Abstract
Background:
A femoral head “divot” is a rare finding during hip arthroscopy. A linear chondral indentation can be observed on the femoral head, just lateral and parallel to the acetabular labrum.
Purpose/Hypothesis:
The purpose of this study was to describe a novel arthroscopic sign and retrospectively review patients with this finding. We hypothesized that this sign would be found in patients with characteristics consistent with hip microinstability.
Study Design:
Case series; Level of evidence, 4.
Methods:
Intraoperative images of patients undergoing primary hip arthroscopy between July 2017 and July 2019 were reviewed for evidence of a femoral head divot. Preoperative characteristics, physical examination findings, radiographic measurements, and magnetic resonance imaging (MRI) findings were described.
Results:
Of 690 available cases, 14 cases (13 patients; 2.0%) had evidence of a femoral head divot. The mean patient age was 29.1 years, and all but 1 patient (92.3%) were female. Ligamentous laxity was present in 81.8% of patients, anterior apprehension test was positive in 78.6%, and painful internal snapping was present in 50.0%. The mean lateral center-edge angle, anterior center-edge angle, and Tönnis angle were 19.2°, 20.3°, and 12.4°, respectively. The divot was identified in 5 of 12 available MRI scans, most commonly on axial proton density sequence. Intraoperatively, all hips had labral tears, iliopsoas bursitis was demonstrated in 78.6%, and the ligamentum teres was damaged in 42.9%. Labral repair was performed in 12 of the 14 hips, with 2 patients undergoing labral reconstruction. Iliopsoas fractional lengthening was performed in 50.0%, capsular plication was performed in 78.6%, and capsular repair was performed in the remainder.
Conclusion:
The femoral head divot sign is a rare arthroscopic finding during hip arthroscopy. The results of this study demonstrated that patients who have a divot also present with characteristic radiographic or physical examination findings of hip microinstability due to either acetabular dysplasia or ligamentous laxity. Recognition of a femoral head divot may be valuable for the diagnosis of microinstability during hip arthroscopy and may help guide appropriate management, such as capsular plication. Further studies are needed to determine the exact prevalence of the femoral head divot in patients with microinstability and to evaluate the effect of this finding on patient outcomes.
Keywords: hip arthroscopic surgery, microinstability, femoral head chondral indentation, iliopsoas impingement
Hip microinstability is gaining recognition as a major contributor to hip pain in adults and as a possible risk factor for the development of early arthritis. Traditionally considered an inherently stable joint, the hip may develop microinstability, defined as extraphysiologic motion that is associated with pain, with or without a feeling of instability.24 Possible causes of microinstability can be classified into 1 of 6 categories: (1) bony abnormalities (eg, developmental dysplasia), (2) connective tissue disorders (eg, Ehlers-Danlos), (3) posttraumatic, (4) microtraumatic (eg, labral tears), (5) iatrogenic, and (6) idiopathic.22
The diagnosis of hip microinstability may be challenging, especially when the primary concern is pain without a sensation of joint instability. The most prevalent forms of microinstability are bony abnormalities and ligamentous laxity. However, microinstability may exist in the setting of normal, or near-normal, radiographic imaging or in a patient without a history of a connective tissue disorder. To our knowledge, no diagnostic tests or physical examination findings are pathognomonic with hip microinstability.22
We have identified an arthroscopic finding of a linear chondral or osteochondral indentation on the anterior surface of the femoral head, running roughly in parallel with the acetabular rim and labrum. This indentation appears on the femoral head, just lateral to the labrum, with the hip in flexion and neutral rotation. Upon flexion and rotation of the hip joint, the divot can be seen entering under the labrum and into the functional joint.
The purpose of this study was to (1) retrospectively identify this finding in patients undergoing primary hip arthroscopy, (2) provide a description of the patients in whom the finding was identified, and (3) attempt to identify the indentation on preoperative magnetic resonance imaging (MRI) scans. Our hypothesis was that patients demonstrating this indentation would also exhibit characteristic signs of microinstability.
Methods
Patient Selection
After institutional review board approval, a retrospective review of the institutional hip preservation registry was performed. Patients who underwent primary arthroscopic hip surgery by the senior author (B.G.D.) between July 2017 and July 2019 were identified. Exclusion criteria included a history of avascular necrosis, slipped capital femoral epiphysis, Legg-Calvé-Perthes disease, or rheumatologic conditions and unwillingness to participate in the institutional research database. Intraoperative arthroscopic photographs were reviewed for all eligible patients for evidence of a femoral head divot. Patients in whom a characteristic femoral head divot could be clearly identified were included in the final series. Patients with a divot were compared with a historical cohort of patients who underwent primary hip arthroscopy between April 2010 and October 2016. Patients were not included in this cohort if they had previous hip conditions.
