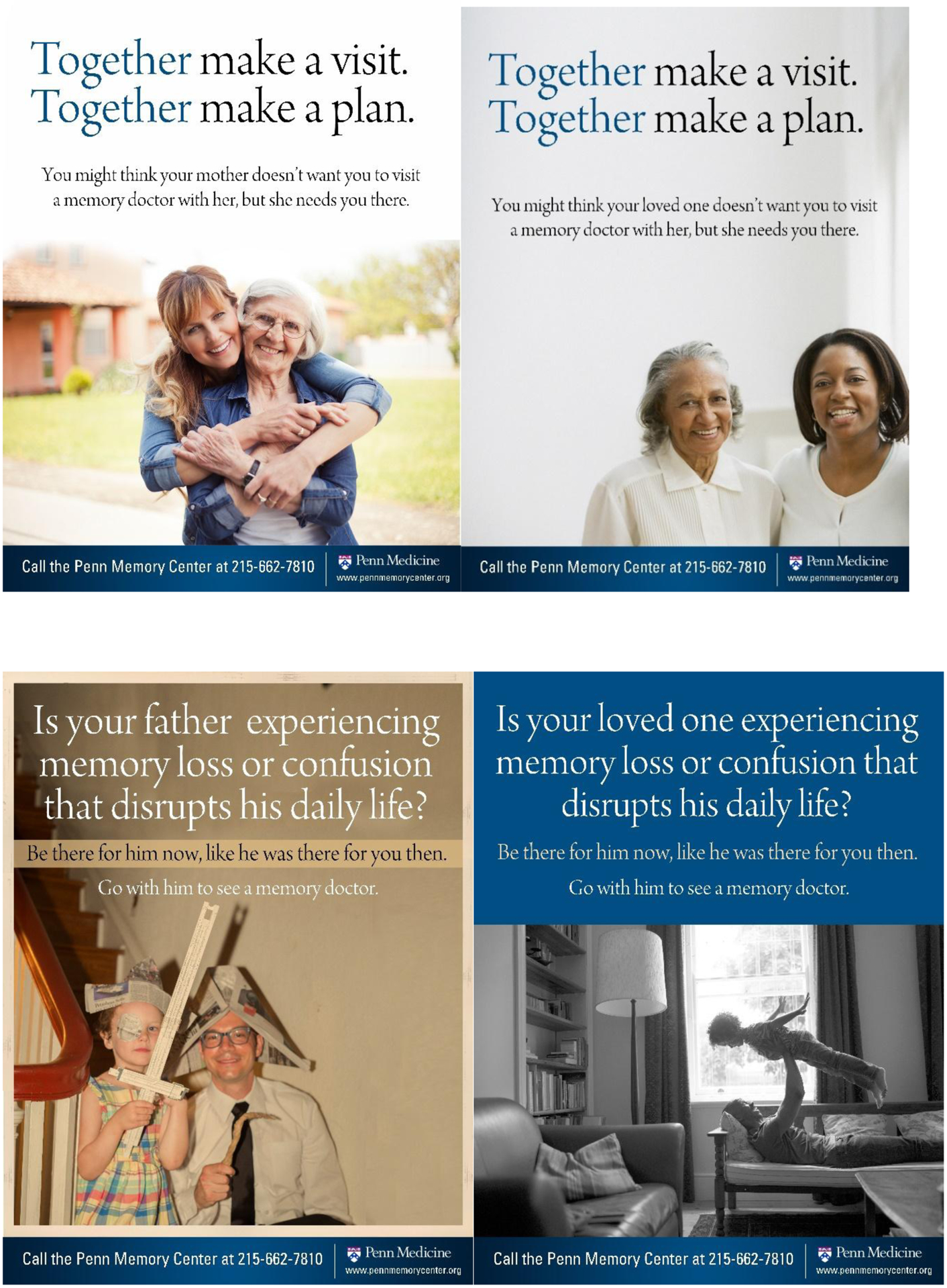
Example messages post focus group testing (Phase 3)
Conclusion
Early diagnosis of Alzheimer’s disease and other causes of cognitive impairment is associated with better outcomes. (Prince, Bryce, & Ferri, 2011; Dubois et al., 2015) Often relatives are the first to notice memory loss, and adult children may be well positioned to act as a knowledgeable informant during a cognitive evaluation, but may be reluctant to take on this novel behavior. Our goal with this research was to understand the beliefs associated with intention to accompany a parent to a visit with a memory specialist, and to determine culturally sensitive approaches to messaging around this behavior. Phase 1 elicitation interviews informed the design of the subsequent Phase 2 IM survey with a representative sample of African American and White Philadelphians with a parent, stepparent, or parent-in-law age 65 or older. Though we did not find differences related to race or gender of the participant in Phases 1 and 2, we did observe differences in the beliefs driving intention depending on whether the participant was imagining visiting a memory specialist with their mother or their father. Thus, in Phase 3 we developed messages specific to those beliefs, and tested them in focus groups.
