Abstract
Objective
School hearing screening may mitigate the effects of childhood hearing loss through early identification and intervention. This study provides an overview of existing school hearing screening programs around the world, identifies gaps in the literature, and develops priorities for future research.
Data Sources
A structured search of the PubMed, Embase, and Cochrane Library databases.
Review Methods
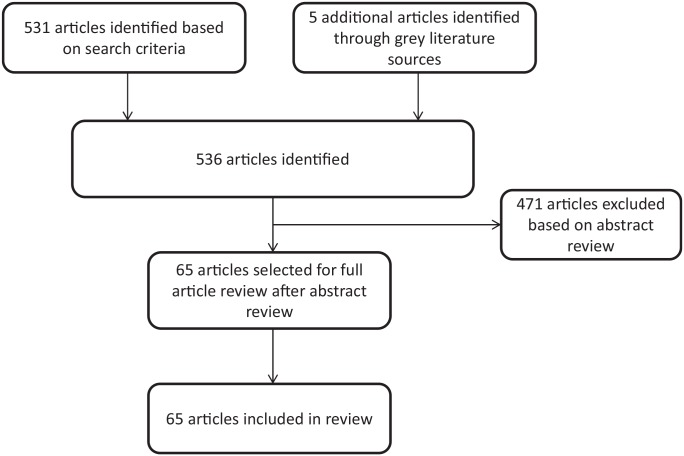
A total of 65 articles were included according to predefined inclusion criteria. Parameters of interest included age groups screened, audiometric protocols, referral criteria, use of adjunct screening tests, rescreening procedures, hearing loss prevalence, screening test sensitivity and specificity, and loss to follow-up.
Conclusions
School hearing screening is mandated in few regions worldwide, and there is little accountability regarding whether testing is performed. Screening protocols differ in terms of screening tests included and thresholds used. The most common protocols included a mix of pure tone screening (0.5, 1, 2, and 4 kHz), otoscopy, and tympanometry. Estimates of region-specific disease prevalence were methodologically inaccurate, and rescreening was poorly addressed. Loss to follow-up was also a ubiquitous concern.
Implications for Practice
There is an urgent need for standardized school hearing screening protocol guidelines globally, which will facilitate more accurate studies of hearing loss prevalence and determination of screening test sensitivity and specificity. In turn, these steps will increase the robustness with which we can study the effects of screening and treatment interventions, and they will support the development of guidelines on the screening, diagnostic, and rehabilitation services needed to reduce the impact of childhood hearing loss.
Keywords: school hearing screening, hearing loss, children, school, audiometry, tympanometry, otoacoustic emissions
Hearing loss represents a growing global health concern. From 2010 to 2013, hearing loss rose from the 13th-leading cause of years lived with disability to the second-leading cause, with 1.3 billion people affected worldwide.1-3 Despite this, hearing loss elicits little attention in comparison with other chronic conditions.4 Childhood hearing loss is associated with speech and language delays, low literacy, decreased educational attainment, higher likelihood of school dropout, and restricted employment opportunities.5 The World Health Organization estimates that 60% of childhood hearing loss may be preventable.6 Connecting children with timely and appropriate ear and hearing care is critical and can circumvent long-term sequelae.7,8 This is particularly important in low- and middle-income countries, which bear >80% of the global burden of hearing loss.9
Universal screening for hearing loss in newborns has been successful and standardized in many high-income countries around the world, and efforts to expand these programs are ongoing.10-12 While newborn screening has improved our ability to identify and treat congenital hearing loss, children who may have minimal losses at birth, experience progressive losses, or develop hearing loss later in childhood—for example, from recurrent middle ear disease—often remain unidentified and without care. Regional data from the United Kingdom illustrate the effect of progressive, late-onset, or acquired hearing loss by estimating that the adjusted prevalence increases from approximately 0.11% in children aged 3 years to 0.21% in children aged 9 to 15 years.13 In their early years, children are at particularly high risk of developing hearing loss as a result of otitis media, or inflammation in the middle ear.14-17 Other causes of childhood hearing loss include infections (eg, meningitis, pertussis), regular exposure to secondhand smoke or loud noise, ototoxic medications, and head trauma.14-18 Primary education, which is focused on establishing fundamental literacy and numeracy skills, is compulsory in almost all countries, making schools a key access point for integrated health checks such as hearing screening, which reduces the sociodemographic inequities of access to health care.19
The World Health Organization and a number of studies to date suggest that school hearing screening may allow for timely identification of childhood hearing loss and may be a cost-effective means of addressing the burden of undiagnosed hearing loss in school-aged children.15,18,20-23 However, data on the implementation of school hearing screening programs are limited. Some countries, such as New Zealand and Sweden, report established postnewborn hearing screening programs, but these occur strictly in the preschool age group.24,25 In addition, there has been recent conflicting evidence on the utility of school hearing screening, with a study in 2016 showing an unfavorable cost-effectiveness analysis based on data from a single region.13 The applicability of these findings to other geographic areas is uncertain, and there is a need for additional high-quality, region-specific data from other parts of the world. While some regions, such as the United States and Europe, have proposed standardized guidelines, most other areas lack data on best practices for school-based hearing screening.17,26 As such, there are no current international guidelines for school hearing screening available.