Data Collection
Demographic data as well as preoperative physical examination findings were retrieved from the surgical database. Demographic information included sex; age at time of surgery; and preoperative height, weight, and body mass index (BMI). Preoperative physical examination findings included presence of antalgic gait, generalized ligamentous laxity as graded by the Beighton score,3 hip range of motion (flexion, internal rotation, external rotation, and abduction), presence of anterior or lateral impingement signs, presence of positive anterior or posterior apprehension test, presence of a painful internal snapping, and ligamentum teres test.16
Arthroscopic Evaluation and Surgical Technique
Each operation was performed by the senior author. Patients were positioned on a traction table in a modified supine position. Standard anterolateral and midanterior accessory portals were used to access the joint and perform the diagnostic portion of the procedure, and an interportal capsulotomy was completed. Additional portals were added as necessary to complete other portions of the operation. A diagnostic arthroscopy was performed, and several intraoperative findings were routinely photographed and recorded: labral condition (Seldes type) and width, acetabular labrum articular disruption (ALAD) grade, chondral damage (Outerbridge score), ligamentum teres condition, presence of iliopsoas bursitis indicated by inflamed tissue, and presence of an iliopsoas impingement lesion.5 After the diagnostic portion of the operation, any indicated procedures were performed. The capsule was elevated from the labrum through use of electrocautery. A 5.5-mm round bur was used to address any bony abnormalities as indicated by preoperative and fluoroscopic imaging. Debridement of the ligamentum teres was performed if tears were evident. Patients who had painful internal snapping preoperatively underwent iliopsoas fractional lengthening using the method described by El Bitar et al9; special care was taken to preserve the capsule for subsequent closure or plication and to avoid extending into the muscle belly. Full-thickness chondral lesions of either the acetabulum or the femoral head were treated using microfracture. Labral repair or reconstruction was performed by use of previously described techniques.18,25 Because all patients had risk factors for microinstability, all capsules were closed, whereas plication of the capsule was performed based on clinical evaluation of hyperlaxity as previously described.6
Radiographic and MRI Analysis
For patients with the identified divot sign, preoperative radiographs and MRI scans were evaluated by 2 independent orthopaedic surgeons (P.J.R. and B.C.M.). Any disagreements in findings were deferred to the senior author for final determination. Standing and supine anteroposterior pelvic radiographs, as well as false-profile, modified 45° Dunn, and cross-table lateral images of the pathologic hip, were performed on all patients as is standard protocol at our institution. Multiple radiographic characteristics and measurements were recorded, including Tönnis grade, joint space at 3 points along the acetabular sourcil, anterior center-edge angle (ACEA), lateral center-edge angle (LCEA), acetabular index (Tönnis angle), neck shaft angle, alpha angle, coxa profunda, and cliff sign, as described by Packer et al.17 Additionally, each patient underwent MRI of the pathologic hip before surgery, and the MRI scan was retrospectively reviewed for evidence of the femoral divot.
Statistical Analysis
Statistical analysis was performed by use of Stata/MP 13.1 for Mac (StataCorp LP). Categorical variables were presented as percentages, whereas means and standard deviations were calculated for continuous variables. Continuous variables were assessed for normality and variance using the Shapiro-Wilk test and F test respectively. A Student’s t-test or a nonparametric equivalent was then used to analyze the data. Categorical variables were examined using a Chi-squared or Fisher’s exact test. A P value of < 0.05 was considered significant.
Results
Preoperative Characteristics
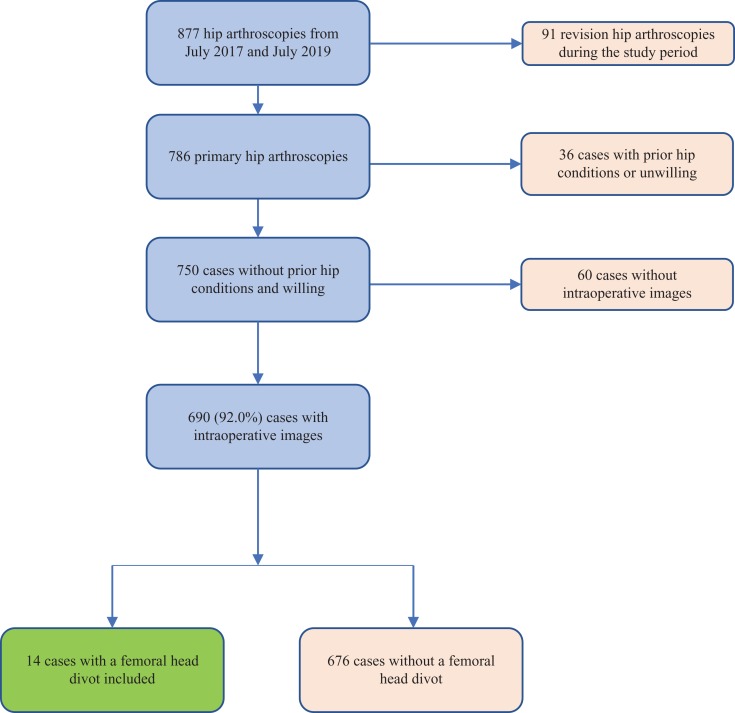
The femoral head divot sign was identified in a total of 14 hips (13 patients) out of 690 available cases of hip arthroscopy (2%) (Figure 1).
Figure 1.
Flowchart depicting patient selection.
