Abstract
AIM
To design and evaluate psychometrics of adolescent self-report and parent proxy-report questionnaires assessing readiness for independent self-care in adolescents with type 1 diabetes (RISQ-T and RISQ-P).
METHODS
178 adolescents with type 1 diabetes (ages 13–17 years) and their parents completed the 20-item RISQ-T and 15-item RISQ-P, along with diabetes-specific measures of parent involvement, self-efficacy, burden, and treatment adherence. Evaluation of psychometric properties included calculation of internal consistency, adolescent and parent agreement, test-retest reliability, concurrent and predictive validity.
RESULTS
The RISQ-T (α=.78) and RISQ-P (α=.77) demonstrated sound internal consistency. Higher RISQ-T and RISQ-P scores (indicating more adolescent readiness for independent self-care) showed significant associations with less parent involvement in diabetes care (adolescent r=−.34; parent r=−.47; p<.0001), greater adolescent diabetes self-efficacy (adolescent r=.32; parent r=.54; p<.0001), less parent-endorsed diabetes-related burden (parent r=−.30; p<.0001), and greater treatment adherence (adolescent r=.26, p=.0004; parent r=.31, p<.0001). Adolescent and parent scores were significantly correlated (r=.35; p<.0001); test-retest reliability was reasonable (ICC RISQ-T r=.66; RISQ-P r=.71). Higher baseline RISQ-P scores significantly predicted reduced family involvement after six months (β=−.14, p=.02).
CONCLUSIONS
RISQ-T and RISQ-P demonstrate sound psychometric properties. Surveys may help inform diabetes teams of the level of support needed to facilitate shift to independent self-management.
Keywords: type 1 diabetes, adolescents, readiness, transition, self-care
1. Introduction
Adolescence is a critical developmental stage for adolescents with type 1 diabetes. Declining treatment adherence and deteriorating glycemic control, resulting in short- and long-term health complications, are common in adolescence [1]. Only 17% of youth achieve the American Diabetes Association (ADA) HbA1c goal of <7.5% (58 mmol/mol) [2]. Regardless of glycemic control, adolescents’ maturity and neurocognitive functioning naturally advance [3, 4] and they begin to seek and assume increasing independence in multiple areas of life [5] during this developmental period.
These normative changes take place alongside physical and psychosocial developmental challenges and culminate in the planned, purposeful transfer of young adults from child-centered to adult-oriented health care systems [6]. Multiple expert consensus statements highlight the importance of timely transitions from pediatric to adult care environments [7, 8]. Transition research tends to focus on readiness for transition in adolescents, as well as biomedical (e.g., glycemic control), behavioral (e.g., self-management), and psychosocial (e.g., quality of life) outcomes using a variety of measures [9, 10]. Existing generic (e.g., Transition Readiness Assessment Questionnaire [TRAQ]) and diabetes-specific (Readiness for Emerging Adults with Diabetes Diagnosed in Youth [READDY]) self-report measures are available to assess transition readiness in adolescents and young adults [10–12].
The transfer from pediatric to adult health care is preceded by the important shift from parent-driven care to adolescent-driven self-care [13–15]. Prior to the actual transfer to adult health care delivery, adolescents must acquire greater knowledge and skills for diabetes self-care, and the ability to perform diabetes self-care tasks independently. Adolescents must gain the understanding and ability to effectively perform the behavioral and cognitive tasks necessary to assume their own diabetes care responsibilities in daily life. For example, adolescents must learn how to independently determine insulin dose based on diet, exercise, and intercurrent illness. Acquisition of these skills needs to be aligned with the person’s goals and needs [16], and with awareness of the importance of self-care for health. Previous studies have shown that perceived importance is predictive of health behaviors such as healthy eating [17] and medication adherence [18].
The shift from parent-driven care to adolescent-driven self-care [13–15] is a precursor to the transfer from pediatric to adult health care, and can be considered one of the first of many developmental shifts that a person with type 1 diabetes will make throughout their lifetime. We can theorize that if this shift is managed well, it may have positive implications for future care transitions. However, there is need for a dedicated, brief measure to assess readiness for independent diabetes self-care targeting adolescents and their parents. To that end, we introduce the psychometric properties of the newly developed Readiness for Independent Self-Care Questionnaire Adolescent (RISQ-T) and Parent (RISQ-P) versions, assessing adolescent and parent perceptions of readiness for independent self-care by adolescents with type 1 diabetes.
