Abstract
Background:
Studies have found that inappropriate use of non-sterile gloves (NSG) can affect hand hygiene compliance; the main risks are missing opportunities for hand hygiene and gloves being a vector for microbial transmission.
Aim:
The aims of this study were to explore the accuracy of healthcare worker (HCW) risk assessment and decision making regarding the use of NSG.
Methods:
The study was conducted in two acute NHS Trusts and a community social enterprise. A cross-sectional survey was carried out, followed by qualitative semi-structured interviews.
Findings:
There were highly significant differences at the 95% probability level between staff groups, unqualified staff being significantly more likely than qualified staff to report NSG use when not indicated (P < 0.0001). The primary motivating factor for staff to wear NSG was for personal protection; the secondary factor being the protection of patients. Staff were also motivated by a desire to create an image of professionalism. Respondents were more likely to follow the lead of seniors in their own profession.
Discussion:
The results suggest a necessity for change interventions aimed at unqualified staff such as healthcare assistants (HCAs). It would be beneficial to review the indications for glove use and amend organisational policies accordingly. Leaders in each professional staff group would be required to influence practice across organisations, taking into account motivating factors, and in association with multi-modal interventions to improve practice.
Keywords: Hand hygiene, glove use, knowledge, attitudes, healthcare workers, healthcare-associated infections
Background
Recent studies have focused on the impact of wearing non-sterile gloves (NSG) on adherence to hand hygiene. Guidance on the use of gloves emphasises the importance of changing gloves between procedures and patients and carrying out hand hygiene after their removal (Loveday et al., 2014). The main risks of inappropriate glove use are missing opportunities for hand hygiene and gloves being a vector for microbial transmission (World Health Organization [WHO], 2009).
Kurtz (2017) found that wearing gloves was a significant factor in lowering nurses’ compliance with hand hygiene. Boudjema et al. (2017) video recorded healthcare workers (HCWs) hand hygiene behaviour and found that the most common breach of hand hygiene protocol was the overuse of gloves. The risk of cross-infection has been demonstrated by Wilson et al. (2017a), who found the overall rate of cross-contamination associated with episodes of care where NSG were used was 49%, and Kang et al. (2017), who found that contamination occurred in 79.2% of simulations involving the removal of personal protective equipment (PPE).
Jackson and Griffiths (2014) conducted semi-structured interviews with registered nurses in the UK and found that fear of contact with dirt was a key driver in glove-donning behaviour, carried out to reduce the threat. The authors concluded that the behaviours were a form of self-protection rather than an infection prevention strategy.
Wilson et al. (2017b) investigated the attitudes of UK student nurses to the use of NSG and found that the most frequently cited reason for the decision to wear gloves was their own judgement. Decisions were not always based on an accurate assessment of the risk of exposure to body fluids, gloves being used for low-risk tasks such as washing patients and helping them to dress. Wilson et al. (2017a) found that the decision to wear gloves is strongly influenced by the emotional need for protection of self, rationalised by a misperception of risk to self and failure to recognise the risk of cross-contamination.
A number of authors have stated that an understanding of the drivers of glove use behaviour is required to design interventions to reduce misuse and overuse and that there is a need to further understand HCWs’ risk assessment regarding the use of gloves (Burdsall et al., 2017).
The aims of this study were to add to the existing evidence by further exploring HCWs’ risk assessment and decision making in relation to NSG use. The goals were to:
- explore HCW risk assessment and decision making regarding NSG;
- investigate hand hygiene behaviour in relation to NSG;
- examine the drivers for NSG use, in relation to feelings of dirt and disgust, perceived hazards, social norms and the influence of co-workers.
- investigate whether staff were aware of organisational policy.
Methods
The study was conducted in two acute Trusts and a community social enterprise, focusing on ward staff.
The study was conducted in two phases: a cross-sectional survey of healthcare staff using a self-completion questionnaire, followed by qualitative semi-structured interviews. The questionnaire and interview schedule were piloted with a selection of HCWs in advance of the main study, to ensure that they addressed the principal aims of the study and were comprehensible.