The objective of this review was to characterize current policies and practices for school hearing screening globally, examining the effectiveness of existing programs in identification, referral, and follow-up. We assessed the shortcomings of current screening protocols, identified gaps in the evidence supporting school hearing screening, and developed priorities for future research on this topic.
Methods
Based on preliminary literature searches, it was apparent that protocols and mandates surrounding school hearing screening varied widely in regions across the world. Heterogeneous study designs, lack of methodologic rigor of individual articles, and an overall thin literature base precluded rigorous analysis of studies. With the goal of including as many articles as possible for review, instead of restricting articles due to exclusions based on methodologic design, we chose to structure this report as a narrative review. Methodologic elements of a scoping review, as outlined by the guidelines of the PRISMA Extension for Scoping Reviews, were nevertheless included to enhance rigor and minimize bias.27
Inclusion Criteria
Studies were included that examined school hearing screening programs on school-aged children. Inclusion criteria included hearing screening studies, analyses of currently existing hearing screening protocols, or outlined guidelines for a recommended protocol. School hearing screening was defined as any screening for hearing loss performed from school entry to postsecondary education. The age range for “school-aged” was not defined numerically due to the expected variation in age at initial school entry among regions.
Exclusion Criteria
Studies were excluded if they encompassed only newborn or preschool hearing screening programs.
Search Strategy
A structured search was performed through 3 primary databases: PubMed, Embase, and Cochrane Library. The search strategy used MeSH terms and keywords related to school, children, and hearing screening (Appendix 1, available online). Sources of interest included but were not limited to primary research studies, reviews, meta-analyses, guidelines, and commentaries. A corresponding gray literature search was also performed primarily through the Google search engine and focused on region-specific published protocols, guidelines, or policies. Both searches were performed by the first and second authors in collaboration between August and September 2018.
Data Extraction and Analysis
Parameters of interest for articles reviewed in this report included age groups screened, audiometric protocols (including screening frequencies), referral criteria, use of adjunct tests (otoscopy, tympanometry, otoacoustic emissions [OAEs], other special tests), presence of a rescreen protocol, estimates of hearing loss prevalence, sample size of children screened, screening test performance characteristics (eg, sensitivity and specificity), and loss to follow-up. These data were tabulated in comparative tables and analyzed qualitatively.
Discussion
A total of 531 articles were identified after the initial search of the 3 databases. After title and abstract review to screen for relevance to school hearing screening, 471 studies were excluded, and a resultant 60 articles were assigned for full review. Gray literature search yielded another 5 articles and reports that were included. The total number of articles included in the review was 65 ( Figure 1 ).
Figure 1.
Search strategy according to inclusion criteria from 3 databases: PubMed, Embase, and Cochrane Library.
Article Types
There were 44 primary research studies found in the literature search. These were divided into geographic regions for the purpose of data representation (Supplemental Tables S1-S6, available online). Other gray literature resources, reports, and guidelines describing current recommendations and policies accounted for the remaining 21 articles.