2. Subjects, Materials and Methods
2.1. Participants and Procedure
Adolescents were recruited using the following eligibility criteria: 13 to 17 years old, type 1 diabetes for at least six months, daily insulin dose ≥0.5 U/kg/day, and fluency in English. Exclusion criteria included significant developmental or cognitive disorder, diagnosed major psychiatric disorder, or other severe psychosocial, medical, or family issues assessed by the health care team. After study protocol approval by the Institutional Review Board, 178 adolescents and their parents participated, and provided written informed assent and consent.
2.2. Data Collection and Measures
Data were collected through joint adolescent-parent interview, medical record review, and glucose meter/pump downloads. HbA1c assay was performed as part of routine clinical care (Roche Cobas Integra, reference range 4.0–6.0%). Parents provided demographic data. Adolescents and parents completed the following surveys on tablet computers using REDCap software [22].
2.2.1. Readiness for Independent Self-Care
The development of the RISQ-T and RISQ-P was driven by research in the domains of adolescent development, type 1 diabetes self-care needs, and transition readiness. A multidisciplinary team of diabetes healthcare professionals developed the measure, informed by the TRAQ [23], to create diabetes-specific items for the RISQ. Three domains are assessed: 1) Knowledge (8 items reflecting knowledge required to engage in effective self-care, e.g., “I know how to determine my insulin dose based on my blood sugar”), 2) Behavior (15 items reflecting frequency of independent self-management behaviors, e.g., “I adjust my insulin and/or food intake for exercise”), and 3) Perceived Importance (5 items reflecting adolescents’ perceptions of the importance of these behaviors, e.g., “To take care of my diabetes on my own, it is important for me to know/learn how to interpret blood sugar information”). Cognitive debriefing for the questionnaire was conducted with a small number of patients.
In the RISQ-T, adolescents report their own perceptions of readiness for independent diabetes self-care. In the parallel RISQ-P, parents report on their perceptions of adolescents’ readiness for independent self-care using only the Knowledge and Behavior scales; the Perceived Importance scale is omitted, as this scale targets adolescents’ perspectives specifically. Response options for the Knowledge domain are “No”/“Yes” (scored 0/4). Response options for the Behavior and Perceived Importance domains are on 5 point Likert scales: 0=“Never” to 4=“Always”, and 0=“Not important” to 4=“Very important”, respectively. Responses are meaned and scaled, resulting in total scores ranging from 0–100, with higher scores indicating greater perceived readiness. Questionnaire completion takes approximately 5 minutes.
2.2.2. Parent involvement in diabetes management
The previously validated Diabetes Family Responsibility Questionnaire (DFRQ) [24] assesses youth and parent perceptions of how diabetes management responsibilities are shared. In both versions of the measure, 17 management tasks are scored on a 3-point Likert scale (1=“adolescent taking or initiating responsibility for this task almost all the time” to 3=“parent taking or initiating responsibility for this task almost all of the time”). Total scores are standardized from 0 (complete adolescent responsibility) to 100 (complete parent responsibility).
2.2.3. Diabetes-specific self-efficacy
The previously validated Diabetes Management Self-Efficacy Survey (DMSE) [25] assesses confidence in youth’s ability to manage diabetes by both youth and parent-proxy report. Each version of the DMSE contains 16 items with response options on a 5-point Likert scale (0=“Disagree a lot” to 4=“Agree a lot”). Total scores range from 0–100; higher scores indicate greater adolescent self-efficacy.
2.2.4. Diabetes-related burden
The previously validated Problem Areas in Diabetes - Pediatric (PAID-Peds) [26] and Parent (PAID-PR) versions [27] assess perceived diabetes-related burden and emotional functioning in youth and parents, respectively. The PAID-Peds and PAID-PR consist of 20 and 18 items, respectively, with response options on a 5-point Likert scale (0=“agree” to 4=“disagree”). Total scores range from 0–100; higher total scores indicate greater perceived burden of diabetes.
2.2.5. Treatment adherence
The previously validated Diabetes Management Questionnaire (DMQ) [28] assesses adherence to diabetes management tasks over the last month (insulin management, physical activity, diet, and glucose monitoring) by both youth and parent report. Each version of the measure consists of 20 items with response options on a 5-point Likert scale (0=“Almost never” to 4=“Almost always”). Total scores range from 0–100, with higher scores indicating greater adherence.