Cross-sectional survey
The questionnaire was divided into five sections looking at demographics, knowledge, attitudes, beliefs and hand hygiene. Questions used Likert-type scales plus some open questions so that further opinions could be freely expressed. The questionnaire was available in paper format and online.
The sample was purposive rather than random probability; however, the sample profile provides a good representation of the population of the hospitals. Statistical significance for differences between independent samples has been estimated at 95% probability using analysis of variance and z scores, assuming a normal approximation to the binomial distribution.
HCWs included registered nurses and midwives, doctors, healthcare assistants (HCAs), student nurses and allied health professionals (AHPs). The study was promoted via the organisations’ communications departments and engagement encouraged by senior staff. Follow-up visits to the wards by the research teams were carried out to raise the response rate for the questionnaires.
Qualitative semi-structured interviews
Staff were invited separately to take part in the interviews. Inclusion criteria were:
HCWs from participating organisations;
age ⩾ 18 years;
working clinically in wards.
Participant information sheets were distributed inviting people to participate and written informed consent was obtained using a pre-interview consent form. The interviews were recorded, transcribed and transcripts anonymised. Analysis was carried out using mind mapping to identify key themes. Mind maps were originally designed by Buzan and Buzan (2003) as a way of collating large quantities of information in a colourful, diagrammatic format where key elements of the central question are shown as branches and sub-branches. Mind maps provide a useful method to review large quantities of data where a visual overview can enhance understanding of the individual perspective (Whiting and Sines, 2012).
Favourable ethical opinion was obtained from the Health Research Authority and from all three participating organisations’ research departments. The study was adopted as a National Institute for Health Research portfolio study.
Results
The results from the questionnaire were analysed with simple descriptive cross-analyses. Quality checks were conducted in order to ensure accuracy and reliability of the uploaded datasets. Thirteen healthcare professionals were recruited for the interviews: six registered nurses (RN); five HCAs; one AHP; and one doctor. The main themes from the interviews were risk assessment, decision making, organisational policy, education and training, leadership, hand hygiene and patient experience.
Demographics
The final dataset consisted of 1084 completed questionnaires. Male respondents represented 18% (n = 196) of the sample and female respondents 80% (n = 873), with 2% (n = 23) unknown. The age ranges of respondents were 18–24 years (15%, n = 169), 25–34 years (29%, n = 322), 35–44 years (24%, n = 267), 45–54 years (18%, n = 198), 54–64 years (11%, n = 123) and the remainder 65+ years or not known (n = 14). Of respondents, 8% (n = 83) had worked in healthcare for < 1 year, 46% (n = 504) for 1–9 years and 45% (n = 498) for > 10 years. A range of HCWs were represented: 10% (n = 114) doctors; 38% (n = 406) RNs; 5% (n = 55) student nurses; 20% (n = 219) HCAs; 20% (n = 193) AHPs; and 3% (n = 41) not known.
Knowledge
Overall, respondents had a good understanding of the indications for glove use, the majority stating that they would wear NSG for indications recommended in national guidance: 95% (n = 1002) would wear gloves when dealing with body fluids; 92% (n = 971) barrier nursing; and 80% (n = 944) said they always wear gloves for tasks such as cleaning commodes. Similar high proportions would always/often wear gloves for intimate care (87%, n = 894) or toileting assistance (87%, n = 915).
Some respondents indicated that they considered sterile gloves to be appropriate for tasks involving aseptic technique, e.g. caring for central venous devices.
