Abstract
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)-related infection has a major impact on public health, and healthcare workers (HCWs) are exposed to high biological risk. This paper describes the prevention procedures introduced at the University Hospital of Bari, Italy to reduce the risk to HCWs, consisting of enhanced preventive measures and activation of a report system to collect HCWs' contacts. Twenty-three confirmed cases of infection (0.4% of all HCWs) were reported in the 30-day observation period following implementation of the protocol. This shows that correct management of HCWs' contacts is essential to avoid nosocomial clusters.
Keywords: SARS-CoV-2, Severe acute respiratory infections, Operating procedure, Report system, COVID-19, Healthcare workers
Introduction
The World Health Organization (WHO) has stated that severe acute respiratory infections (SARIs) are acute respiratory infections associated with fever (>38°C), onset of cough (or re-exacerbation in patients with chronic obstructive pulmonary disease) and other pulmonary symptoms that start within 10 days before hospital admission [1].
Sometimes, SARIs can become a public health emergency; this happens when a pathogen (frequently a virus) gains high virulence, spreading through populations in many countries on different continents (pandemic). Throughout history, influenza A viruses, belonging to the Orthomyxoviridae family, have caused pandemics. However, in recent times, retroviruses belonging to the Coronavirinae family have also been shown to cause SARI outbreaks due to their affinity for the lower respiratory tract epithelium receptors. In 2002–2003, severe acute respiratory syndrome coronavirus (SARS-CoV) infected 8096 people and caused 774 deaths, while Middle East respiratory syndrome (MERS-CoV) has infected 2494 people and caused 858 deaths since 2012 [2]. Recently, on 9th January 2020, the Chinese Centres for Disease Control identified a novel coronavirus – severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) – and on 3rd March 2020, WHO declared a pandemic. Multiple infection routes (via the respiratory route, contact with fomites and, probably, faecal-oral) and high contagiousness [3] (highest estimated R0 = 4.6) seem to be essential factors for this global outbreak.
To date, over two-thirds of Italian cases of SARS-CoV-2 have been grouped in four northern regions. Climatic factors and particulate matter levels may play a role in promoting viral spread. Indeed, particulate matter is known to be able to transfer small pathogens from the upper to the lower respiratory tract [4].
Due to the high contagiousness of SARS-CoV-2, healthcare professionals are occupationally exposed to high biological risk. However, Cheng et al. [5] demonstrated that correct use of personal protective equipment (PPE) by healthcare workers (HCWs) in hospitals in Hong Kong was associated with no cases of infection over a 42-day observation period.
This paper will describe the preventive protocol for SARS-CoV-2-related infection adopted by the Operative Unit of Occupational Medicine for HCWs at the University Hospital of Bari, Apulia, Southern Italy.
Methods
Study design, setting and participants
The preventive protocol was based on the latest guidelines published by WHO [6]. Current definitions by the European Centre for Disease Prevention and Control of suspected, probable and confirmed cases were adopted, as well as assessments of close and casual contact [7], to identify HCWs exposed to significant biological risk. This protocol was applied for all 5750 HCWs working at the University Hospital of Bari for a 30-day observation period after implementation of the protocol (21st February 2020). All HCWs were informed about the research protocol and its purpose.
General hygiene practices (e.g. avoiding hand shakes, frequent air changes in rooms, physical separation of suspected infected patients, room disinfection and avoidance of overcrowding) were reinforced among both HCWs and hospital users. Moreover, appropriate utilization of PPE was implemented. In this regard, all HCWs were educated about correct donning and doffing procedures carried out in the anteroom before and after making contact with suspected or confirmed cases, and were guided by signs to perform the actions correctly.
Reporting system pattern
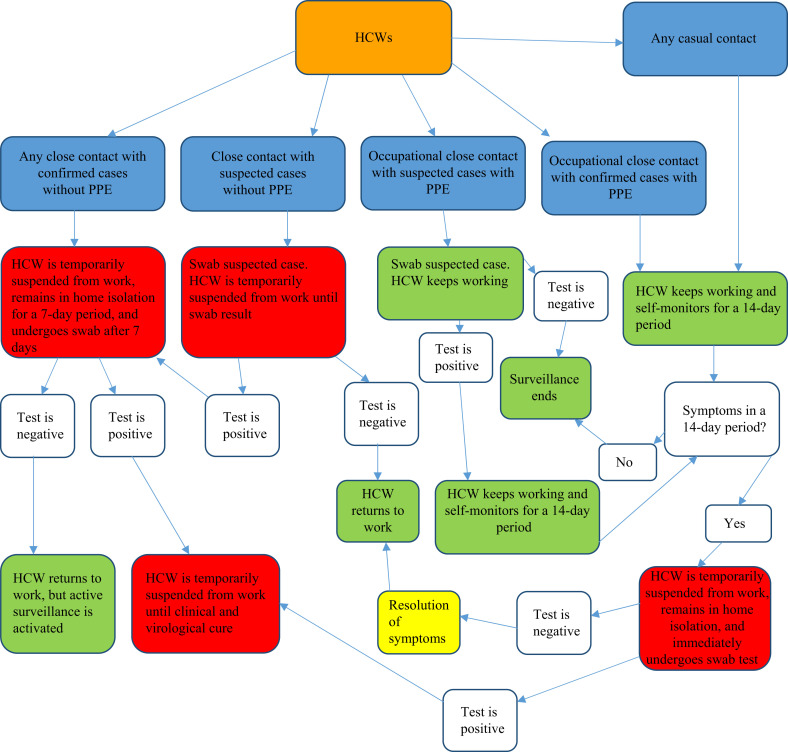
A reporting system was activated to collect and monitor all HCWs' contacts with cases with suspected or confirmed SARS-CoV-2. Reports started from a HCW that had contact with a case; he/she informed the head physician of his/her hospital ward, who in turn alerted a central control room, known as the ‘COVID-19 Control Room’, and the Operative Unit of Occupational Medicine. The Operative Unit of Occupational Medicine evaluated the clinical conditions and undertook virological assessment of each HCW to decide their resumption of work (Figure 1 ).
