Abstract
Background:
Meniscal root tears and ramp lesions have been rigorously characterized in recent literature. However, one of the most common lateral meniscal injuries identified with an acute anterior cruciate ligament (ACL) disruption, a posterior horn lateral meniscal oblique radial tear (LMORT), has not been thoroughly described.
Purpose:
To determine the incidence of all meniscal tears and, more specifically, the incidence of posterior horn LMORTs in a multicenter cohort of consecutive, acute ACL reconstructions. Additionally, the authors aimed to develop a new classification system to help guide treatment of posterior horn LMORTs.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A multicenter retrospective cohort design was used to analyze 200 consecutive cases of acute ACL reconstruction from each of 3 different surgeons, for a total of 600 patients. The operative notes and intraoperative photos were analyzed to determine the incidence and laterality of all meniscal tears. A classification system based on tear characterization was then used to categorize tear patterns into similar groups.
Results:
A total of 396 (66%) of the 600 patients with acute ACL disruption had concomitant meniscal tears. Specifically, 187 (31%) had a lateral meniscal injury, 89 (15%) had a medial meniscal injury, and 122 (20%) had both medial and lateral meniscal injuries. The most common lateral meniscal tear was an LMORT; 71 (18%) patients with meniscal tears had a posterior horn LMORT. Overall, the incidence of ACL injury with a concomitant posterior horn LMORT was 12%. A classification was developed, which included type 1 tear (partial thickness <10 mm from the root attachment), type 2 tear (complete radial oblique tear that extended <10 mm from root), type 3 tear (incomplete LMORT that extended >10 mm from root), and type 4 tear (complete LMORT >10 mm from root).
Conclusion:
In 600 consecutive acute ACL reconstructions, the incidence of concomitant ACL injury with meniscal injury was 66%, and posterior horn LMORTs represented a large proportion of all meniscal tears (12%). A classification scheme was developed for posterior horn LMORTs to aid reporting and clinical decision making for these common tears.
Keywords: LMORT, lateral meniscus, oblique meniscal tear, oblique radial tear, meniscal tear
There has been recent interest in better quantifying the incidence of concomitant meniscal tears with anterior cruciate ligament (ACL) injury. In addition, improved characterization of common tear patterns can lead to advancement of recognition and treatment options. It is well established that meniscal tears may greatly alter the biomechanics of the knee, leading to increased contact pressures, instability, and accelerated development of osteoarthritis.2,7,12,13,17,24 Studies have reported the incidence of meniscal tears associated with ACL tears to range between 47% and 65%.1,7,9,14,18,19 Unlike medial meniscal tears, which commonly occur chronically after ACL injury, lateral meniscal tears occur most commonly with acute ACL injuries.4,5,7,8 Posterior meniscal tears commonly occur concurrently with ACL injuries.19 Westermann et al23 found that more than 84% of patients with ACL injury and meniscal injury had posterior meniscal injuries alone, whereas only 14% of patients had both anterior and posterior meniscal injuries. Concurrent ACL reconstruction with meniscal repair has been shown to be effective in the short and long term, with long-term failure rates between 10% and 29%.22,23
Meniscal root tears and ramp lesions have been rigorously characterized in recent literature. However, one of the most common lateral meniscal injuries identified with an acute ACL disruption, a posterior horn lateral meniscal oblique radial tear (LMORT), has not been thoroughly described. The classification system by LaPrade et al11 was created for both medial and lateral meniscal root tears. In that classification system, a type 4 tear is a complete radial tear located less than 10 mm from the meniscus root, but this does not adequately characterize the LMORT, as the majority of these tears extend beyond 10 mm from the root origin. Therefore, the distance to the posterior root and the severity (partial vs complete) of these LMORTs directly affect the type of treatment. Duchman et al6 found that small, stable, peripheral lateral meniscal tears fared well without repair, but another report showed that large radial lateral meniscal tears were associated with instability and pain and often required repair.15 The consequences of leaving these tears untreated are currently unknown, although significant long-term morbidity is a genuine concern.
Therefore, the purpose of this study was to determine the incidence of all meniscal tears and, more specifically, the incidence of posterior horn LMORTs in a multicenter cohort of consecutive acute ACL reconstructions. Additionally, we aimed to develop a new classification system that would aid recognition and perhaps guide the treatment method for posterior horn LMORTs. We hypothesize that a more thorough classification system will improve the intraoperative identification of each tear type and help guide decision making in the clinical setting.