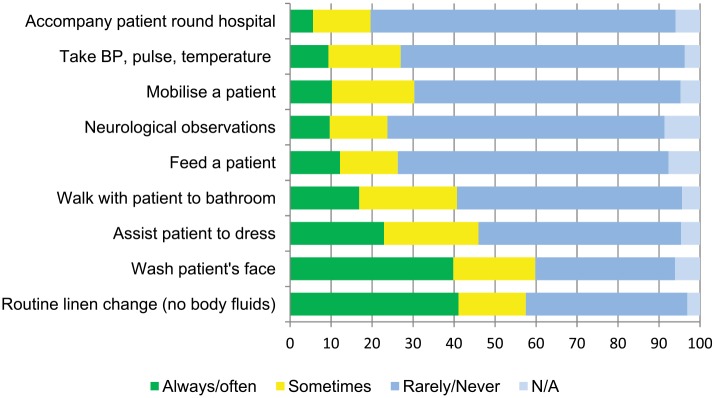
Responses regarding the routine use of NSG for tasks not indicated in national guidance are shown in Figure 1. There were highly significant differences at the 95% probability level between staff groups, unqualified staff being significantly more likely than qualified staff to report NSG use when not indicated (P < 0.0001), for example assisting patients to dress and mobilise, and cardiovascular observations.
Figure 1.
Percentage responses as to whether NSG gloves should be worn for tasks where NSG are not indicated (n = 1044).
Risk assessment and decision making
From the interviews, the main hazards perceived when deciding to wear NSG were associated with the risk of infection and body fluids. The principal motivating factor for staff to wear NSG was for personal protection, with the secondary motivating factor being the protection of patients.
Interviewees were questioned about fear of contact with ‘dirt’ being a key driver in behaviour carried out to reduce threat. The concept of ‘dirt’ was associated with body fluids, faeces in particular. Patients being seen as ‘dirty’ affected 27% (n = 276) of healthcare staff in their decision to wear NSG, and 44% (n = 443) of respondents agreed that their decision to wear NSG would be influenced by whether the patients could meet their self-care needs.
The principal influences on decision making on when to wear NSG were whether a patient had a known systemic (82%, n = 836) or topical infection (92%, n = 941). Only 4% (n = 41) agreed that wearing gloves to reduce having to wash their hands so often influenced their decision making.
Of the respondents, 27% (n = 273) agreed with the statement that ‘it is normal in our ward to wear gloves when touching a patient,’ with one-fifth of respondents agreeing that they sometimes wear gloves even when it is not necessary. Although only 7% (n = 73) agreed that they wear gloves because everyone else on the ward does so, the qualitative data suggest that HCWs, as a matter of course, wear gloves for most patient interactions. At interview, respondents stated that NSGs were worn for reasons that were not related to infection control, especially the desire to look professional and to portray an image of cleanliness.
‘Wearing gloves has visual message of being safe and showing that you are doing the right thing by wearing them.’ (RN)
Organisational policy
There was a high level of agreement in the questionnaires that staff were aware of the hospital policy on glove use (81%, n = 842), with 79% (n = 817) agreeing that they follow the hospital policy for glove use. However, participants in the interviews stated that they had not actively sought the hospital policy on glove use and had not seen any formal guidelines. The interviewees reported witnessing many examples of inappropriate glove use, e.g. mobilising patients, or wearing the same gloves for more than one patient, suggesting that HCWs do not always follow policy, even if they are aware of it.
‘Some people put gloves on for everything, even if they are pushing a bed down the corridor.’ (HCA)
Education and training
Glove use had been included in mandatory training for many of the interviewees; however, respondents commented that the sessions were mainly focused on hand hygiene and the detail on correct glove use was less in-depth. Knowledge was acquired from a mixture of mandatory training, general experience and observations on the wards:
‘I have watched other people, but no-one has specifically said this is what you do when you have to put on the gloves.’ (HCA)
The correct use of gloves was not consequently embedded in any organisational training, many using their own initiative to devise practice. However, a junior doctor and student nurse did confirm that hand washing and glove use were covered in their respective medical school and nurse training.
Leadership/Social influences
Behaviour regarding glove use was felt by interviewees to be influenced by those around them. Interviewees would be more likely to follow the lead of senior clinical staff in their own profession, but not necessarily those of other professions.
‘I think a lot of people follow by example rather than by their own reasoning.’ (HCA)
Challenging glove practices
At interview, senior staff demonstrated a willingness to challenge practice in relation to NSG use; however, junior staff explained that they were aware of their place within the work hierarchy and consequently would not want to challenge the behaviour of colleagues.