2.3. Statistical Analyses
Data were analyzed using SAS v.9.4 (SAS Institute, Cary, NC). Descriptive statistics are presented as M±SD for continuous data and as percentages for categorical data. To examine the psychometric properties of the RISQ-T and RISQ-P, bivariate correlations and paired t-tests were performed. Cronbach’s α and item-to-total correlations (using standardized values) were calculated to assess internal consistency. Concurrent validity was assessed through associations with adolescent and parent scores on the Diabetes Family Responsibility Questionnaire (DFRQ), Diabetes Management Self-Efficacy Questionnaire (DMSE), Problem Areas in Diabetes–Pediatric (PAID-Peds) and –Parent (PAID-PR) surveys, and the Diabetes Management Questionnaire (DMQ). Adolescents and parents also completed the RISQ-T and RISQ-P again after 6 months, and test-retest reliability was assessed by calculating the intraclass coefficient (ICC) estimates. To assess predictive validity, multivariate regression models controlling for age, sex, and baseline HbA1c calculated associations between baseline RISQ-T and RISQ-P with changes in adolescent- and parent-reported family involvement, adolescent self-management, and adolescent glycemic control at 6 months.
3. Results
3.1. Participants’ characteristics
Table 1 presents demographic and diabetes-related characteristics. About half of adolescents (48%) were female and 88% were non-Hispanic white. Participants had a mean age of 14.9±1.3 years and diabetes duration of 7.4±3.7 years. Mean frequency of blood glucose monitoring was 4.9±2.0 times daily, the majority of adolescents (67%) received insulin pump therapy, and 15% of adolescents used continuous glucose monitoring (CGM). Mean HbA1c of the sample was 8.5±1.0% (69±11 mmol/mol).
Table 1 –
Participant Characteristics (N=178)
| Mean ± SD or % | |
|---|---|
| Age (years) | 14.9±1.3 |
| Sex (% female) | 48 |
| Race/ethnicity (% non-Hispanic white) | 88 |
| Parent education (% with college degree) | 72 |
| Regimen (% pump treated) | 67 |
| CGM use (%) | 15 |
| Family structure (% 2 parent family) | 87 |
| Type 1 diabetes duration (years) | 7.4±3.7 |
| Blood glucose monitoring frequency (times/day) | 4.9±2.0 |
| HbA1c (mmol/mol; %) | 69±11 mmol/mol; 8.5±1.0 |
3.2. RISQ-T and RISQ-P scores
Individual items on the RISQ-T (originally 28 items) and RISQ-P (originally 23 items) were first assessed for variability and item-to-total correlations to determine unique contributions of each item to the measure. Questions were removed from the RISQ-T, and RISQ-P if they showed little variability or an item-to-total correlation under 0.2. Parallel questions were then removed from the RISQ-P and RISQ-T, respectively. The final version of the RISQ-T included 20 items, and the final version of the RISQ-P included 15 items. Psychometrics of the final versions are described below.
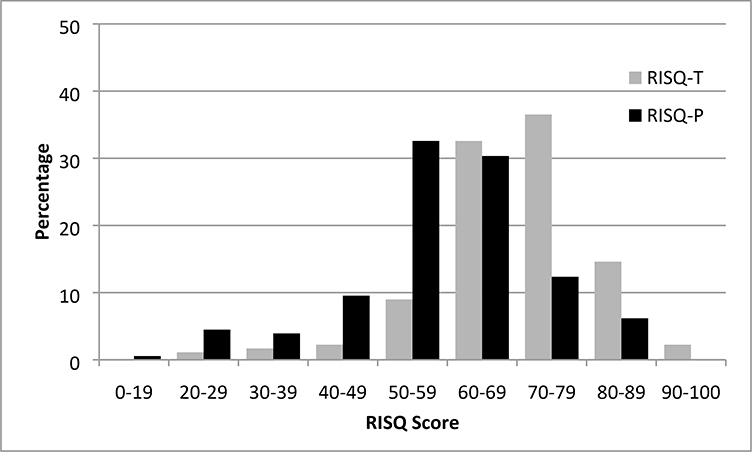
Distribution of the RISQ-T and RISQ-P scores are shown in Figure 1. Mean was 69.3±11.7 and 58.7±13.6 for RISQ-T and RISQ-P scores respectively. RISQ-T and RISQ-P were significantly correlated (r = .35, p<.0001) although adolescents reported significantly greater readiness for independent self-care than parents (t(177)=9.83, p<.0001). Both measures were significantly positively correlated with adolescent age (RISQ-T r=.21, p=.006 and RISQ-P r=.36, p<.0001). There were no significant differences in RISQ-T or RISQ-P scores between sexes or by insulin regimen. Neither survey was associated with diabetes duration and HbA1c.