We are limited in our ability to generalize the findings of this study beyond African American and White urban populations. Philadelphia may be unique in that it has specialists and centers qualified to conduct comprehensive evaluations. The messages we have designed assume that the setting in which a campaign like this would operate has the capacity to offer specialized evaluation, which may not be the case in every community. Moreover, while we followed a three-phase process of elicitation interviews, telephone survey, and focus group interviews, Phase 1 and Phase 3 relied on convenience samples and the representativeness of the respondents in the Phase 2 telephone survey may be limited due to the low response rate. The participants in the Phase 2 research were also more highly educated (47.5% college graduate or higher) and many were never married (26.7%), thus the ability to attend a visit with a memory specialist may be different for those who, for example, have young children to care for or who have demanding careers. We conducted this research with adults who may or may not have had pressing concerns about a parents’ memory. We asked those without concerns to think hypothetically, which may or may not always represent how they would think if faced with the reality of a parent’s failing memory. Ultimately, an important next step in this process will be to test these messages within a community setting to assess whether exposure to these messages leads to changes in beliefs and ultimately behavior.
Despite these limitations, the present study represents an effort to create messages around a behavior that is critically important to encourage as the US population ages. Our scan of the message environment revealed few current campaigns related to aging and memory loss with the exception of three widely disseminated ones, two from the Alzheimer’s Association (Alzheimer’s Association, 2009; Alzheimer’s Association, 2018b), and one from the Administration for Community Living (Administration for Community Living, 2015). While these campaigns and others in the media environment are important for generally raising awareness, their target audiences are older adults and the general public. Their action steps include “Schedule an appointment with your doctor,” “Stay on top of your game, and “Join the fight.” None are specifically geared to adult children and none have a specific action step that encourages an adult child to attend a specialist visit with a parent. At least one other English language non-US country (Australia) did address this behavior in its messaging, though their campaign is no longer active and we were unable to find published research on the development or effectiveness of the campaign or any of the awareness campaigns described above. It is our hope that this research effort offers a model for the creation of culturally sensitive messages and highlights an important behavior to target to improve the well-being of older adults.
In addition to the lack of relevant public health messaging campaigns, research has also not yet been done to identify the attitudes, self-efficacy beliefs, and norms that relate to an adult child’s intention to serve as a knowledgeable informant by accompanying their parent to a memory evaluation, or how these drivers might vary by characteristics such as race or gender. This study is a novel application of an established theory, the Integrative Model of Behavior Change, utilizing methodology that has been employed to develop messages encouraging a variety of different health behaviors.
Our findings show that, among urban African American and White adult children, messages encouraging them to serve as knowledgeable informants for their fathers should speak to their desire to provide emotional support to their father. In this same population, messages about serving in this role for their mothers should target the desire for accurate information and the chance to ask the doctor questions, while countering the beliefs that no treatment is available and that the mother does not want the adult child present. Additionally, we identified preferences about wording, types of images, font, and text placement that can increase the perceived relevance and believability of such messages.
Acknowledgement
This publication was funded by the Centers for Disease Control and Prevention under cooperative agreement U48DP005053. The views, findings and conclusions of this manuscript are those of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Contributor Information
Amy Jordan, School of Communication and Information, Rutgers, the State University of New Jersey, 4 Huntington Street, New Brunswick, NJ 08901, 848-932-8789.
Amy Bleakley, Annenberg School for Communication.
Kristin Harkins, Penn Memory Center, University of Pennsylvania.
Tigist Hailu, Children’s Hospital of Philadelphia, Department of Radiology.
Kyle Cassidy, Annenberg School for Communication, University of Pennsylvania.
Sara Hachey, School of Medicine, Temple University.
Jason Karlawish, School of Medicine, University of Pennsylvania.