Methods
Institutional review board approval was obtained for this study. A multicenter retrospective review of prospectively collected data was used to analyze 200 consecutive acute ACL reconstruction surgeries from each of 3 different surgeons for a total cohort of 600 patients. The surgeon reviewers were also the treating surgeons. Each surgeon inspected the lateral and medial compartments intraoperatively and prospectively recorded any meniscal injuries, including the location, laterality, size, and shape of the tear. The tear size was measured with a graduated probe at the time of arthroscopy and recorded in the operative notes. Arthroscopic photographs were taken to carefully document the tear. Patients who sustained an ACL tear were included in the study. Patients with concomitant ligamentous injuries that were low grade and treated nonoperatively were also included in the study. Patients were excluded if they had a multiligament reconstruction or prior meniscal surgery.
An electronic chart review was performed to analyze the operative report and demographic information for each patient undergoing an ACL reconstruction from 2013 to 2019 (Table 1). A total of 200 consecutive ACL repairs were analyzed for each of the 3 sports medicine–trained orthopaedic surgeons. Of the 3 reviewers, 2 reviewers (M.J.S. and P.A.S.) each have 30 years of experience, whereas the third (A.J.K.) has 10 years of experience. The operative notes and intraoperative photos were reanalyzed retrospectively, and the incidence and laterality of the meniscal tears were noted. The lateral meniscal tears were then subclassified according to tear size, location, pattern, and repair type. Arthroscopic photographs of each tear were personally reviewed by 2 reviewers (A.J.K. and M.J.S.) until consensus was reached. In cases of disagreement, the tear type was again reviewed until consensus was reached between the 2 reviewers. Once the patterns were finalized, a classification system using tear characterization was used to categorize tear patterns into similar groups.
Table 1.
Patient Demographic Information
| Demographic Parameter | n (%)a |
|---|---|
| Sex | |
| Male | 346 (57.7) |
| Female | 254 (42.3) |
| Mean age, y | 23.1 |
| Mean body mass index, kg/m2 | 25.8 |
| Mechanism of injury | |
| Noncontact | 454 (75.7) |
| Contact | 136 (22.7) |
| Activity level | |
| Sedentary | 31 (5.2) |
| Recreational | 227 (37.8) |
| Competitive | 331 (55.2) |
| Unknown | 11 (1.8) |
| Smoker | |
| No | 548 (91.3) |
| Yes | 52 (8.7) |
aValues are expressed as n (%), except for age and body mass index.
Statistical analysis was performed using Microsoft Excel to create diagrams and calculate descriptive statistical values, including percentages.
Results
Of the 600 patients with acute ACL tears, 396 patients (66%) had a concomitant meniscal tear. Specifically, 187 (31%) had a lateral meniscal injury, 89 (15%) had a medial meniscal injury, and 122 (20%) had bilateral meniscal injuries (Table 2). Of the patients with meniscal tears, 71 (18%) patients had posterior horn LMORTs (Table 3). The incidence of ACL injury with concomitant posterior horn LMORTs was 11.8%.
Table 2.
Characteristics and Locations of Meniscal Tears
| Characteristics and Locations | n (%) |
|---|---|
| Meniscal injury | |
| Lateral alone | 187 (31.2) |
| Medial alone | 89 (15) |
| Both | 122 (20.3) |
| Other injuriesa | |
| Medial collateral ligament | 82 (13.7) |
| Posterior cruciate ligament | 17 (2.8) |
| Lateral collateral ligament | 19 (3.2) |
| Side | |
| Left | 298 (49.7) |
| Right | 302 (50.3) |
aConcomitant ligamentous injuries were low grade and were treated nonoperatively.
Table 3.
Lateral Meniscal Tear Characteristicsa
| Characteristic | n |
|---|---|
| Anatomic location | |
| Anterior horn | 10 |
| Body | 78 |
| Posterior horn | 273 |
| Meniscocapsular | 4 |
| Central | 90 |
| Peripheral | 33 |
| Tear type | |
| Lateral meniscal oblique radial | 71 |
| Vertical longitudinal | 112 |
| Root avulsion | 34 |
| Radial | 69 |
| Bucket handle | 16 |
| Horizontal cleavage | 14 |
| Superficial (partial) | 18 |
| Complex (defined as ≥1 tear plane) | 34 |
aThe number of tears is larger than number of patients with tear because some patients had bilateral tears or multiple tears on 1 meniscus.