For the patients with a femoral head divot, the average age was 29.1 years, and nearly all (92.3%) were female. Compared with the historical cohort, the femoral head divot group was significantly younger and had a higher proportion of female patients (P = .0319 and P < .0001, respectively). The mean BMI was 25.0 (Table 1). On physical examination, a majority (76.9%) of patients had no gait disturbance, whereas the others had an antalgic gait. Generalized ligamentous laxity (Beighton score ≥4) was present in 81.8% (n = 9/11) of patients. Signs of anterior and lateral impingement were present in 92.9% and 64.29% of hips, respectively. Positive anterior apprehension test was reported in 78.6% of hips. Range of motion measurements can be found in Table 2. Internal snapping was present in 50.0% of hips. The ligamentum teres test was positive in 2 hips (16.7%). Tönnis grade 0 was found in 12 cases (85.7%); Tönnis grade 1 in the remaining 2 cases (Table 3). Radiographic measurements of dysplasia demonstrated a mean LCEA of 19.2° ± 5.5° and ACEA of 20.3° ± 5.1°. Mean Tönnis angle was 12.4° ± 4.8° (Table 4). When compared with the historical cohort, the femoral head divot group demonstrated significantly lower values for LCEA and ACEA and a higher value for Tönnis angle.
Table 1.
Summary of Descriptive Dataa
| Femoral Head Divot Cohort (n = 13b) | Historical Cohort (n = 1796) | P Value | |
|---|---|---|---|
| Age, y | 29.1 ± 13.3 | 36.8 ± 14.4 | .0319 |
| Sex | <.0001 | ||
| Female | 92.3 (12) | 63.9 (1148) | |
| Male | 7.7 (1) | 36.1 (648) | |
| Laterality | .9510 | ||
| Right | 50.0 (7) | 52.7 (947) | |
| Left | 50.0 (7) | 47.3 (849) | |
| Body mass index, kg/m2 | 25.0 ± 4.0 | 26.1 ± 5.3 | .4545 |
aResults are presented as percentage (n) or mean ± SD.
bOne patient presented with a bilateral finding of a femoral head divot.
Table 2.
Physical Examination Findings in Cases of Femoral Head Divota
| Physical Examination Finding | |
|---|---|
| Gait | |
| Normal | 76.9 (10) |
| Antalgic | 23.1 (3) |
| Beighton scoreb | |
| 0 | 18.2 (2) |
| 4 | 27.3 (3) |
| 6 | 45.5 (5) |
| 8 | 9.0 (1) |
| Range of motion, deg | |
| Hip flexion | 118 ± 13 |
| Internal rotation | 32 ± 14 |
| External rotation | 47 ± 18 |
| Abduction | 38 ± 9 |
| Impingement sign | |
| Anterior | 92.9 (13) |
| Lateral | 64.3 (9) |
| Apprehension sign | |
| Anterior apprehension test | 78.6 (11) |
| Posterior apprehension test | 0.0 (0) |
| Painful internal snapping | 50.0 (7) |
| Ligamentum teres testb | 16.7 (2) |
aResults are presented as percentage (n) or mean ± SD. N = 14 cases (13 patients). Findings without a laterality are reported by patient and not by hip.
bTwo patients did not have complete physical examination data recorded for the indicated tests.
Table 3.
Radiographic Measurementsa
| Femoral Head Divot Cohort (n = 14) | Historical Cohort (n = 1796) | P Value | |
|---|---|---|---|
| Tönnis grade | >.9999 | ||
| 0 | 85.7 (12) | 84.9 (1525) | |
| 1 | 14.3 (2) | 15.1 (271) | |
| Average joint space, mm | 4.6 ± 0.6 | 4.3 ± 0.1 | .0008 |
| Neck shaft angle, deg | 130.4 ± 7.3 | 133.3 ± 6.4 | .0198 |
| Alpha angle, deg | 57.9 ± 9.7 | 60.0 ± 21.8 | .9747 |
| Coxa profunda | 28.6 (4) | 23.4 (421) | .8930 |
| LCEA, deg | 19.2 ± 5.5 | 30.5 ± 6.4 | <.0001 |
| ACEA, deg | 20.3 ± 5.1 | 31.3 ± 7.4 | <.0001 |
| Tönnis angle, deg | 12.4 ± 4.8 | 5.0 ± 4.7 | <.0001 |
aResults are presented as percentage (n) or mean ± SD. ACEA, anterior center-edge angle; LCEA, lateral center-edge angle.
Table 4.