References
- Administration for Community Living. (2015). What is Brain Health?. Retrieved August 1, 2017, from https://brainhealth.nia.nih.gov/about-the-campaign/
- Administration on Aging. (2016). A Profile of Older Americans: 2016. Retrieved August 1, 2017, from https://www.acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2016-Profile.pdf
- Alzheimer’s Association. (2009). 10 Early Signs and Symptoms of Alzheimer’s. Retrieved August 1, 2017, from http://www.alz.org/alzheimers_disease_10_signs_of_alzheimers.asp
- Alzheimer’s Association. (2014). 2014 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 10, e47–e92. doi: 10.1016/j.jalz.2014.02.001 [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2018a). 2018 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 14, 367–429. doi: 10.1016/j.jalz.2018.02.001 [DOI] [Google Scholar]
- Alzheimer’s Association. (2018b). The First Survivor. Retrieved August 23, 2018, from https://www.alz.org/about/awareness_campaigns/first_survivor
- Alzheimer’s Association & Centers for Disease Control and Prevention. (2013). The Healthy Brain Initiative: The Public Health Road Map for State and National Partnerships, 2013–2018. Chicago, IL: Alzheimer’s Association. [Google Scholar]
- Auyeung TW, Kwok T, Lee J, Leung PC, Leung J, & Woo J (2008). Functional decline in cognitive impairment: The relationship between physical and cognitive function. Neuroepidemiology, 31, 167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer JM, & Sousa-Poza A (2015). Impacts of informal caregiving on caregiver employment, health, and family. Journal of Population Ageing, 8, 113–145. doi: 10.1007/s12062-015-9116-0 [DOI] [Google Scholar]
- Briggs R, & O’Neill D (2016). The informant history: A neglected aspect of clinical education and practice. QJM: An International Journal of Medicine, 109, 301–302. doi: 10.1093/qjmed/hcv145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpentier N, Bernard P, Grenier A, & Guberman N (2010). Using the life course perspective to study the entry into the illness trajectory: The perspective of caregivers of people with Alzheimer’s disease. Social Science & Medicine, 70, 1501–1508. doi: 10.1016/j.socscimed.2009.12.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Self-reported increased confusion or memory loss and associated functional difficulties among adults aged >/= 60 years - 21 States, 2011. MMWR Morb Mortal Wkly Rep, 62, 347–350. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention & the Alzheimer’s Association. (2007). The Healthy Brain Initiative: A national public health road map to maintaining cognitive health. Chicago, IL: Alzheimer’s Association. [Google Scholar]
- Dubois B, Padovani A, Scheltens P, Rossi A, & Dell’Agnello G (2015). Timely diagnosis for Alzheimer’s disease: A literature review on benefits and challenges. Journal of Alzheimer’s disease, 49, 617–631. doi: 10.3233/JAD-150692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erol R, Brooker D, & Peel E (2015). Women and Dementia: A global research review. Retrieved August 1, 2018, from https://www.alz.co.uk/sites/default/files/pdfs/Women-and-Dementia.pdf
- Fishbein M (2000). The role of theory in HIV prevention. AIDS Care, 12, 273–278. doi: 10.1080/09540120050042918 [DOI] [PubMed] [Google Scholar]
- Fishbein M, & Azjen I (2010). Predicting and changing behavior: A reasoned action approach. New York, NY: Psychology Press, Taylor & Francis Group. [Google Scholar]
- Fishbein M, & Cappella J (2006). The role of theory in developing effective health communications. Journal of Communication, 56, S1–S17. [Google Scholar]
- Fishbein M, Cappella J, Hornik R, Sayeed S, Yzer M, & Ahern RK (2002). The role of theory in developing effective antidrug public service announcements In Crano WD & Burgoon M (Eds.), Mass Media and Drug Prevention: Classic and Contemporary Theories and Research. Mahwah, N.J.: Erlbaum. [Google Scholar]
- Fishbein M, & Yzer MC (2003). Using theory to design effective health behavior interventions. Communication Theory, 13, 164–183. [Google Scholar]
- Fisher GG, Franks MM, Plassman BL, Brown SL, Potter GG, Llewellyn D, … Langa KM (2011). Caring for individuals with dementia and cognitive impairment, not dementia: Findings from the aging, demographics, and memory study. Journal of the American Geriatric Society, 59, 488–494. doi: 10.1111/j.1532-5415.2010.03304.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Shih RA, Langa KM, & Hurd MD (2015). U.S. prevalence and predictors of informal caregiving for dementia. Health Affairs, 34, 1637–1641. doi: 10.1377/hlthaff.2015.0510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A, Bleakley A, Hennessy M, & Vaala S (2015). Sugar-sweetened beverage-related public service advertisements and their influence on parents. American Behavioral Scientist, 59, 1847–1865. [Google Scholar]