‘I probably wouldn’t challenge because I would choose my battles. . . and that might be sort of lower down my list of priorities, but I would challenge if I thought they were delivering unsafe practice.’ (RN)
Barrier to hand hygiene compliance
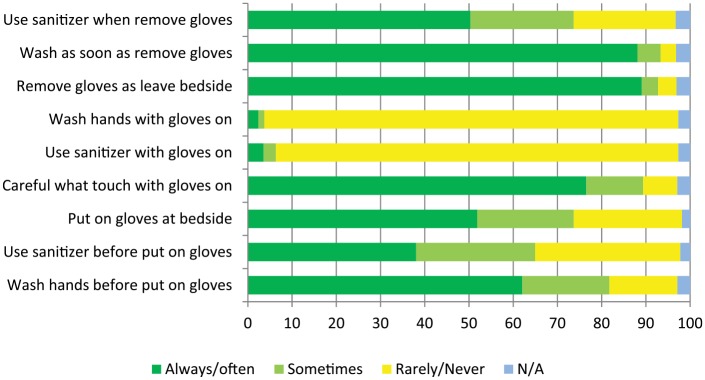
Responses regarding hand hygiene practice in relation to glove use are shown in Figure 2. Only 43% (n = 432) of respondents agreed that they would always wash their hands before putting on NSG, with 23% (n = 232) always using sanitiser before donning gloves. On removal of gloves, 75% (n = 754) stated that they would always wash their hands and 32% (n = 322) would always use sanitiser.
Figure 2.
Responses (%) regarding hand hygiene practice in relation to NSG use (n = 1006).
Many noted during the interviews that they had seen staff wearing gloves as an alternative to hand hygiene. Some observed that hand washing would be better if staff could actually feel something on their hands:
‘If my hands have got contaminated without wearing gloves, I really make sure that I wash my hands, like really well.’ (RN)
An attitude shared was that it was just easier to put on gloves for some tasks:
‘If it’s something really sticky, just to keep your hand cleaner, because it’s much easier to put on a pair of gloves, clean it up, get rid of them and then give your hands a quick wash, rather than having to really scrub if you’ve got something really horrible on them.’ (HCA)
Patient experience
Patient expectations of NSG use appeared to be a less important factor in the decision to wear gloves, with only 16% (n = 163) agreeing that patients prefer them to wear NSG, and 11% (n = 112) agreeing that patients prefer not to have skin-to-skin contact. One-third of respondents agreed that patients feel safer when HCWs wear gloves. Generally, interviewees felt that patients would be reassured to see HCWs wearing gloves, that they were being protected from infection. However, interviewees acknowledged that wearing gloves could give the wrong message, that the patients are ’dirty’ or infectious.
‘I spend a lot of time holding their [patients’] hands, and it can be a bit . . . different if you’re holding their hand within a glove. It’s just less personal.’ (Doctor)
Touch has an important role in communication; it helps to develop rapport and to convey comfort and care, especially for those who are vulnerable.
Discussion
The present study has compiled the largest dataset of all the studies reviewed in the literature, with comprehensive data complemented by qualitative data as part of the questionnaire and separate narrative interviews.
As identified at interview, the principal motivating factor for staff to wear NSG was for personal protection; the secondary motivating factor was to protect patients from cross-infection. Unqualified staff were significantly more likely than qualified staff to use NSG when they were not indicated. Similarly, Walaszek et al. (2018) found that HCWs with lower seniority, including students, attached greater importance to the use of gloves. This suggests a necessity for behavioural change interventions aimed at unqualified staff. The interviewees clearly demonstrated a lack of knowledge regarding the transmission of disease which affected their use of gloves.
However, education alone has its limitations. Herbert et al. (2013) found that 70% of medical students indicated an excellent/good knowledge of hand hygiene guidelines, but only 43% adhered to hand hygiene recommendations. The application of behaviour change paradigms to better translate knowledge into behaviour has been suggested by Sahai et al. (2016).