Radiographic Measurements of Dysplasiaa
| Case No. | LCEA, deg | ACEA, deg | Tönnis Angle, deg | Cliff Sign | Upsloping Lateral Sourcil |
|---|---|---|---|---|---|
| 1b | 8 | 19 | 22 | No | Yes |
| 2 | 22 | 22 | 12 | Yes | Yes |
| 3 | 21 | 15 | 11 | No | Yes |
| 4 | 26 | 23 | 8 | Yes | No |
| 5 | 24 | 24 | 4 | Yes | Yes |
| 6 | 18 | 17.5 | 10 | Yes | Yes |
| 7 | 22 | 25 | 9.5 | Yes | No |
| 8 | 19 | 15.7 | 10.2 | Yes | Yes |
| 9 | 16 | 18 | 8.3 | Yes | Yes |
| 10b | 8 | 14 | 18 | No | Yes |
| 11 | 21 | 33 | 15 | No | Yes |
| 12 | 26 | 21 | 14 | Yes | Yes |
| 13 | 19 | 15 | 14.2 | Yes | Yes |
| 14 | 19 | 22 | 18 | Yes | Yes |
| Mean ± SD or n/N (%) | 19.2 ± 5.5 | 20.3 ± 5.1 | 12.4 ± 4.8 | 10/14 (71.4) | 12/14 (85.7) |
aACEA, anterior center-edge angle; LCEA, lateral center-edge angle.
bPatients who underwent concomitant periacetabular osteotomy and arthroscopy.
Intraoperative Findings and Procedures
All hips had labral tears evident during surgery, and 50% had an ALAD grade of 2. The Outerbridge score for acetabular chondral damage was grade 2 in 50.0% of hips and grade 1 in 28.6%. There were 2 hips that demonstrated femoral head chondral damage (14.3%), located at the apex of the femoral head and distinct from the femoral divot. The ligamentum teres was damaged in 42.9% of hips. Iliopsoas bursitis was noted in 78.5% of hips, with an iliopsoas impingement lesion present in 21.4%. Complete intraoperative findings can be found in Table 5.
Table 5.
Summary of Intraoperative Findingsa
| Intraoperative Finding | |
|---|---|
| Labral tear | |
| Seldes 1 | 28.6 (4) |
| Seldes 2 | 21.4 (3) |
| Combined | 50.0 (7) |
| Labral width, mmb | 5.0 ± 1.0 |
| Acetabular labrum cartilage disruption | |
| Grade 0 | 21.4 (3) |
| Grade 1 | 28.6 (4) |
| Grade 2 | 50.0 (7) |
| Outerbridge score | |
| Acetabular | |
| Grade 0 | 21.4 (3) |
| Grade 1 | 28.6 (4) |
| Grade 2 | 50.0 (7) |
| Femoralc | |
| Grade 0 | 85.7 (12) |
| Grade 3 | 7.1 (1) |
| Grade 4 | 7.1 (1) |
| Ligamentum teres tear | 42.9 (6) |
| Iliopsoas bursitis | 78.6 (11) |
| Iliopsoas impingement lesion | 21.4 (3) |
aResults are presented as percentage (n) or mean ± SD. N = 14 cases (13 patients).
bOne patient had missing labral width data.
cThe femoral head damage in these patients was apical and distinct from the femoral divot.
Labral repair was performed in 12 of the 14 hips, with the other 2 hips undergoing labral reconstruction. Capsular repair was completed in all cases, with an additional plication performed in 78.6% of hips. Iliopsoas fractional lengthening was performed in the hips of patients who presented with painful internal snapping (50.0%). The remainder of surgical procedure data are reported in Table 6.
Table 6.
Procedures Performeda
| Procedure | |
|---|---|
| Labral treatment | |
| Repair | 85.7 (12) |
| Reconstruction | 14.3 (2) |
| Capsular treatment | |
| Repair only | 21.4 (3) |
| Repair and plication | 78.6 (11) |
| No. of sutures used | 3.6 ± 1.1 |
| Femoroplasty | 100.0 (14) |
| Microfracture | |
| Acetabulum | 14.3 (2) |
| Femoral | 7.1 (1) |
| Ligamentum teres debridement | 28.6 (4) |
| Iliopsoas fractional lengthening | 50.0 (7) |
aResults are presented as percentage (n) or mean ± SD. N = 14 cases (13 patients).
Femoral Divot Characteristics
During the diagnostic arthroscopy, the divot was best observed from the anterolateral viewing portal while the arthroscope was aimed toward the anterior portion of the femoral head. The typical presentation of the divot was a smooth, linear, chondral or osteochondral groove or indentation (Figure 2).
Figure 2.
Characteristic appearance of femoral head divot. The arthroscopic viewing portal is the anterolateral portal. After release of traction, upon reduction of the femoral head, with the hip in 60° of flexion and neutral rotation, the indentation (red arrow) is seen lateral and parallel to the acetabular rim.