- Jordan A, Piotrowski JT, Bleakley A, & Mallya G (2012). Developing media interventions to reduce household sugar-sweetened beverage consumption. Annals of the American Academy of Political and Social Science, 640, 118–135. [Google Scholar]
- Jorgensen CM, Gelb CA, Merritt TL, & Seeff LC (2001). Observations from the CDC: CDC’s screen for life: A national colorectal cancer action campaign. Journal of Women’s Health & Gender Based Medicine, 10, 417–422. [DOI] [PubMed] [Google Scholar]
- Kelder S, Hoelscher D, Perry CL (2015). How individuals, environments, and health behaviors interact: Social cognitive theory In Glanz K, Rimer B & Vishwanath V (Eds.), Health behavior: Theory, research, and practice (pp. 159–181). San Francisco, CA: Jossey Bass. [Google Scholar]
- Langa KM, Larson EB, Crimmins EM, Faul JD, Levine DA, Kabeto MU, & Weir DR (2017). A comparison of the prevalence of dementia in the United States in 2000 and 2012. JAMA Internal Medicine, 177, 51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F, Wharton W, Dowling NM, Ries ML, Johnson SC, Carlsson CM, … Gleason CE (2010). Awareness of memory abilities in community-dwelling older adults with suspected dementia and mild cognitive impairment. Dementia and Geriatric Cognitive Disorders, 30, 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr., Kawas CH, … Phelps CH (2011). The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & Dementia, 7, 263–269. doi: 10.1016/j.jalz.2011.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montano DE, & Kasprzyk D (2015). Theory of reasoned action, theory of planned behavior, and the integrated behavioral model In Glanz K, Rimer B & Viswanath K (Eds.), Health behavior: Theory, research, and practice (pp. 95–124). San Francisco, CA: Jossey Bass. [Google Scholar]
- Montano DE, Kasprzyk D, Hamilton DT, Tshimanga M, & Gorn G (2014). Evidence-based identification of key beliefs explaining adult male circumcision motivation in Zimbabwe: Targets for behavior change messaging. AIDS and Behavior, 18, 885–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving and the Alzheimer’s Association. (2017). Dementia Caregiving in the U.S. 2015 Retrieved August 1, 2018, from https://www.caregiving.org/wp-content/uploads/2014/01/Dementia-Caregiving-in-the-US_February-2017.pdf
- Navaie-Waliser M, Spriggs A, & Feldman PH (2002). Informal caregiving: Differential experiences by gender. Medical Care, 40, 1249–1259. [DOI] [PubMed] [Google Scholar]
- Plassman BL, Langa KM, Fisher GG, Heeringo SG, Weir DR, Ofstedal MB, … Wallace RB (2008). Prevalence of cognitive impairment without dementia in the United States. Annals of Internal Medicine, 148, 427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Bryce R, & Ferri C (2011). World Alzheimer Report 2011: The Benefits of Early Diagnosis and Intervention. London, U.K: Alzheimer’s Disease International. [Google Scholar]
- Rabarison KM, Bouldin ED, Bish CL, McGuire LC, Taylor CA, & Greenlund KJ (2018). The economic value of informal caregiving for persons with dementia: Results from 38 states, the District of Columbia, and Puerto Rico, 2015 and 2016 BRFSS. American Journal of Public Health, e1–e8. doi: 10.2105/ajph.2018.304573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatino CP (2011). Damage prevention and control for financial incapacity. Journal of the American Medical Association, 305, 707–708. [DOI] [PubMed] [Google Scholar]
- Sauvaget C, Yamada M, Fujiwara S, Sasaki H, & Mimori Y (2002). Dementia as a predictor of functional disability: A four-year follow-up study. Gerontology, 48, 226–233. [DOI] [PubMed] [Google Scholar]
- Turró-Garriga O, Garre-Olmo J, Calvó-Perxas L, Reñé-Ramírez R, Gascón-Bayarri J, Conde-Sala JL, & Dourado M (2016). Course and determinants of anosognosia in Alzheimer’s disease: A 12-month follow-up. Journal of Alzheimer’s disease, 51, 357–366. doi: 10.3233/jad-150706 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. ACS Demographic and Housing Estimates, 2012–2016 American Community Survey 5-Year Estimates, Table DP05. Retrieved August 1, 2018, from http://factfinder.census.gov
- U.S. Department of Health and Human Services. (2012). National Plan to Address Alzheimer’s Disease. Retrieved January 8, 2016, from https://aspe.hhs.gov/national-plans-address-alzheimers-disease