We identified 4 types of posterior horn LMORTs during the study. The tears were classified into 4 groups based on the severity of the tear and the distance from the root, with each group having specific suggested treatments. Type 1 tears were identified as partial-thickness radial oblique tears less than 10 mm from the posterior root attachment. Type 1 tears were treated with partial meniscectomy. Type 2 tears were identified as complete radial oblique tears that extended less than 10 mm from the lateral meniscus posterior root attachment site but did not involve the attachment site. Type 2 tears were addressed with transtibial pullout root repair, as this radial tear near the root is structurally similar to a posterior root tear. Type 3 tears were identified as incomplete (not entirely through the posterior rim of the meniscus) LMORTs that extended more than 10 mm from the posterior root. Type 4 tears were complete (entirely through the posterior rim to the meniscofemoral ligament, which remained intact) LMORTs extending more than 10 mm from the posterior root. Type 3 and type 4 tears were repaired with all-inside repair (either knot-tying with suture placement via self-retrieving instrument or all-inside suture device) or inside-out repair. The types of LMORTs are shown in Figures 1 and 2.
Figure 1.
Illustrations of the 4 types of posterior horn lateral meniscal oblique radial tears. The tear types were classified to include a corresponding treatment for each. The tear types were (1) partial oblique tear <10 mm from the lateral root (type 1); (2) complete oblique tear <10 mm from the root attachment, but not involving the root site (type 2); (3) incomplete oblique tear extending >10 mm from the root (type 3); and (4) complete oblique tear extending >10 mm from the root (type 4). Type 1 tears were repaired with partial meniscectomy. Type 2 tears were repaired with transtibial pullout repair. Type 3 and type 4 tears were repaired with all-inside suture repair or, rarely, with inside-out suture repair. Ant, anterior; LM, lateral meniscus; Post, posterior.
Figure 2.
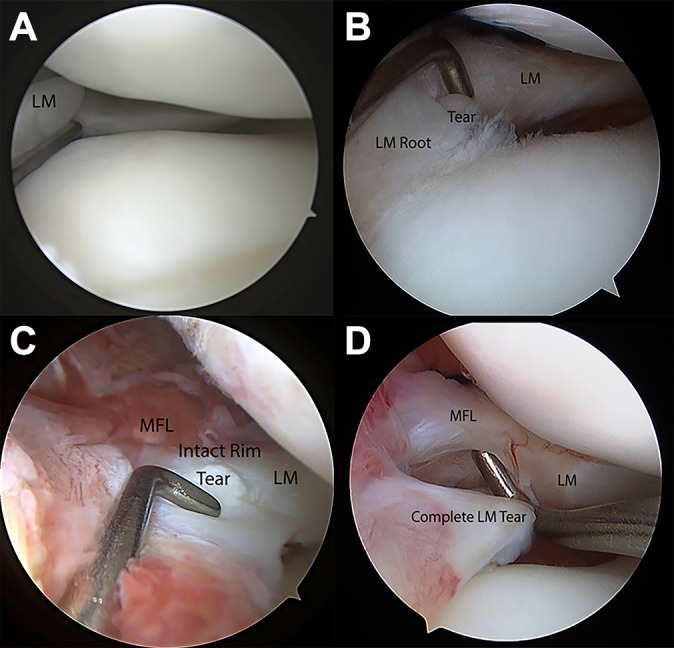
Arthroscopic views of the 4 types of posterior horn lateral meniscal oblique radial tears. (A) Type 1: partial oblique tear <10 mm from the lateral root. (B) Type 2: complete oblique tear <10 mm from the root attachment, but not involving the root site. (C) Type 3: incomplete oblique tear extending >10 mm from the root. (D) Type 4: complete oblique tear extending >10 mm from the root. LM, lateral meniscus; MFL, meniscofemoral ligament.
Of the 71 posterior horn LMORTs, 7 (9.9%) were type 1 tears, 9 (12.7%) were type 2 tears, 21 (29.6%) were type 3 tears, and 34 (47.9%) were type 4 tears (Table 4). For the type 1 tears, 6 tears were treated with partial meniscectomy; the seventh tear was stable and no treatment was performed. For type 2 tears, all 9 tears were treated with transtibial root repairs. For type 3 and type 4 tears, 53 tears were treated with all-inside repair and 2 tears were treated with inside-out repair.
Table 4.
Frequency of Each Lateral Meniscal Oblique Radial Tear Type
| Tear Type | n (%) | Repair Performed |
|---|---|---|
| Type 1 | 7 (9.9) | None: 1 Partial meniscectomy: 6 |
| Type 2 | 9 (12.7) | Transtibial repair: 9 |
| Type 3 | 21 (29.6) | All-inside repair: 21 |
| Type 4 | 34 (47.9) | All-inside repair: 32 Inside-out repair: 2 |
Discussion
A subtype of lateral meniscal tears—LMORTs—have not been described in detail despite their frequent occurrence. The purpose of this study was to better quantify the incidence of meniscal tears in patients undergoing ACL reconstruction and to create a novel classification system for posterior horn LMORTs in order to better guide identification and treatment of these meniscal tears. Our analysis of 600 consecutive acute ACL reconstructions found the incidence of meniscal injuries to be 66% and the incidence of posterior horn LMORTs to be 11.8%. We also classified radial oblique tears of the lateral meniscus into types 1 through 4 to aid reporting and decision making in the clinical setting.