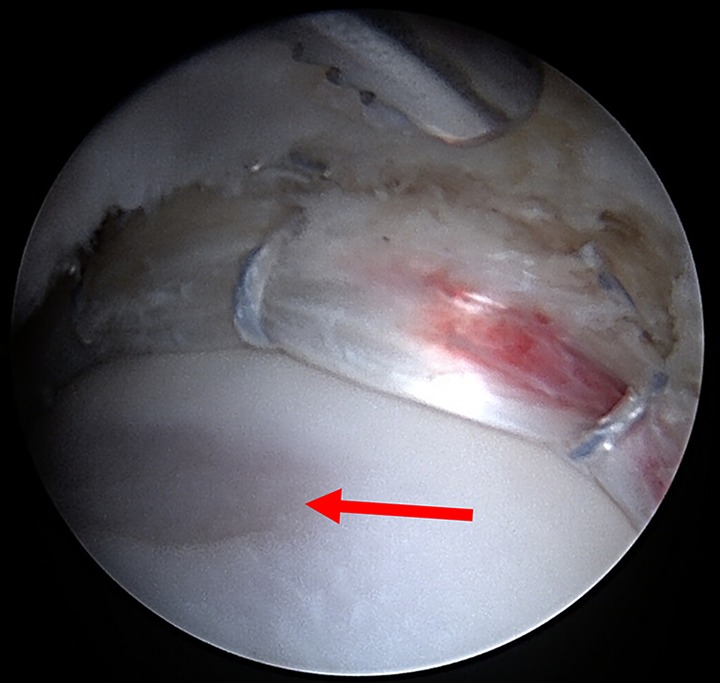
Upon flexion of the leg in neutral rotation, the groove was oriented approximately parallel to the acetabular rim and just lateral to the labrum on the anterior aspect of the femoral head (Figure 2). During rotation of the hip, it was observed that the divot could enter the hip joint by passing underneath the labrum and creating a break in the continuity of the labral-femoral head suction seal (Figure 3). During this maneuver, we have occasionally observed synovial fluid extravasating from within the joint as the indentation disrupts the suction seal of the labrum.
Figure 3.

The divot (red arrow) is seen passing under the repaired labrum when the hip is flexed and rotated.
Some variability was noted in the appearance of the indentation seen intraoperatively. We found that 2 of the divots had a more degenerative appearance with noted chondral fraying and damage (Figure 4).
Figure 4.

Degenerative appearance of the divot with irregularity of the overlying cartilage (red arrow).
The femoral head divot was identifiable on 5 of the 12 available MRI scans, findings were equivocal on 4 scans, and the femoral head divot was not seen in the remaining 3 scans. The divot was best seen on the axial cut of proton density–weighted MRI sequences. When seen, the divot was identified on the anterior surface of the femoral head on axial views. It was identifiable as either a flattening of the head sphericity or concavity, often with a small area of hyperintensity of the cartilage or underlying bone (Figures 5 and 6).
Figure 5.

Characteristic appearance of the divot on preoperative magnetic resonance imaging scan. These paraxial proton density sequences depict (A) concave deformation or (B) flattening of the anterior femoral head (red arrows).
Figure 6.

Appearance on T2-weighted magnetic resonance imaging sequences. When viewed on paraxial T2-weighted sequence, red arrows in panels (A) and (B) indicate the location of the divot.
Discussion
In this study we have described the femoral head divot sign as an arthroscopically observed indentation of the femoral head chondral surface. The divot is identified as a linear chondral indentation running parallel and lateral to the acetabulum when the hip is in approximately 60° of flexion and neutral rotation. The divot sign was observed in 2.0% of primary hip arthroscopies (14/690). All patients in whom the sign was observed had characteristic clinical or radiographic findings of hip microinstability, such as increased Beighton score or decreased LCEA angles.
Microinstability has gained recognition as an important cause of pain and disability in the adult hip. Microinstability has been classified based on bony or soft tissue origin, with 2 of the most common causes being acetabular undercoverage and ligamentous laxity.10,14 Signs of microinstability on physical examination were extremely prevalent in this patient series. A positive anterior apprehension test was noted in 78.6% of hips (11/14), and 81.8% of patients (9/11) presented with a Beighton score of 4 or higher. A recent study reported a Beighton score of 4 or higher in only 18.9% of patients undergoing hip arthroscopy, significantly less common than the demonstrated rate in the current study.21
Additionally, 13 of the 14 hips in our study were in female patients. Ligamentous laxity has been reported as being significantly more common in women.19,21 As such, it is intuitive that women are at higher risk of microinstability given that laxity is a predominant risk factor for microinstability.6,21 The only male patient in this cohort had an extreme case of hip dysplasia and femoral anteversion and underwent hip arthroscopy with concomitant periacetabular osteotomy (PAO).
Iliopsoas abnormality, such as bursitis and associated painful internal snapping, was also a common finding in this population, with 50% of hips undergoing iliopsoas fractional lengthening to treat painful internal snapping. The prevalence of iliopsoas abnormality has been shown to be particularly high in young female patients undergoing hip arthroscopy, especially when ligamentous laxity is present.13,15,20,21 Several authors have raised concerns for induced microinstability, and even frank dislocation, after iliopsoas fractional lengthening.2,8,11,23 The major concern for instability after iliopsoas procedures is based on 3 cases of dislocations after iliopsoas tenotomy in which other concurrent procedures were performed, such as labral debridement.1,8,23 However, there is a paucity of data on the role of the iliopsoas muscle and tendon in hip stabilization. One cadaveric, biomechanical study demonstrated that the primary role of the iliopsoas changed with varying degrees of hip flexion. Through the first 15° of hip flexion, the iliopsoas acted as a stabilizer of the femoral head. However, during flexion beyond 15°, the more dominant role of the iliopsoas was as a lumbar spine erector and hip flexor.28 Hartigan et al12 reported on 32 patients with borderline acetabular dysplasia undergoing iliopsoas fractional lengthening and showed significant improvements in patient-reported outcomes and high patient satisfaction. Additionally, no patients experienced a dislocation at the minimum 2-year follow-up.