Figure 1.
Distribution of RISQ-T and RISQ-P scores
3.3. Internal consistency of RISQ-T and RISQ-P
For both RISQ-T and RISQ-P, internal consistency (Cronbach α) was good: RISQ-T α=.78; RISQ-P α=.77. The domains revealed moderate levels of internal consistency: Knowledge, α RISQ-T=.51; α RISQ-P=.61; Behavior, α RISQ-T=.62; α RISQ-P=.71; and adolescent’s Perceived Importance α RISQ-T=.81. Item-to-total correlations ranged from 0.19 to 0.55, with 75% of items on the RISQ-T and 87% of items on the RISQ-P>0.25.
3.4. Concurrent validity
Associations between RISQ-T and RISQ-P total and domain scores with psychosocial surveys appear inTable 2a and Table 2b, respectively. Higher total scores on both measures were correlated with greater adolescent- and parent reported diabetes-related self-efficacy (RISQ-T r =.32; RISQ-P r= .54, both p<.0001), more treatment adherence (RISQ-T r=.26, p=.0004; RISQ-P r=.31, p<.0001), and less parental involvement (RISQ-T r= −.34; RISQ-P r=−.47, both p<.0001). No association was found between RISQ-T and adolescent-reported diabetes-related burden, while higher scores on the RISQ-P were associated with less parent-reported diabetes-related burden (r=−.30, p<.0001).
Table 2a –
Pearson correlations between RISQ-T total and domain scores with adolescent age and psychosocial survey scores (adolescent reports)
| Total RISQ-T | Knowledge | Behavior | Importance | |
|---|---|---|---|---|
| Adolescent age | .21b | .11 | .21 b | .12 |
| Parent involvement | −.34 d | −.23 b | −.39 d | −.10 |
| Self-efficacy | .32 d | .28 c | .30 d | .13 |
| Treatment adherence | .26 c | .12 | .26 c | .19 a |
| Diabetes burden | −.07 | −.12 | −.03 | −.03 |
p<.05
p<.01
p<.001
p<.0001
Table 2b –
Pearson correlations between RISQ-P total and domain scores with adolescent age and psychosocial survey scores (parent reports)
| Total RISQ-P | Knowledge | Behavior | |
|---|---|---|---|
| Adolescent age | .36 d | .28 c | .32 d |
| Parent involvement | −.47 d | −.31 d | −.48 d |
| Self-efficacy | .54 d | .35 d | .56 d |
| Treatment adherence | .31 d | .21 b | .31 d |
| Diabetes burden | −.30 d | −.17 a | −.33 d |
p<.05
p<.01
p<.001
p<.0001
Similar to correlations with total scores, domain scores also showed significant associations with psychosocial measures. The Knowledge domain of both the RISQ-T and RISQ-P were positively correlated with adolescent- and parent-reported diabetes-related self-efficacy (RISQ-T Knowledge r=.28, p=.0002; RISQ-P Knowledge r=.35, p<.0001). Only the RISQ-P Knowledge domain was positively related to treatment adherence (RISQ-P r=.21, p=.006). The Behavior domain on both measures was also positively correlated with adolescent- and parent-reported self-efficacy (RISQ-T Behavior r=.30 p<.0001; RISQ-P Behavior r=.56, p<.0001). Behavior domain scores on both measures were also positively correlated with adolescent- and parent-reported treatment adherence (RISQ-T r=.26, p=.0006; RISQ-P r=.31, p<.0001). The Importance domain of the RISQ-T was positively related to adolescent-reported treatment adherence (RISQ-T r=.19, p=.01) but not self-efficacy.