Etiology of Hearing Loss in School Children
The majority of articles focused on 6 main causes of hearing loss in school-aged children: progressive congenital conditions, otitis media with effusion, drug-related ototoxicity, infection, cerumen impaction, and noise exposure. There was concern that children who pass newborn hearing screening may have undetected progressive hearing loss or can still develop hearing loss related to congenital causes later in childhood.14-18 In regions without newborn hearing screening, school hearing screening represented the first point of access to ear and hearing care. Otitis media with effusion was a ubiquitous concern, with many studies suggesting that it was the main cause of conductive hearing loss in younger children.22,28-34 In low- and middle-income regions, including some parts of sub-Saharan Africa and Asia, bacterial and viral infections were identified as important etiologies for permanent hearing loss.17,35 Related to this, drug-related ototoxicity was reported to be a significant concern, especially in areas with a high prevalence of infectious diseases because of the use of systemic ototoxic antibiotics.17,22,29,35 Cerumen impaction was also listed as a major contributor to conductive hearing loss, especially in low- and middle-income regions.22,30,34 For example, cerumen impaction was related to 12.6% of all conductive hearing loss in southern India, and cerumen contributed to hearing loss in 39% of children during screening in Malaysia.31,36 Finally, noise-induced hearing loss was highlighted as a growing concern in adolescents in all regions worldwide due to the increasing use of personal sound devices for recreation and exposure to work-related noise hazards.17,37-42
Screening Mandates
There was a scarcity of guidelines on school hearing screening globally and inconsistent implementation of the few guidelines that exist. For example, only 66% of states within the United States currently carry out any form of school hearing screening despite national recommendations that hearing screening take place at regular intervals.43 Hearing screening is recommended in South Africa, but there are no available data on the amount of screening that takes place.44 In the United Kingdom, approximately 10% of schools do not provide school entry screening despite recommendations.45 Other countries had either little or no published data on current school hearing screening regulations or policies.
Screening Equipment
Most studies used conventional audiometers to perform screening tests. A select number of studies used mobile audiometers without sound booths or teleaudiometry (remote testing) to perform audiometric screening.18,23,46-48 These studies recommended that these alternative methods can improve access to hearing screening for underserved areas, such as rural locations.
The environment in which screening was carried out was most often a quiet school setting (eg, an empty classroom). The majority of countries used noise-reducing headphones to minimize the effects of ambient noise.
Screening Tests
Across all regions worldwide, pure tone screening was considered an indispensable aspect of school hearing screening protocols and the gold standard as a confirmatory diagnostic test for hearing loss. However, the audiometric frequencies and referral criteria varied widely among studies. Even within countries such as the United States, protocol frequencies ranging from 0.25 to 8 kHz were noted. The most common tested frequencies were 0.5, 1, 2, and 4 kHz. Articles that evaluated hearing loss in older adolescents drew particular attention to the importance of additional high-frequency testing at 6 and 8 kHz, as these frequencies are most often affected by noise exposure.38-42,46 Referral criteria in almost all studies involved failure to hear at any 1 frequency in either ear, but the threshold limits differed greatly among studies. The most commonly used threshold was ≥20 dB HL with headphones, but difficulties with ambient noise even in a quiet school testing environment caused some authors to choose higher threshold limits, ranging from 25 to 40 dB HL.
There was variation in the recommended adjunct tests that should be included in the school hearing screening protocol, which included otoscopy, tympanometry, and OAEs. The most commonly used screening protocols incorporated a combination of otoscopy and tympanometry in addition to standard use of pure tone screening.
Otoscopy was recommended as an important adjunct test given its usefulness in detecting obvious outer and middle ear abnormalities requiring medical follow-up.31,34,49 It was a well-tolerated procedure that was often used prior to audiometric screening and tympanometry to yield more accurate screening results. It was also particularly helpful in regions with high prevalence of cerumen impaction.31,36,50 However, there was little guidance on who should be performing otoscopic screening.51 Most studies employed trained students, specialized nurses, audiologists, or physicians as screeners, limiting the generalizability of the recommendation in low-resource settings.*
Tympanometry was recommended as another highly useful test owing to the importance of evaluating middle ear pathology such as otitis media.18,22,29,60,61 There was some variability regarding the decision to include it as a first-line screening test or to reserve it as a second-line test after initial referred screening by pure tone screening or OAE testing.14,29,50,61 A few authors recommended either immediately referring abnormal tympanometry results for medical follow-up or repeating screening at least 1 month later to check for resolution.14,34,61
OAEs were recommended to be a part of the routine school hearing screening battery in a smaller proportion of studies and guidelines. Current data indicate that OAE screening is less sensitive and yields a higher number of false positives than pure tone screening.53 Most authors found OAEs to be more relevant in situations where children were unable to follow directions for hearing screening, such as those who are very young or those with special needs.14,50,53 In these cases, OAEs may be useful as first-line screening tests due to the objective nature of the test.14
Rescreening
A major area lacking agreement in existing screening protocols was the process of immediately rescreening children who referred from initial hearing screening. Several authors have cited that a high false-positive rate among hearing screening protocols has been a major cost burden associated with school hearing screening.18,34 Immediate rescreening after an initial referred screen can be used to reduce false positives, yet the majority of studies did not include rescreening. This is a seemingly simple yet incredibly important aspect of hearing screening protocols that can have a profound impact on the overall viability of the intervention.