Figure 1.
Report system pattern for healthcare workers (HCWs).
HCWs who had close contact with a confirmed case without PPE were suspended from work for a 7-day period. Hospitalization was not required if their clinical condition was good; instead, home isolation was required under the control of the Prevention Department with territorial jurisdiction, located outside the hospital, which briefed the COVID-19 Control Room and Operative Unit of Occupational Medicine about workers' conditions and, on the last day, took nasopharyngeal swabs. A molecular test was performed for all HCWs who became symptomatic. HCWs who tested positive were not allowed to return to work until they were clinically and virologically cured; the latter was defined as negative results on two molecular tests in a 24-h period.
If a HCW tested negative for SARS-CoV-2, he/she was allowed to return to work but was subjected to active surveillance to detect early symptoms suggestive of SARS-CoV-2 (i.e. ageusia, anosmia, fever, cough, myalgia, weakness, dyspnoea, migraine), as a window of a few days is described for this infection.
HCWs who had close contact with a suspected case without PPE were suspended from work, and the suspected case underwent a swab test. If the patient was negative, the HCW was allowed to return to work. If the case was confirmed as SARS-CoV-2, the HCW followed the protocol for close contact with a confirmed case without PPE.
All HCWs who had close contact with PPE were reported to the COVID-19 Control Room, but they were allowed to continue to work. Self-monitoring was recommended for a 14-day period, as medical viral clearance is thought to be approximately 11 days in symptomatic patients and shorter in asymptomatic patients [8]. A swab test was performed if workers became symptomatic. HCWs with a negative test result were allowed to return to work, and HCWs with a positive test result were suspended from work until clinical and virological cure was documented.
HCWs who had casual contact were allowed to work, but self-monitoring was strongly recommended. In the case of symptoms, the management protocol was identical to the protocol utilized for close contact with PPE.
HCWs allowed to work had to avoid the workplace if they became symptomatic during a shift (i.e. fever, cough, myalgia, weakness, short breath, migraine) for a 14-day period after exposure; they also had to inform the COVID-19 Control Room and Operating Unit of Occupational Medicine of their symptoms. If symptoms started at home, workers had to inform the Prevention Departments outside the hospital, which in turn had to alert the COVId-19 Control Room and Operating Unit of Occupational Medicine. These HCWs underwent rapid swab testing; the protocol adopted after the swab result was identical to that for HCWs who had close contact with PPE.
Results and discussion
After implementation of the protocol, all notified close contacts of HCWs were recorded, and each case was scanned and verified by the COVID-19 Control Room and Operative Unit of Occupational Medicine. From the beginning of the epidemic in Italy (21st February 2020) to date, 7033 nasopharyngeal swabs have been taken from hospital users referred to pre-triage of the emergency department. These tests were justified by epidemiological (close contacts) and clinical (ageusia, anosmia, cough, fever, myalgia, weakness or SARI symptoms) criteria. Among the tests, 1065 were positive (15.14%) and 5968 were negative (84.86%). All involved HCWs reported contact modalities with these patients to the COVID-19 Control Room through the reporting system. Contacts of employees were also collected. Based on these reports, 560 HCWs' contact tracing forms were collected to determine all people who had contact with these HCWs. Moreover, based on the decision-making process shown in Figure 1, 1303 swabs were taken in the hospital setting over the 30-day observation period due to the high risk of HCWs' close contacts. Of these, only 16 (1.38%) swabs were positive (two after a second confirmatory test). Of swabs taken at home, seven were positive and reported to the COVID-19 Control Room. Overall, 23 HCWs (average age 48.6 years) were infected by SARS-CoV-2. Among these, 16 were doctors (two of whom were in training), five were nurses and two were social health assistants. Regarding the most commonly reported symptoms, weakness was present in 72% of workers, diarrhoea in 60%, cough in 56% and fever in 52%. Almost half of infected HCWs reported anosmia and ageusia.