Radiographic findings suggesting hip instability have previously been described. In this study, the average LCEA was 19.2°, with 12 of the 14 hips exhibiting dysplasia or borderline dysplasia. Anterior undercoverage can be assessed by using the ACEA, with angles <20° suggesting instability. In this cohort, the average ACEA was 20.3°, with 7 of 14 (50%) hips having ACEAs <20°. Further, 6 of the remaining 7 hips had ACEAs ≤25°, placing them in the low range of normal. The upsloping lateral sourcil (ULS) is a radiographic sign in which the lateral aspect of the sourcil assumes a cranial inclination with loss of the normal lateral acetabular concavity. The ULS has previously been associated with ligamentous laxity as well as hip dysplasia defined by a smaller LCEA.27 In this patient series, the ULS was found in 85.7% of hips. Another radiographic sign of instability is the cliff sign, in which a steep drop-off on the lateral edge of the femoral head can be observed on an anteroposterior radiograph. In the present study’s cohort, the cliff sign was present in 71% of hips. Previous literature has reported the cliff sign in 89% of patients with microinstability compared with only 27% of patients without microinstability.17 The radiographic findings in our patient series supported the hypothesis that dysplasia-induced microinstability would be a dominant cause for formation of the divot.
The retrospective nature of this study limited the ability to determine the exact pathogenesis of the femoral head divot. However, we propose a number of possible explanations for its formation.
One possibility is that in patients with microinstability, the femoral head subluxates from the acetabular socket and impinges on the acetabular rim at this location. This repetitive edge loading may lead to deformation of the femoral head over time. In 1 of the cases presented, the divot was especially prominent in a patient with severe dysplasia and femoral anteversion, and on MRI scan the divot could be seen engaging the acetabular rim (Figure 7). This patient as well as 1 other patient underwent a concomitant PAO and hip arthroscopy. Previous biomechanical studies have shown reduction in contact stresses of the hip joint in patients undergoing PAO and transfer of the load to more medial areas of the acetabulum and femoral head.26,30 The reduced loads laterally as well as the change in the orientation of the acetabulum likely reduce the continued engagement and edge-loading of the divot lesion.
Figure 7.

Magnetic resonance imaging scan of a patient with a large osteochondral femoral divot. The femoral indentation can be seen engaging the acetabular rim (red arrow).
Another possible explanation is that in patients with anterior undercoverage, the iliopsoas tendon causes abrasion of the femoral head as it traverses down to the lesser trochanter. Although the iliopsoas may be a minor stabilizer of the normal hip joint, it has been postulated that in cases of microinstability, the iliopsoas tendon assumes a pathological hyperactivity. This increased strain on the iliopsoas may lead to impingement, pain, and snapping, which could further damage the underlying structures, such as the anterior labrum (ie, labral impingement sign). It is possible that this same mechanism of shear stress by the iliopsoas tendon may be a cause for the observed femoral head divot. This may be particularly true in patients with anterior undercoverage, who have fewer acetabular bony and labral anatomic features to shield the femoral head from repetitive forces from the iliopsoas that could over time result in a divot. In our cohort, 50% of hips had painful internal snapping, which may attest to the plausibility of this etiological factor.
A similar mechanism has been proposed for a finding of a chondral divot in the humeral head. Castagna et al4 described a chondral print sign on the humeral head as a similar finding of a linear imprint on the humeral head cartilage. The authors postulated that this is due to biceps instability and that its finding can assist in confirming equivocal cases, although other studies have not found an association of this sign with biceps abnormality.7 In contrast to the femoral head divot sign, the chondral print sign in the shoulder has a higher reported prevalence, with 1 study noting a prevalence of nearly 25% in patients undergoing shoulder arthroscopy. We found the femoral head divot sign to be relatively rare, with a prevalence of 2%, although this may have been an underestimate of the true prevalence. The iliopsoas is a more robust structure than the biceps tendon and is not reliant on other structures, such as the subscapularis tendon and glenoid labrum, for stability, which may be a contributing factor to the lower incidence of the femoral divot.
Another possible cause of the femoral head divot is indentation due to a displaced labral flap causing chronic pressure on the cartilage. A similar mechanism was proposed to describe the “wave sign,” a chondral injury to the medial femoral condyle that is seen in association with occult longitudinal peripheral meniscal tears of the posterior horn. The meniscus was believed to displace anteriorly and cause the injury to the cartilage.29
The presence of a femoral head divot has some potential clinical implications. First, it can corroborate a clinical diagnosis of hip microinstability and can aid in treatment decisions, such as capsular plication. Because this study was retrospective and the divot was not initially identified as a clear indicator of microinstability, 3 of the hips (21.4%) underwent capsular closure without plication. Second, the incongruency of the femoral head may have a detrimental effect on the suction seal of the joint. As the divot passes the labrum, synovial fluid may escape the joint, further inducing microinstability. This continued instability may limit patient improvement despite appropriate treatment of other conditions, such as labral tearing or bony deformity. Future research is warranted to evaluate whether tightening of the ligamentous stabilizers in these patients is sufficient to reduce symptoms of instability or whether further procedures that directly address the lesion, such as osteochondral implantation, are required.