Prevalence and Screening Test Performance Parameters
One of the most striking findings was the lack of articles estimating the true prevalence of hearing loss among school children. Although 17 articles included prevalence estimates, ranging from 0.9% in Taiwan55 to 34% in Brazil,62 many other articles provided referral percentages of screening tests in lieu of prevalence.† These studies assumed 100% sensitivity in their screening protocols and did not include a comparison with gold standard pure tone audiometry, meaning that any estimates on disease prevalence represented screening test referral percentages rather than true measures of disease prevalence. The prevalence estimates that these studies provided were therefore noted as “referral percentages” in the comparison tables (“REF” in Supplemental Tables S1-S6, available online). The referral percentage among these studies ranged from 0.16% in China to 15% in Malaysia.36,63 The reporting of referral percentages also made it impossible to interpret any estimation of sensitivity and specificity as an accurate measure of the true performance of screening protocols. Distinguishing between an estimate of true prevalence and the reporting of a particular protocol’s referral percentage is critical, as some existing hearing screening protocols have sensitivities as low as 12%.38 This makes them unsuitable to be used as a viable screening strategy.38,39,68 In addition, there is some suspicion that the true prevalence of hearing loss among school children may be higher than current estimates.66
Challenges of Follow-up
A key issue surrounding school hearing screening was loss to follow-up for children who were referred. Out of 44 primary research articles, only 8 reported any data on follow-up of students after hearing screening referral. These studies reported follow-up ranging from 10% to 65%.14,15 Potential reasons cited for poor follow-up included the inability to contact and notify parents of the screening test results, the lack of parental awareness of the medical significance of hearing loss, the cost of subsequent care, the inability of parents to miss work, and geographic barriers.15,29,34,69 Letter mail and telephone calls were the favored modes of communication, but the majority of studies did not document or recommend guidelines for follow-up.15,16,39,42 Other concerns related to loss to follow-up in low- and middle-income countries included shortages of specialist care and inadequate infrastructure for continued educational support.22 Overall, there was a near-unanimous recommendation that addressing lost to follow-up is urgently needed to improve the overall effectiveness of school hearing screening programs across the world.18,34,46
Limitations
The narrative nature of this review makes it possible that information and selection bias could be present. To minimize these sources of bias, close adherence to the guidelines of the PRISMA Extension for Scoping Reviews was maintained through use of a predetermined and structured search algorithm of 3 literature databases, as well as a gray literature search. Additionally, while it is recognized that countries such as New Zealand and Sweden have robust preschool hearing screening programs that occur after initial newborn hearing screening, these programs were excluded from this review because they fall outside school-aged hearing screening and thus are beyond the scope of this analysis.24,25 Finally, articles were not critically appraised and graded for methodologic design, which could add a potential source of bias. However, as stated in the methodologic justification, this specific study design was chosen because of the heterogeneity and methodologic inaccuracies among the existing school screening literature.
Implications for Practice
School hearing screening programs have the potential to mitigate many of the cascading negative effects of childhood hearing loss but are currently lacking because of either poor political and financial commitment or an incorrect assumption that all childhood hearing loss is detected through newborn hearing screening programs. When school hearing screening programs are implemented, protocols and practices are inconsistent, in part, because of the limited number of regional or country-wide guidelines that exist. There is an urgent need for further research in this area and the establishment of globally standardized school hearing screening protocols, not only to encourage and improve the quality of early detection and diagnosis of hearing loss through hearing screening programs, but also to increase comparability across research studies. Data capture is a fundamental component of any screening program for quality assurance and monitoring and to evaluate its longer-term success in mitigating the educational disadvantage that hearing loss can have within this population.70 Hearing aids and cochlear implants, as part of an early intervention program, have proven effectiveness in addressing hearing loss and, when fitted early, can reduce the economic burden on society.71 Classroom amplification, FM systems, and other classroom and listening strategies augmented with parental support are also core components of an early intervention program for permanent hearing loss or chronic middle ear disease.