3.5. Test-retest reliability
The intraclass correlation coefficients (ICC) between RISQ scores, after six months, were acceptable for RISQ-T (r=.66) and RISQ-P (r=.71).
3.6. Predictive validity
Associations between the RISQ-T and RISQ-P with changes in family involvement, adolescent adherence, and glycemic control were assessed at 6 months. In a statistically significant model (controlling for age, sex, baseline HbA1c, and baseline adolescent report of family involvement; R2=0.22, p<.0001), RISQ-T baseline scores did not predict adolescent-reported change in parent involvement. In contrast, parallel analyses with parent reports (R2=0.17, p<.0001) revealed that baseline RISQ-P scores predicted significant reduction in parent involvement (β=−.14, p=.02). RISQ-T and RISQ-P baseline scores did not predict adolescent- or parent-reported changes in adolescent adherence or adolescent HbA1c.
4. Discussion
Readiness for independent self-care is a first step in the shift of responsibility for diabetes management from parents to adolescents, and can be considered as a precursor to transfer from pediatric to adult healthcare. With the RISQ-T and the RISQ-P, we introduce an adolescent- and parent-version of a novel, brief questionnaire to assess adolescent readiness for independent self-care during adolescence prior to transfer to adult health care. The current validation study indicated that the 20-item RISQ-T and 15-item RISQ-P are valid and reliable novel measures of adolescent readiness for independent self-care. Other measures, such as the generic TRAQ and the diabetes-specific READDY, used with adolescents and young adults, have focused on readiness for transfer from pediatric to adult health care [12, 23]. The RISQ surveys may be considered precursors to that, as they emphasize readiness for independent self-care in adolescents as a first step to autonomous diabetes management prior to transfer to adult healthcare. These novel surveys offer opportunities to help screen for ‘yellow flags’[30] in routine clinical care by identifying gaps in adolescent knowledge of basic diabetes care, the frequency and ability to engage in self-management behaviors, and adolescent perceptions of the importance of independent diabetes self-care. Further, they may assess the impact of transition-focused interventions, and may be optimally suited to be used in the patient-centered approach of shared-decision making [31] with adolescents and parents (e.g., when deciding on which self-management behaviors to focus in an adolescent’s trajectory towards more independence).
Our study indicated that adolescents perceived themselves as more ready to engage in independent self-care than their parents perceived them to be. This finding points to the importance of assessing both adolescent and parent reports of adolescent readiness for independent self-care, as adolescent emotional and cognitive maturity [32] may not always allow the best estimation of their own knowledge and behaviors. Despite these differences, the RISQ-T and RISQ-P were significantly correlated, supporting the valid performance of the surveys. Further, both RISQ-T and RISQ-P showed adequate internal consistency and test-retest reliability.
Adolescent readiness for independent self-care was associated with higher levels of adolescent self-efficacy and treatment adherence by both adolescent- and parent-reports. This suggests that greater perceived readiness to independently manage diabetes is associated with greater confidence in adolescents’ abilities and may manifest as greater treatment adherence. Future interventions focused on improving adolescents’ confidence in their abilities to independently manage diabetes may be beneficial to enhance adolescent readiness. Further, readiness for independent self-care was associated with lower parent involvement in diabetes care. This natural shift in responsibility from parent to adolescent may have a bidirectional relationship with perceived readiness, as readiness may be enhanced by less involvement, and less involvement may increase readiness. Additionally, the finding that more parent-perceived readiness for adolescent independent self-care was associated with less parental burden suggests that parents may feel relief when they believe their adolescents are capable of performing diabetes self-care on their own. No associations of the RISQ-T or RISQ-P were found with glycemic control, a finding that deserves further investigation, as it could point to a disconnect between perceptions of readiness for independent self-care and self-care behaviors that would lead to better glycemic control.
Lastly, analysis of predictive validity demonstrated significant associations between higher baseline RISQ-P scores and decreases in parent-reported family involvement after six months. This finding warrants clinical attention and further research, as less parental involvement in diabetes care over time may be an explanatory factor for the finding that more readiness for independent self-care is not related to better treatment adherence nor improved glycemic control. Clinical interventions that focus on structured and timely shifts of responsibility for diabetes care from parents to youth in order to enhance adherence and glycemic control while maintaining parental guidance and support, may be beneficial.