Staff may not be aware of organisational policy and national guidance, may choose to ignore it and make their own decisions, or policies may lack clarity. Cusini et al. (2015) stated that ‘it is not surprising that gloving can have a negative impact on hand hygiene because it can be time consuming’. The authors eliminated mandatory glove use in the care of patients being nursed with contact precautions and found that the change significantly improved hand hygiene compliance. Organisational policies need to be well-defined about indications for NSG and more accessible to staff. It would be beneficial to review the indications for glove use and amend policy accordingly. This would contribute to the sustainability programme within the NHS.
The principal influences on decision making on when to wear NSG were whether a patient had a known systemic or topical infection. However, staff were also motivated by a desire to create a positive image of professionalism, cleanliness and to protect patients’ dignity. It is important to acknowledge that some motivating factors are not influenced by a lack of knowledge or desire to follow organisational policy.
Interviewees were more likely to follow the lead in their own profession, but not necessarily those in other professions, demonstrating the importance of leadership by all staff groups in influencing practice across an organisation. This was also found by Smiddy et al. (2015) in the systematic qualitative review of hand hygiene; that junior doctors and medical students were influenced by senior medical staff and student nurses were influenced by qualified nursing staff.
Rarely did HCWs feel able to challenge the glove practices of colleagues, senior staff showing more confidence in challenging the behaviours of others. In a study by Ward (2010), nursing and midwifery students were concerned that challenging poor practice could lead to ostracism from the team and provoke a critical clinical report. Hinkin and Cutter (2014) recommended that staff be equipped with the skills to question the behaviour of others in such a way as to minimise the risk of conflict or embarrassment and maintain a positive working environment.
Wilson et al. (2017a) identified a conflation of the concepts of standard precautions and contact precautions, resulting in glove use for all patient contact. The rise of antimicrobial resistance and the risk of multidrug-resistant organisms may be intensifying this perception. Behaviour change in relation to glove use is a complex issue. Behaviour change theories may offer tools for improving glove use and hand hygiene; however, these theories have not been extensively examined (Srigley et al., 2014). Burdsall et al. (2017) have recommended that human factors engineering research and studies that assess healthcare workflow could assist in overcoming the overuse of gloves.
Based on the present study, the authors recommend the development of multi-modal interventions to address glove use behaviour in clinical practice (behaviour change interventions, development of safety climate, visual reminders, use of social marketing and system change), in addition to studies to explore the evidence base for use of PPE and transmission based precautions.
The present study has demonstrated the complex issues associated with the use of NSG for HCWs. If we are to develop a sustainable NHS for the future, the use of NSG needs to be clarified so that guidance and training across organisations is standardised and behaviour is positively changed and maintained.
Limitations
There are a number of limitations to the present study. The sample was a convenience sample and may not be representative of the population. The study was carried out across three healthcare organisations in two counties but may not reflect the picture nationally. The questionnaire asked for participants’ role but did not classify maternity staff separately from other HCWs, so it is not possible to analyse this group separately. An issue with questionnaires exploring attitudes is that participants may give what they think are the ‘correct’ answers, and therefore some of the responses reported may not always fully reflect behaviour on the wards.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a commercial sponsor Industrial Microbiology Services Limited (IMSL), Pale Lane, Hartley Wintney, Hampshire; and research funding from the Infection Prevention Society, London South branch.
The data collection tools (questionnaire and interview script), data and statistical analysis can be accessed from the authors.
Peer review statement: Not commissioned; blind peer-reviewed.