On the basis of the findings in this review—and as a minimum starting point—we advocate for the inclusion of pure tone screening with circumaural headphones at 1, 2, and 4 kHz, with a referral threshold of >20 dB HL at any frequency in either ear. However, determination of the referral threshold should be considered within the context of available diagnostic and rehabilitation services, given the increased false positives associated with a lower referral threshold. Noise levels should be assessed to ensure that the screening environments are suitable for testing.26 Screening with OAEs may be an alternative for children where pure tone screening is not feasible, but the utility of OAEs for school screening as a replacement for pure tone screening needs further research.
Tympanometry with a standard 226-Hz probe tone should be included where possible, as well as direct otoscopic examination provided that screening personnel possess an adequate level of training. Rescreening should be a mandatory step that occurs immediately after children do not pass initial screening. It is important for diagnostic and treatment services to be available and accessible for children identified through screening programs. Lastly, a documented follow-up procedure should exist to ensure that referred children are reliably connected to diagnostic and treatment services, thereby reducing eventual losses to follow-up.
The establishment of standardized school hearing screening guidelines is a critical step for expansion of standardized school screening programs globally and will facilitate the performance of higher-quality studies, which are needed to provide more accurate, region-specific estimates of disease prevalence. Additionally, standardization will aid in the development of protocols that optimize the sensitivity and specificity of screening tests, which could contribute to improved efficacy of school hearing screening programs globally.
Author Contributions
Michael Yong, study design, search algorithm, data collection, data analysis, manuscript writing; Neelima Panth, data collection, data analysis, manuscript writing; Catherine M. McMahon, manuscript editing critical for intellectual content; Peter R. Thorne, manuscript editing critical for intellectual content; Susan D. Emmett, study design, manuscript editing critical for intellectual content.
Disclosures
Competing interests: None.
Sponsorships: Michael Yong is supported by the University of British Columbia’s Clinician Investigator Program.
Funding source: None.
Supplemental Material
Supplemental material, Appendix_1 for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_1_-_North_America for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_2_-_Africa for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_3_-_Australasia for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_4_-_Europe for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_5_-_Middle_East for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_6_-_South_America for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Acknowledgments
This article serves as background for the World Health Organization’s World Report on Hearing.
Supplemental Material: Additional supporting information is available at http://journals.sagepub.com/doi/suppl/10.1177/2473974X20923580
References
- 1. Vos T, Flaxman A, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789-1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hearing loss: an important global health concern. Lancet. 2016;387(10036):2351-2352. [DOI] [PubMed] [Google Scholar]
- 5. Wilson BS, Tucci DL, Merson MH, O’Donoghue GM. Global hearing health care: new findings and perspectives. Lancet. 2017;390(10111):2503-2515. [DOI] [PubMed] [Google Scholar]
- 6. Childhood hearing loss: strategies for prevention and care. Published 2016. Accessed September 1, 2018 http://apps.who.int/iris/bitstream/handle/10665/204632/9789241510325_eng.pdf? sequence=1
- 7. Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):E43. [DOI] [PubMed] [Google Scholar]
- 8. Robinshaw HM. Early intervention for hearing impairment: differences in the timing of communicative and linguistic development. Br J Audiol. 1995;29(6):315-334. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization. WHO global estimates on prevalence of hearing loss. Published 2012. Accessed September 1, 2018 http://www.who.int/pbd/deafness/WHO_GE_HL.pdf?ua=1