The prevalence of SARS-CoV-2 infection among all HCWs working at the University Hospital of Bari was 0.4% (23/5750) over the 30-day observation period following implementation of the protocol (Table I ).
Table I.
Summary of results obtained over a 30-day period after implementation of a preventive protocol
| Hospital users | Total swabs | 7033 (100%) | |
| Positive swabs | 1065 (15.14%) | ||
| Negative swabs | 5968 (84.86%) | ||
| HCWs | Total swabs (in hospital setting) | 1303 (100%) | |
| Positive swabs (in hospital setting) | 16 (1.38%) | ||
| Negative swabs (in hospital setting) | 1285 (98.62%) | ||
| Positive swabs (outside hospital setting) | 7 | ||
| Total positive swabs among HCWs | 23 | ||
| Positive HCWs: average age (years) | 48.6 | ||
| Positive HCWs: specific task | 16 physicians (two of whom were in training) 5 nurses 2 social health assistants |
||
| Prevalence of SARS-CoV-2 infection among HCWs over a 30-day observation period | 0.4% | ||
HCWs, healthcare workers; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2.
This result is likely due to the adoption of correct prevention measures that focused on infection source control, administrative strategies, environmental control and correct PPE utilization, associated with ancillary hygienic measures to avoid overcrowding (e.g. reducing the number of HCWs in rooms hosting suspected and/or confirmed cases, organizing necessary bedside medical and surgical procedures in advance, using PPE for the maximum usage time, and performance of nasopharyngeal swabs by a single HCW per work shift).
Establishment of preventive protocols is essential to provide safe guidance for HCWs and consequently reduce their work-related stress, which is known to influence work performance [9]. The reporting system is also essential to prevent nosocomial outbreaks from HCWs; reports through this platform were mandatory for professional and environmental close contacts. In the protocol, the COVID-19 Control Room plays a central role in cooperating with Prevention Departments outside the hospital about suspected and confirmed cases of HCWs placed in home isolation. It also evaluates all people who have had contact with involved HCWs and ordains domiciliary nasopharyngeal swabs. It would be beneficial to monitor all patients who have had contact with involved HCWs in hospital by ward for a 14-day period. Patients who had been discharged from the hospital should be monitored in home isolation by the Prevention Department. Compliance with all appropriate prevention procedures, together with detailed reporting systems, are crucial to avoid hospital outbreaks and to achieve very low prevalence among HCWs. In this regard, Wang et al. [10], in a retrospective single-centre case series of 138 patients with COVID-19, estimated that 29% were HCWs working in the same hospital centre and infected during shifts due to occupational exposure to infected patients, compared with 0.4% in the present study. In this regard, half of the positive HCWs reported ageusia and anosmia; these seem to be early symptoms, if present, so great attention should be given to them from the outset. HCWs occupationally exposed to SARS-CoV-2 should be aware of the strategic importance of referring any close contact to the hospital management system, with a subsequent careful focus on all secondary contacts. Moreover, ward managers should ensure that there is effective performance of self-monitoring procedures, with particular regard to HCWs subjected to active surveillance.
In conclusion, this protocol had good results at the University Hospital of Bari, with only 23 HCWs found to be infected by SARS-CoV-2 after testing 1303 swabs. However, this result was based solely on swabs taken after accurate risk assessment; further studies are needed to understand the effectiveness of SARS-CoV-2 immunity among HCWs.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.World Health Organization . WHO; Geneva: 2020. WHO surveillance case definitions for ILI and SARI.https://www.who.int/influenza/surveillance_monitoring/ili_sari_surveillance_case_definition/en/ Available at: [last accessed April 2020] [Google Scholar]
- 2.Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anastassopoulou C., Russo L., Tsakris A., Siettos C. Data-based analysis, modelling and forecasting of the COVID-19 outbreak. MedRxiv. 2020 doi: 10.1371/journal.pone.0230405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quarato M., De Maria L., Gatti M.F., Caputi A., Mansi F., Lorusso P. Air pollution and public health: a prisma-compliant systematic review. Atmosphere. 2017;8:183. [Google Scholar]
- 5.Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;5 doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . WHO; Geneva: 2020. Novel coronavirus (2019-nCoV)https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Available at: [last accessed April 2020] [Google Scholar]
- 7.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2020. Case definition and European surveillance for COVID-19, as of 2 March 2020.https://www.ecdc.europa.eu/en/case-definition-and-european-surveillance-human-infection-novel-coronavirus-2019-ncov Available at: [last accessed April 2020] [Google Scholar]
- 8.Chen J., Qi T., Liu L., Ling Y., Qian Z., Li T. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020;80:e1–e6. doi: 10.1016/j.jinf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Sio S., Buomprisco G., Perri R., Bruno G., Mucci N., Nieto H.A. Work-related stress risk and preventive measures of mental disorders in the medical environment: an umbrella review. Eur Rev Med Pharmacol Sci. 2020;24:821–830. doi: 10.26355/eurrev_202001_20065. [DOI] [PubMed] [Google Scholar]
- 10.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]