This study has several limitations. Although we believe the divot to be specific for microinstability, it is not a sensitive sign, and most patients with microinstability do not exhibit this sign. However, although we identified only 14 cases, this may still be an underrepresentation of the true prevalence given the retrospective nature of the study. We retrospectively reviewed operative images and therefore were limited to the views recorded during surgery. Because this sign was not prospectively identified, we have only recently begun consistently evaluating for its presence, and some patients with the divot may have not been detected. Additionally, images were missing for nearly 10% of patients undergoing surgery during this time period. Some MRI procedures were performed at outside facilities, without consistent imaging protocols, and therefore not all of the images were of sufficient quality to identify the divot. Additionally, because the femoral divot is relatively small, it may be missed on MRI due to the thickness of each slice. Last, this study entailed patients who underwent surgery within the past 2 years, and therefore the study did not include an outcome analysis. Future studies should be performed to assess the clinical importance of this finding.
Conclusion
The femoral head divot sign is a rare arthroscopic finding during hip arthroscopy. The results of this study demonstrated that patients who have a divot also present with characteristic radiographic or physical examination findings of hip microinstability due to either acetabular dysplasia or ligamentous laxity. Recognition of a femoral head divot may be valuable for the diagnosis of microinstability during hip arthroscopy and may help guide appropriate management, such as capsular plication. Further studies are needed to determine the exact prevalence of the femoral head divot in patients with microinstability and to evaluate the effect of this finding on patient outcomes.
Footnotes
Final revision submitted January 6, 2020; accepted January 22, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.J.R. has received hospitality payments from Arthrex, Stryker, and Smith & Nephew. J.S. has received hospitality payments from Arthrex, Stryker, and Smith & Nephew. D.R.M. has received hospitality payments from Arthrex, Stryker, and Smith & Nephew. M.B.M. has received educational support and hospitality payments from Arthrex, Stryker, and Smith & Nephew. A.C.L. reports educational support from Medwest and Smith & Nephew; research support from Arthrex, Stryker, and Medacta; food and beverage from Smith & Nephew, Stryker, Zimmer Biomet, Arthrex; travel and lodging from Stryker and Arthrex; and consulting fees from Arthrex and Graymont Medical. B.G.D. has had ownership interests in Hinsdale Orthopaedics, the American Hip Institute, SCD#3, North Shore Surgical Suites, and Munster Specialty Surgery Center; has received research support from Arthrex, ATI, the Kauffman Foundation, Stryker, and Pacira Pharmaceuticals; has received consulting fees from Adventist Hinsdale Hospital, Arthrex, MAKO Surgical, Medacta, Pacira Pharmaceuticals, and Stryker; has received educational support from Arthrex, Breg, and Medwest; has received speaking fees from Arthrex and Pacira Pharmaceuticals; and receives royalties from Arthrex, DJO Global, MAKO Surgical, Stryker, and Orthomerica. The American Hip Institute Research Foundation funded this research and is where our study was performed. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Advocate Health Care Institutional Review Board (ref No. 5276).
References
- 1. Austin DC, Horneff JG, Kelly JD. Anterior hip dislocation 5 months after hip arthroscopy. Arthroscopy. 2014;30(10):1380–1382. [DOI] [PubMed] [Google Scholar]
- 2. Barlow B. Iliopsoas fractional lengthening: treating a disease or a symptom? Editorial commentary Arthroscopy. 2019;35(5):1441–1444. [DOI] [PubMed] [Google Scholar]
- 3. Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Castagna A, Mouhsine E, Conti M, et al. Chondral print on humeral head: an indirect sign of long head biceps tendon instability. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):645–648. [DOI] [PubMed] [Google Scholar]
- 5. Chandrasekaran S, Close MR, Walsh JP, et al. Arthroscopic technique for iliopsoas fractional lengthening for symptomatic internal snapping of the hip, iliopsoas impingement lesion, or both. Arthrosc Tech. 2018;7(9):e915–e919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162–173. [DOI] [PubMed] [Google Scholar]
- 7. Domos P, Neogi DS, Longo UG, Ahrens PM. The chondral print sign: what does it really mean? J Shoulder Elbow Surg. 2017;26(6):e188–e192. [DOI] [PubMed] [Google Scholar]
- 8. Duplantier NL, McCulloch PC, Nho SJ, Mather RC, Lewis BD, Harris JD. Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthroscopy. 2016;32(7):1428–1434. [DOI] [PubMed] [Google Scholar]