- 10. Pimperton H, Blythe H, Kreppner J, et al. The impact of universal newborn hearing screening on long-term literacy outcomes: a prospective cohort study. Arch Dis Child. 2016;101(1):9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Muse C, Harrison J, Yoshinaga-Itano C, et al. Supplement to the JCIH 2007 position statement: principles and guidelines for early intervention after confirmation that a child is deaf or hard of hearing. Pediatrics. 2013;131(4):e1324-e1349. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization. Newborn and infant hearing screening: current issues and guiding principles for action. Published 2010. Accessed September 1, 2018 http://www.who.int/blindness/publications/Newborn_and_Infant_Hearing_Screening_Report.pdf
- 13. Fortnum H, Ukoumunne OC, Hyde C, et al. A programme of studies including assessment of diagnostic accuracy of school hearing screening tests and a cost-effectiveness model of school entry hearing screening programmes. Health Technol Assess. 2016;20(36):1-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Subcommittee on Childhood Hearing Screening. American Academy of Audiology Childhood Hearing Screening Guidelines. Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 15. Flanary VA, Flanary CJ, Colombo J, Kloss D. Mass hearing screening in kindergarten students. Int J Pediatr Otorhinolaryngol. 1999;50(2):93-98. [DOI] [PubMed] [Google Scholar]
- 16. Baur K, Cook D, Guillory L, Herndon D, Park K. Guidelines for Hearing Screening in the School Setting. Missouri Department of Health and Senior Services; 2015. [Google Scholar]
- 17. Skarżyński H, Piotrowska A. Prevention of communication disorders—screening pre-school and school-age children for problems with hearing, vision and speech: European consensus statement. Med Sci Monit. 2012;18(4):SR17-SR21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swanepoel DW, Maclennan-Smith F, Hall JW. Diagnostic pure-tone audiometry in schools: mobile testing without a sound-treated environment. J Am Acad Audiol. 2013;24(10):992-1000. [DOI] [PubMed] [Google Scholar]
- 19. UNESCO. Global education monitoring report target 4.1—primary and secondary education. Published 2017. Accessed March 16, 2020 https://gem-report-2017.unesco.org/en/chapter/primary-and-secondary-education/
- 20. World Health Organization. Deafness and hearing loss. Published 2018. Accessed September 1, 2018 http://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
- 21. North-Matthiassen C, Singh SA. The hearing profile among learners in schools in the Western Cape, South Africa. Int J Pediatr Otorhinolaryngol. 2007;71(1):113-118. [DOI] [PubMed] [Google Scholar]
- 22. Westerberg BD, Skowronski DM, Stewart IF, Stewart L, Bernauer M, Mudarikwa L. Prevalence of hearing loss in primary school children in Zimbabwe. Int J Pediatr Otorhinolaryngol. 2005;69(4):517-525. [DOI] [PubMed] [Google Scholar]
- 23. Georgalas C, Xenellis J, Davilis D, Tzangaroulakis A, Ferekidis E. Screening for hearing loss and middle-ear effusion in school-age children, using transient evoked otoacoustic emissions: a feasibility study. J Laryngol Otol. 2008;122(12):1299-1304. [DOI] [PubMed] [Google Scholar]
- 24. Gray S. Before School Check Audit. Counties Manukau District Health Board; 2014. [Google Scholar]
- 25. Stenfeldt K. Preschool hearing screening in Sweden: an evaluation of current practices and a presentation of new national guidelines. Int J Pediatr Otorhinolaryngol. 2018;110:70-75. [DOI] [PubMed] [Google Scholar]
- 26. American Academy of Audiology. Childhood hearing screening guidelines. Published 2011. Accessed September 1, 2018 https://www.cdc.gov/ncbddd/hearingloss/documents/aaa_childhood-hearing-guidelines_2011.pdf
- 27. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. [DOI] [PubMed] [Google Scholar]
- 28. New Zealand Health Technology Assessment. Screening Programmes for the Detection of Otitis Media with Effusion and Conductive Hearing Loss in Pre-school and New Entrant School Children: A Critical Appraisal of the Literature. New Zealand Health Technology Assessment; 1998. NZHTA Report 3 [Google Scholar]
- 29. Clark JL. Hearing loss in Mozambique: current data from Inhambane Province. Int J Audiol. 2008;47(suppl 1):49. [DOI] [PubMed] [Google Scholar]
- 30. Minja BM, Machemba A. Prevalence of otitis media, hearing impairment and cerumen impaction among school children in rural and urban Dar es Salaam, Tanzania. Int J Pediatr Otorhinolaryngol. 1996;37(1):29-34. [DOI] [PubMed] [Google Scholar]