The present study has certain limitations. First, generalizability of our findings may be hampered by the relatively homogeneous nature of our sample of predominantly Caucasian adolescents from two-parent families with higher socioeconomic status. Generalizability may also be limited by the relatively higher than usual rates of blood glucose monitoring and pump use and the lower average HbA1c of our sample compared to other clinic-based samples of youth with type 1 diabetes[2]. Future studies utilizing the RISQ-T and RISQ-P may benefit from replication in a more diverse sample reflective of national demographics and outcomes for adolescents with type 1 diabetes. Second, due to the study design, test-retest reliability was calculated at a six-month interval. As changes in adolescent readiness for independent self-care could be partially accounted for by developmental maturation and growth, future studies could benefit from assessing test-retest reliability at a shorter time interval.
Despite these limitations, the current study may have important clinical implications. Adolescent readiness for independent self-care is likely an evolving process that involves a timely, yet sequenced, transfer of responsibilities for diabetes self-care tasks from parents to adolescents. Assessing adolescent readiness for independent self-care with validated adolescent self- and parent proxy-reported questionnaires may help identify at-risk adolescents as well as improve self-care for adolescents with type 1 diabetes during the transition period. The RISQ questionnaires may inform adolescents, families, and providers of adolescents’ progress toward more autonomous management and indicate those in need of greater support.
In conclusion, RISQ-T and RISQ-P appear to be reliable and valid measures of adolescent readiness for independent self-care, with strong applicability to clinical settings, and future research focusing on the highly relevant process of transition and transfer from pediatric to adult health care settings.
Acknowledgments
Funding
This research was supported by NIH grants R01DK095273, K12DK094721, T32DK007260, and P30DK036836; JDRF grant 2-SRA-2014-253-M-B; Bringing Science Home; the Katherine Adler Astrove Youth Education Fund; the Maria Griffin Drury Pediatric Fund; and the Eleanor Chesterman Beatson Fund. Dr. Goethals’ work on this project was supported by the Belgian American Educational Foundation (BAEF), and a Mary K. Iacocca Research Fellowship provided by the Iacocca Family Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of these organizations.
Footnotes
We have no relevant conflict of interest to disclose.
Portions of this manuscript were presented at the 75th Scientific Sessions of the American Diabetes Association, June 5–9, 2015, Boston, MA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wood JR, et al. , Most youth with type 1 diabetes in the T1D Exchange Clinic Registry do not meet American Diabetes Association or International Society for Pediatric and Adolescent Diabetes clinical guidelines. Diabetes Care, 2013. 36(7): p. 2035–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster NC, et al. , State of Type 1 Diabetes Management and Outcomes from the T1D Exchange in 2016–2018. Diabetes Technol Ther, 2019. 21(2): p. 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Snelgrove RK, McGill DE, and Laffel LM, Adolescence and Emerging Adulthood: Diabetes in Transition, in Textbook of Diabetes, Holt RIG et al. , Editors. 2017, Wiley-Blackwell: Chichester, West Sussex, UK; Hoboken, NJ, USA: p. 896–908. [Google Scholar]
- 4.Goethals ER, et al. , Child and parental executive functioning in type 1 diabetes: Their unique and interactive role toward treatment adherence and glycemic control. Pediatr Diabetes, 2018. 19(3): p. 520–526. [DOI] [PubMed] [Google Scholar]
- 5.Borus JS and Laffel L, Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr, 2010. 22(4): p. 405–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blum RW, et al. , Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health, 1993. 14(7): p. 570–576. [DOI] [PubMed] [Google Scholar]
- 7.Peters A, Laffel L, and The American Diabetes Association Transitions Working Group, Diabetes care for emerging adults: Recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care, 2011. 34(11): p. 2477–2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cameron FJ, et al. , ISPAD Clinical Practice Consensus Guidelines 2018: Diabetes in adolescence. Pediatr Diabetes, 2018. 19 Suppl 27: p. 250–261. [DOI] [PubMed] [Google Scholar]