ORCID iD: Ashley Flores  https://orcid.org/0000-0002-4901-8207
https://orcid.org/0000-0002-4901-8207
References
- Boudjema S, Tarantini C, Peretti-Watel P, Brouqui P. (2017) Merging video coaching and an anthropologic approach to understand health care provider behaviour toward hand hygiene protocols. American Journal of Infection Control 45: 487–491. [DOI] [PubMed] [Google Scholar]
- Burdsall DP, Gardner SE, Cox T, Schweitzer M, Culp KR, Steelman VM, Herwaldt LA. (2017) Exploring inappropriate certified nursing assistant glove use in long-term care. American Journal of Infection Control 45: 940–945. [DOI] [PubMed] [Google Scholar]
- Buzan T, Buzan B. (2003) The Mind Map Book. Revised Edition. London: BBC Worldwide Ltd. [Google Scholar]
- Cusini A, Nydegger D, Kaspar T, Schweiger A, Kuhn R, Marschall J. (2015) Improved hand hygiene compliance after eliminating mandatory glove use from contact precautions-Is less more? American Journal of Infection Control 43(9): 922–927. [DOI] [PubMed] [Google Scholar]
- Herbert V, Schlumm P, Kessler H, Frings A. (2013) Knowledge of and Adherence to Hygiene Guidelines among Medical Students in Austria. Interdisciplinary Perspectives on Infectious Diseases 2013: 802930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinkin J, Cutter J. (2014) How do university education and clinical experience influence pre-registration nursing students' infection control practice? A descriptive, cross sectional survey. Nurse Education Today 34(2): 196–201. [DOI] [PubMed] [Google Scholar]
- Jackson C, Griffiths P. (2014) Dirt and disgust as key drivers in nurses’ infection control behaviours: an interpretative, qualitative study. Journal of Hospital Infection 87: 71–76. [DOI] [PubMed] [Google Scholar]
- Kang J, O’Donnell J, Colaianne B, Bircher N, Ren D, Smith K. (2017) Use of personal protective equipment among health care personnel: Results of clinical observations and simulations. American Journal of Infection Control 45: 17–23. [DOI] [PubMed] [Google Scholar]
- Kurtz SL. (2017) Identification of low, high and super gelers and barriers to hand hygiene among intensive care unit nurses. American Journal of Infection Control 45: 839–843. [DOI] [PubMed] [Google Scholar]
- Loveday HP, Wilson JA, Pratt R, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto J, Wilcox M. (2014) epic3: National Evidence-Based Guidelines for Preventing Healthcare-Associated Infections in NHS Hospitals in England. Journal of Hospital Infection 86(Suppl.1): S1–S70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahai V, Eden K, Glustein S, Nesdole R. (2016) Hand hygiene knowledge, attitudes and self-reported behaviour in family medicine residents. Canadian Journal of Infection Control 31(1): 11–17. [Google Scholar]
- Smiddy MP, O’Connell R, Creedon SA. (2015) Systematic qualitative literature review of health care workers' compliance with hand hygiene guidelines. American Journal of Infection Control 43(3): 269–274. [DOI] [PubMed] [Google Scholar]
- Srigley JA, Furness CD, Baker GR, Gardam M. (2014) Quantification of the Hawthorne effect in hand hygiene compliance monitoring using an electronic monitoring system: a retrospective cohort study. BMJ Quality & Safety 23: 974–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wałaszek M, Kołpa M, Różańska A, Wolak Z, Bulanda M, Wójkowska -Mach J. (2018) Practice of hand hygiene and use of protective gloves: Differences in the perception between patients and medical staff. American Journal of Infection Control 46(9): 1074–1076. [DOI] [PubMed] [Google Scholar]
- Ward D. (2010) Infection control in clinical placements: experiences of nursing and midwifery students. Journal of Advanced Nursing 66(7): 1533–1542. [DOI] [PubMed] [Google Scholar]
- Whiting M, Sines D. (2012) Mind maps: establishing ‘trustworthiness’ in qualitative research. Nurse Researcher 20(1): 21–27. [DOI] [PubMed] [Google Scholar]
- Wilson J, Bak A, Loveday H. (2017. a) Applying human factors and ergonomics to the misuse of nonsterile clinical gloves in acute care. American Journal of Infection Control 45: 779–786. [DOI] [PubMed] [Google Scholar]
- Wilson J, Bak A, Whitfield A, Dunnett A, Loveday H. (2017. b) Public perceptions of the use of gloves by healthcare workers and comparison with perceptions of student nurses. Journal of Infection Prevention 18(3): 123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2009) WHO guidelines on hand hygiene in healthcare. Geneva: WHO; Available at: https://www.who.int/gpsc/5may/tools/9789241597906/en/. [Google Scholar]