- 31. Jacob A, Rupa V, Job A, Joseph A. Hearing impairment and otitis media in a rural primary school in south India. Int J Pediatr Otorhinolaryngol. 1997;39(2):133-138. [DOI] [PubMed] [Google Scholar]
- 32. Thorne JA. Middle ear problems in Aboriginal school children cause developmental and educational concerns. Contemp Nurse. 2004;16(1-2):145-150. [DOI] [PubMed] [Google Scholar]
- 33. American Speech-Language-Hearing Association. Guidelines for audiology service provision in and for schools. Published 2002. Accessed August 7, 2018 https://www.asha.org/policy/GL2002-00005/#r10
- 34. Govender S, Latiff N, Asmal N, Ramsaroop S, Mbele T. Evaluating the outcomes of a hearing screening service for grade one learners in urban areas at Durban, South Africa. J Public Health Afr. 2015;6(1):529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Osei AO, Larnyo PA, Azaglo A, Sedzro TM, Torgbenu EL. Screening for hearing loss among school going children. Int J Pediatr Otorhinolaryngol. 2018;111:7-12. [DOI] [PubMed] [Google Scholar]
- 36. Khairi Md, Daud M, Noor RM, Rahman NA, Sidek DS, Mohamad A. The effect of mild hearing loss on academic performance in primary school children. Int J Pediatr Otorhinolaryngol. 2010;74(1):67-70. [DOI] [PubMed] [Google Scholar]
- 37. Taylor EJ, Emanuel DC. Assessment of the efficacy of a hearing screening program for college students. J Am Acad Audiol. 2013;24(7):607-615. [DOI] [PubMed] [Google Scholar]
- 38. Sekhar DL, Rhoades JA, Longenecker AL, et al. Improving detection of adolescent hearing loss. Arch Pediatr Adolesc Med. 2011;165(12):1094-1100. [DOI] [PubMed] [Google Scholar]
- 39. Sekhar DL, Zalewski TR, Ghossaini SN, et al. Pilot study of a high-frequency school-based hearing screen to detect adolescent hearing loss. J Med Screen. 2014;21(1):18-23. [DOI] [PubMed] [Google Scholar]
- 40. Sekhar DL, Zalewski TR, Paul IM. Variability of state school-based hearing screening protocols in the United States. J Community Health. 2013;38(3):569-574. [DOI] [PubMed] [Google Scholar]
- 41. Meinke DK, Dice N. Comparison of audiometric screening criteria for the identification of noise-induced hearing loss in adolescents. Am J Audiol. 2007;16(2):190. [DOI] [PubMed] [Google Scholar]
- 42. Meinke DK, Meade S, Johnson CDC, Jensema J. Occupational model of mobile audiometric testing for high school students. Semin Hear. 2008;29(01):49. [Google Scholar]
- 43. American Speech-Language-Hearing Association. State Hearing Screening Requirements. American Speech-Language-Hearing Association; 2019. [Google Scholar]
- 44. South African Speech-Language Hearing Association. Standards and Guidelines for Speech-Language Therapists Working in Hearing Screening in Schools. South African Speech-Language Hearing Association; 2011. [Google Scholar]
- 45. National Screening Committee. The UK NSC Policy on Hearing Screening in Children. National Screening Committee; 2006. [Google Scholar]
- 46. Skarzyński PH, Świerniak W, Piłka A, et al. A hearing screening program for children in primary schools in Tajikistan: a telemedicine model. Med Sci Monit. 2016;22:2424-2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Botasso M, Sanches SGG, Bento RF, Samelli AG. Teleaudiometry as a screening method in school children. Clinics (Sao Paulo). 2015;70(4):283-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Monica SD, Ramkumar V, Krumm M, Raman N, Nagarajan R, Venkatesh L. School entry level tele-hearing screening in a town in South India—lessons learnt. Int J Pediatr Otorhinolaryngol. 2017;92:130-135. [DOI] [PubMed] [Google Scholar]
- 49. Basañez I, Nakku D, Stangl S, Wanna GB. Prevalence of hearing loss among primary school children in Mbarara, Uganda. Int J Pediatr Otorhinolaryngol. 2015;79(12):2359-2363. [DOI] [PubMed] [Google Scholar]
- 50. Chen H, Wang N, Chiu W, et al. A test protocol for assessing the hearing status of students with special needs. Int J Pediatr Otorhinolaryngol. 2014;78(10):1677-1685. [DOI] [PubMed] [Google Scholar]
- 51. Beals M, Larson SD, Kaplan B, et al. Hearing Screening Guidelines for the Pre-school/School Population. State of Alaska Department of Health and Social Services; 2016. [Google Scholar]
- 52. Lancaster P, Krumm M, Ribera J, Klich R. Remote hearing screenings via telehealth in a rural elementary school. Am J Audiol. 2008;17(2):114-122. [DOI] [PubMed] [Google Scholar]
- 53. Krueger WWO, Ferguson L. A comparison of screening methods in school-aged children. Otolaryngol Head Neck Surg. 2002;127(6):516-519. [DOI] [PubMed] [Google Scholar]