The incidence of meniscal tears with concomitant ACL injury in our study (66%) was slightly higher than the incidence of 47% to 61% reported in previous studies. This could be due to the fact that 93% of our patients were recreational or competitive athletes, and our patients were younger on average than other studies.3,18,20 The mechanism for these posterior horn lateral meniscal tears is likely the pivot-shift phenomenon, where subluxation in the lateral compartment of the lateral femoral condyle compresses the posterior horn of the lateral meniscus. Sports participation and the pivot-shift mechanism of injury have been reported to be major causes of lateral meniscal injuries.3,20 In a recent biomechanical study, Tang et al21 found that posterior lateral meniscal tears diminished knee stability in patients with ACL reconstruction and that lateral meniscal repair significantly improved knee stability under pivot-shift loadings. Krych et al10 recently demonstrated that a high percentage of lateral meniscus posterior root tears were missed on magnetic resonance imaging (MRI). The high frequency of posterior lateral meniscal injury and the frequency of missed findings on MRI highlight the importance of posterior horn visualization through the intercondylar notch and probing of the meniscus at the time of arthroscopy. Preservation of the lateral meniscus whenever possible is important given its vital role as a secondary stabilizer of the knee.10,16
Posterior horn LMORTs represented a significant proportion (23%) of lateral meniscal tears. We could not find any previous reports about the incidence of posterior horn LMORTs that did not include posterior root tears. In a study of 314 pediatric and adolescent patients with meniscal injury, Wilson et al24 found that 15% of patients had lateral meniscus posterior root injuries and that lateral meniscal root injuries occurred with ACL injuries 85% of the time. Praz et al18 found the incidence of ACL injury with concomitant lateral meniscus posterior root tear to be 6.6%, but those authors did not include incomplete radial or longitudinal tears. Although the majority of radial oblique tears in our study were type 3 or 4 tears, 8.5% of tears in our study were partial tears (type 1), which could partially explain why the incidence of posterior horn tears was lower in the study by Praz et al.
We believe that we have generated a useful classification system for a tear type that has not been adequately described despite the high incidence of 12% with concomitant ACL injuries found in this study. To the best of our knowledge, no other classification system has focused on posterior horn LMORTs. Forkel et al8 and LaPrade et al11 previously classified different types of meniscal tears; however, they primarily focused on root tears and radial oblique tears within 10 mm of the lateral meniscus root attachment, which represented only 22.6% of all posterior horn LMORTs. Our study found that 77.4% of posterior horn LMORTs extended more than 10 mm from the root attachment. The suggested surgical treatment of these tears needs further clinical study. A recent study by Tsujii et al22 found that 90% of the 30 patients who underwent second-look arthroscopy 2 years after concomitant ACL reconstruction and radial posterior lateral meniscal repair had excellent healing rates. Tsujii et al exclusively performed repairs using all-inside and inside-out repairs. Further study is necessary to replicate these findings and to evaluate the clinical effectiveness of the proposed transtibial repairs for the type 2 tears discussed in this study.
Strengths of the current study include the large sample size of consecutive ACL repairs performed by experienced, board-certified, sports medicine orthopaedic surgeons. Limitations include the retrospective nature of using prospectively collected data. In addition, it was difficult to classify each meniscal tear, especially at the beginning of the study before the classification system had been created. We attempted to limit biases by having 2 reviewers analyze each arthroscopic photograph to reach a consensus.
In 600 consecutive acute ACL reconstructions, the incidence of concomitant ACL injury with meniscal injury was 66%, and posterior horn LMORTs represented a large proportion of all meniscal tears (12%). A classification scheme was developed for posterior horn LMORTs to improve accurate identification and focused treatment of these common tears.
Footnotes
Final revision submitted January 30, 2020; accepted February 13, 2020.