- 9.Pierce JS, et al. , Health Care Transition for Young Adults With Type 1 Diabetes: Stakeholder Engagement for Defining Optimal Outcomes. J Pediatr Psychol, 201742(9): p. 970–982. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz LA, et al. , Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol, 2014. 39(6): p. 588–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sawicki GS, et al. , Measuring the Transition Readiness of Youth with Special Healthcare Needs: Validation of the TRAQ--Transition Readiness Assessment Questionnaire. J Pediatr Psychol, 2011. 36(2): p. 160–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corathers SD, et al. , Development and Implementation of the Readiness Assessment of Emerging Adults With Type 1 Diabetes Diagnosed in Youth (READDY) Tool. Diabetes Spectrum, 2019: p. ds18–0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markowitz JT, Garvey KC, and Laffel LM, Developmental changes in the roles of patients and families in type 1 diabetes management. Curr Diabetes Rev, 2015. 11(4): p. 231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goethals ER, et al. , Parenting and Treatment Adherence in Type 1 Diabetes Throughout Adolescence and Emerging Adulthood. J Pediatr Psychol, 2017. 42(9): p. 922–932. [DOI] [PubMed] [Google Scholar]
- 15.Vesco AT, et al. , Responsibility sharing between adolescents with type 1 diabetes and their caregivers: importance of adolescent perceptions on diabetes management and control. J Pediatr Psychol, 2010. 35(10): p. 1168–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Diabetes A, 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2020. Diabetes Care, 2020. 43(Suppl 1): p. S48–S65. [DOI] [PubMed] [Google Scholar]
- 17.Deshpande S, Basil MD, and Basil DZ, Factors influencing healthy eating habits among college students: an application of the health belief model. Health Mark Q, 2009. 26(2): p. 145–64. [DOI] [PubMed] [Google Scholar]
- 18.Eakin MN, et al. , Development and validation of CF-Medication Beliefs Questionnaire: A mixed-methods approach. J Cyst Fibros, 2017. 16(5): p. 637–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Commissariat PV, et al. , Associations between major life events and adherence, glycemic control, and psychosocial characteristics in teens with type 1 diabetes. Pediatr Diabetes, 2018. 19(1): p. 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanenbaum ML, et al. , Adapting and validating a measure of diabetes-specific self-compassion. J Diabetes Complications, 2018. 32(2): p. 196–202. [DOI] [PubMed] [Google Scholar]
- 21.Orji R, Vassileva J, and Mandryk R, Towards an effective health interventions design: an extension of the health belief model. Online J Public Health Inform, 2012. 4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harris PA, et al. , Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform, 2009. 42(2): p. 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wood DL, et al. , The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr, 2014. 14(4): p. 415–22. [DOI] [PubMed] [Google Scholar]
- 24.Anderson BJ, et al. , Assessing family sharing of diabetes responsibilities. J Pediatr Psychol, 1990. 15(4): p. 477–492. [DOI] [PubMed] [Google Scholar]
- 25.Giani E, et al. , Validation of the Diabetes Management Self-Efficacy Survey for teens with T1D and their parents [Abstract]. Diabetes, 2016. 65(Suppl 1): p. A209. [Google Scholar]
- 26.Markowitz JT, et al. , Youth-perceived burden of type 1 diabetes: Problem Areas in Diabetes survey-Pediatric version (PAID-Peds). J Diabetes Sci Technol, 2015. 9(5): p. 1080–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markowitz JT, et al. , Re-examining a measure of diabetes-related burden in parents of young people with Type 1 diabetes: the Problem Areas in Diabetes Survey - Parent Revised version (PAID-PR). Diabet Med, 2012. 29(4): p. 526–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mehta SN, et al. , Validation of a contemporary adherence measure for children with Type 1 diabetes: the Diabetes Management Questionnaire. Diabet. Med, 2015. 32(9): p. 1232–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mulvaney SA, et al. , Development and initial validation of the barriers to diabetes adherence measure for adolescents. Diabetes Res Clin Pract, 2011. 94(1): p. 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eilander MM, et al. , Disturbed eating behaviors in adolescents with type 1 diabetes. How to screen for yellow flags in clinical practice? Pediatr Diabetes, 2017. 18(5): p. 376–383. [DOI] [PubMed] [Google Scholar]
- 31.Wieringa TH, et al. , Decision aids that facilitate elements of shared decision making in chronic illnesses: a systematic review. Syst Rev, 2019. 8(1): p. 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cameron FJ, Northam EA, and Ryan CM, The effect of type 1 diabetes on the developing brain. Lancet Child Adolesc Health, 2019. 3(6): p. 427–436. [DOI] [PubMed] [Google Scholar]