- 54. Elango S, Purohit GN, Hashim M, Hilmi R. Hearing loss and ear disorders in Malaysian school children. Int J Pediatr Otorhinolaryngol. 1991;22(1):75-80. [DOI] [PubMed] [Google Scholar]
- 55. Yang T, Wu C, Liao W, Yeh K, Chou P. Mean hearing thresholds among school children in Taiwan. Ear Hear. 2011;32(2):258-265. [DOI] [PubMed] [Google Scholar]
- 56. Mourad MI, Farghaly NF, Mohamed HG. Hearing impairment: is it a public health problem among primary school pupils in Alexandria? J Egypt Public Health Assoc. 1993;68(5-6):703-726. [PubMed] [Google Scholar]
- 57. Sarafraz M, Ahmadi K. A practical screening model for hearing loss in Iranian school-aged children. World J Pediatr. 2009;5(1):46-50. [DOI] [PubMed] [Google Scholar]
- 58. TarvijEslami S, Nassirian H, Bayesh S. Impact on performance of hearing screening program through prevalence and diagnostic age evaluation in elementary school students in north-eastern city of Iran, Mashhad. Pediatria Polska. 2017;92(6):705-710. [Google Scholar]
- 59. Czechowicz JA, Messner AH, Alarcon-Matutti E, et al. Hearing impairment and poverty: the epidemiology of ear disease in Peruvian schoolchildren. Otolaryngol Head Neck Surg. 2010;142(2):272-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Winston-Gerson R, Sabo DL. Hearing loss detection in schools and early child care settings: an overview of school-age hearing screening practices. NASN Sch Nurse. 2016;31(5):257-262. [DOI] [PubMed] [Google Scholar]
- 61. Ministry of Health. The B4 School Check: A Handbook for Practitioners. Ministry of Health; 2008. [Google Scholar]
- 62. Nogueira JCR, Mendonça MdC. Assessment of hearing in a municipal public school student population. Braz J Otorhinolaryngol. 2011;77(6):716-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Fu S, Chen G, Dong J, Zhang L. Prevalence and etiology of hearing loss in primary and middle school students in the Hubei Province of China. Audiol Neurootol. 2010;15(6):394-398. [DOI] [PubMed] [Google Scholar]
- 64. Hattori H. Two-level screening audiometry in public school. Auris Nasus Larynx. 1989;16(suppl 1):15. [DOI] [PubMed] [Google Scholar]
- 65. Hu T, Stead K, Fu T, Papsin B. A program evaluation of Kids2Hear, a student-run hearing screening program for school children. J Otolaryngol Head Neck Surg. 2016;45(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Śliwa L, Hatzopoulos S, Kochanek K, Piłka A, Senderski A, Skarżyński PH. A comparison of audiometric and objective methods in hearing screening of school children: a preliminary study. Int J Pediatr Otorhinolaryngol. 2011;75(4):483-488. [DOI] [PubMed] [Google Scholar]
- 67. Bamford J, Fortnum H, Bristow K, et al. Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen. Health Technol Assess. 2007;11(32):1-168. [DOI] [PubMed] [Google Scholar]
- 68. Kam ACS, Gao H, Li LKC, Zhao H, Qiu S, Tong MCF. Automated hearing screening for children: a pilot study in China. Int J Audiol. 2013;52(12):855-860. [DOI] [PubMed] [Google Scholar]
- 69. Hendershot C, Pakulski LA, Thompson A, Dowling J, Price JH. School nurses’ role in identifying and referring children at risk of noise-induced hearing loss. J Sch Nurs. 2011;27(5):380-389. [DOI] [PubMed] [Google Scholar]
- 70. Helfer TM, Lee RB, Maris DC, Shields AR. Wanted: a national standard for early hearing detection and intervention outcomes data. Am J Audiol. 2003;12(1):23-30. [DOI] [PubMed] [Google Scholar]
- 71. Ching T, Dillon H, Button L, et al. Age at intervention for permanent hearing loss and 5-year language outcomes. Pediatrics. 2017;140(3):e20164274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix_1 for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_1_-_North_America for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_2_-_Africa for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_3_-_Australasia for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_4_-_Europe for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_5_-_Middle_East for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation
Supplemental material, Table_6_-_South_America for How the World’s Children Hear: A Narrative Review of School Hearing Screening Programs Globally by Michael Yong, Neelima Panth, Catherine M. McMahon, Peter R. Thorne and Susan D. Emmett in OTO Open: The Official Open Access Journal of the American Academy of Otolaryngology-Head and Neck Surgery Foundation