- 9. El Bitar YF, Stake CE, Dunne KF, Botser IB, Domb BG. Arthroscopic iliopsoas fractional lengthening for internal snapping of the hip: clinical outcomes with a minimum 2-year follow-up. Am J Sports Med. 2014;42(7):1696–1703. [DOI] [PubMed] [Google Scholar]
- 10. Han S, Alexander JW, Thomas VS, et al. Does capsular laxity lead to microinstability of the native hip? Am J Sports Med. 2018;46(6):1315–1323. [DOI] [PubMed] [Google Scholar]
- 11. Harris JD. Caveat flexor—to release or not to release the iliopsoas, that is the question. Editorial commentary Arthroscopy. 2018;34(6):1851–1855. [DOI] [PubMed] [Google Scholar]
- 12. Hartigan DE, Perets I, Close MR, et al. Arthroscopic treatment of iliopsoas snapping in patients with radiographic acetabular dysplasia using iliopsoas fractional lengthening and capsular plication. Arthroscopy. 2018;34(6):1841–1850. [DOI] [PubMed] [Google Scholar]
- 13. Khan M, Adamich J, Simunovic N, Philippon MJ, Bhandari M, Ayeni OR. Surgical management of internal snapping hip syndrome: a systematic review evaluating open and arthroscopic approaches. Arthroscopy. 2013;29(5):942–948. [DOI] [PubMed] [Google Scholar]
- 14. Kraeutler MJ, Garabekyan T, Pascual-Garrido C, Mei-Dan O. Hip instability: a review of hip dysplasia and other contributing factors. Muscles Ligaments Tendons J. 2016;6(3):343–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Maldonado DR, Krych AJ, Levy BA, Hartigan DE, Laseter JR, Domb BG. Does iliopsoas lengthening adversely affect clinical outcomes after hip arthroscopy? A multicenter comparative study. Am J Sports Med. 2018;46(11):2624–2631. [DOI] [PubMed] [Google Scholar]
- 16. O’Donnell J, Economopoulos K, Singh P, Bates D, Pritchard M. The ligamentum teres test: a novel and effective test in diagnosing tears of the ligamentum teres. Am J Sports Med. 2014;42(1):138–143. [DOI] [PubMed] [Google Scholar]
- 17. Packer JD, Cowan JB, Rebolledo BJ, et al. The cliff sign: a new radiographic sign of hip instability. Orthop J Sports Med. 2018;6(11):2325967118807176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perets I, Hartigan DE, Chaharbakhshi EO, Walsh JP, Close MR, Domb BG. Circumferential labral reconstruction using the knotless pull-through technique-surgical technique. Arthrosc Tech. 2017;6(3):e695–e698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Quatman CE, Ford KR, Myer GD, Paterno MV, Hewett TE. The effects of gender and maturational status on generalized joint laxity in young athletes. J Sci Med Sport Sports Med Aust. 2008;11(3):257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rankin AT, Bleakley CM, Cullen M. Hip joint pathology as a leading cause of groin pain in the sporting population: a 6-year review of 894 cases. Am J Sports Med. 2015;43(7):1698–1703. [DOI] [PubMed] [Google Scholar]
- 21. Saadat AA, Lall AC, Battaglia MR, Mohr MR, Maldonado DR, Domb BG. Prevalence of generalized ligamentous laxity in patients undergoing hip arthroscopy: a prospective study of patients’ clinical presentation, physical examination, intraoperative findings, and surgical procedures. Am J Sports Med. 2019;47(4):885–893. [DOI] [PubMed] [Google Scholar]
- 22. Safran MR. Microinstability of the hip—gaining acceptance. J Am Acad Orthop Surg. 2019;27(1):12–22. [DOI] [PubMed] [Google Scholar]
- 23. Sansone M, Ahldén M, Jónasson P, Swärd L, Eriksson T, Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):420–423. [DOI] [PubMed] [Google Scholar]
- 24. Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30(2):349–367. [DOI] [PubMed] [Google Scholar]
- 25. Suarez-Ahedo C, Martin TJ, Walsh JP, Chandrasekaran S, Lodhia P, Domb BG. Anatomic labral repair in the hip using a knotless tensionable suture anchor. Arthrosc Tech. 2016;5(5):e1089–e1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thomas-Aitken HD, Willey MC, Goetz JE. Joint contact stresses calculated for acetabular dysplasia patients using discrete element analysis are significantly influenced by the applied gait pattern. J Biomech. 2018;79:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wong TY, Jesse MK, Jensen A, Kraeutler MJ, Coleman C, Mei-Dan O. Upsloping lateral sourcil: a radiographic finding of hip instability. J Hip Preserv Surg. 2018;5(4):435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yoshio M, Murakami G, Sato T, Sato S, Noriyasu S. The function of the psoas major muscle: passive kinetics and morphological studies using donated cadavers. J Orthop Sci. 2002;7(2):199–207. [DOI] [PubMed] [Google Scholar]
- 29. Zhang X, You T, Jiang X, Zhang H, Zhang W. Characteristic arthroscopic signs of cartilage injuries indicating concomitant occult medial meniscal peripheral tears of posterior horn. Int Orthop. 2016;40(1):191–195. [DOI] [PubMed] [Google Scholar]
- 30. Zhao X, Chosa E, Totoribe K, Deng G. Effect of periacetabular osteotomy for acetabular dysplasia clarified by three-dimensional finite element analysis. J Orthop Sci. 2010;15(5):632–640. [DOI] [PubMed] [Google Scholar]