One or more of the authors has declared the following potential conflict of interest or source of interest: A.J.K. has received research support from Aesculap/B.Braun, Ceterix, Exactech, Gemini Medical, and Histogenics; consulting fees from Arthrex, JRF Ortho, and Vericel; speaking fees from Arthrex; and royalties from Arthrex; he is a board or committee member for the Musculoskeletal Transplant Foundation and has stock/stock options in Responsive Arthroscopy. M.D.L. has a family member with the following disclosures: consulting fees from Arthrex, Linvatec, Ossur, and Smith & Nephew; research support and speaking fees from Smith & Nephew; grant support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950); and royalties from Arthrex, Ossur, Smith & Nephew, and Thieme. M.J.S. has received research support from Arthrex and Stryker and consulting fees and royalties from Arthrex. P.A.S. has received research support, consulting fees, and royalties from Arthrex; educational support from Elite Orthopedics; and speaking fees from Arthrex and Alpha Orthopedic Systems and has stock/stock options in Spinal Simplicity. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic Institutional Review Board (study No. PR15-000601-05).
References
- 1. Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67–75. [DOI] [PubMed] [Google Scholar]
- 2. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 3. Beldame J, Wajfisz A, Lespagnol F, Hulet C, Seil R. Lateral meniscus lesions on unstable knee. Orthop Traumatol Surg Res. 2009;95(8) (suppl 1):S65–S69. [DOI] [PubMed] [Google Scholar]
- 4. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 5. Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Duchman KR, Westermann RW, Spindler KP, et al. The fate of meniscus tears left in situ at the time of anterior cruciate ligament reconstruction: a 6-year follow-up study from the MOON cohort. Am J Sports Med. 2015;43(11):2688–2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Feucht MJ, Bigdon S, Bode G, et al. Associated tears of the lateral meniscus in anterior cruciate ligament injuries: risk factors for different tear patterns. J Orthop Surg Res. 2015;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–118. [DOI] [PubMed] [Google Scholar]
- 9. Granan LP, Inacio MC, Maletis GB, Funahashi TT, Engebretsen L. Intraoperative findings and procedures in culturally and geographically different patient and surgeon populations: an anterior cruciate ligament reconstruction registry comparison between Norway and the USA. Acta Orthop. 2012;83(6):577–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Krych AJ, Wu IT, Desai VS, et al. High rate of missed lateral meniscus posterior root tears on preoperative magnetic resonance imaging. Orthop J Sports Med. 2018;6(4):23259 67118765722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 12. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–479. [DOI] [PubMed] [Google Scholar]
- 13. Magee T, Shapiro M, Williams D. MR accuracy and arthroscopic incidence of meniscal radial tears. Skeletal Radiol. 2002;31(12):686–689. [DOI] [PubMed] [Google Scholar]
- 14. Mansori AE, Lording T, Schneider A, Dumas R, Servien E, Lustig S. Incidence and patterns of meniscal tears accompanying the anterior cruciate ligament injury: possible local and generalized risk factors. Int Orthop. 2018;42(9):2113–2121. [DOI] [PubMed] [Google Scholar]
- 15. McDermott I. Meniscal tears, repairs and replacement: their relevance to osteoarthritis of the knee. Br J Sports Med. 2011;45(4):292–297. [DOI] [PubMed] [Google Scholar]
- 16. Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591–1597. [DOI] [PubMed] [Google Scholar]
- 17. Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, et al. Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy. 2016;32(4):624–633. [DOI] [PubMed] [Google Scholar]
- 18. Praz C, Vieira TD, Saithna A, et al. Risk factors for lateral meniscus posterior root tears in the anterior cruciate ligament-injured knee: an epidemiological analysis of 3956 patients from the SANTI study group. Am J Sports Med. 2019;47(3):598–605. [DOI] [PubMed] [Google Scholar]
- 19. Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–1443. [DOI] [PubMed] [Google Scholar]
- 20. Tandogan RN, Taser O, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):262–270. [DOI] [PubMed] [Google Scholar]
- 21. Tang X, Marshall B, Wang JH, et al. Lateral meniscal posterior root repair with anterior cruciate ligament reconstruction better restores knee stability. Am J Sports Med. 2019;47(1):59–65. [DOI] [PubMed] [Google Scholar]
- 22. Tsujii A, Yonetani Y, Kinugasa K, et al. Outcomes more than 2 years after meniscal repair for radial/flap tears of the posterior lateral meniscus combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(12):2888–2894. [DOI] [PubMed] [Google Scholar]
- 23. Westermann RW, Wright RW, Spindler KP, Huston LJ, Wolf BR. Meniscal repair with concurrent anterior cruciate ligament reconstruction: operative success and patient outcomes at 6-year follow-up. Am J Sports Med. 2014;42(9):2184–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilson PL, Wyatt CW, Romero J, Sabatino MJ, Ellis HB. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6(11):2325967118803888. [DOI] [PMC free article] [PubMed] [Google Scholar]



