Abstract
Purpose
There have been nearly 200,000 deaths worldwide so far from coronavirus disease 2019 (COVID-19), which is caused by a coronavirus called SARS-CoV-2. Cancer history appears to be a poor prognostic factor for COVID-19 patients, although the reasons for this are unclear. In this report, we assess whether extent of prior lung irradiation is a risk factor for death as a result of COVID-19 infection.
Methods and Materials
Patients who tested positive for COVID-19 between March 14 and April 15, 2020, at our institution and who previously received radiation therapy for cancer in our department were included in this analysis. Patient characteristics and metrics describing the extent of lung irradiation were tabulated. Cox regression models were used to identify predictors of death after COVID-19 diagnosis. A logistic model was used to characterize the association between mean lung radiation therapy dose and 14-day mortality risk after COVID-19 diagnosis.
Results
For the study, 107 patients met the inclusion criteria. With a median follow-up of 7 days from COVID-19 diagnosis for surviving patients, 24 deaths have been observed. The actuarial survival rate 14 days after COVID-19 testing is 66%. Increasing mean lung dose (hazard ratio [HR] per Gy = 1.1, P = .002), lung cancer diagnosis (HR = 3.0, P = .034), and receiving radiation therapy between 1 month and 1 year before COVID-19 testing (HR = 3.4, P = .013) were associated with increased risk of death. Our survival model demonstrates a near linear relationship between mortality risk after COVID-19 diagnosis and mean lung radiation therapy dose.
Conclusions
COVID-19 patients with a history of radiation therapy for cancer have a poor prognosis, and mortality risk appears to be associated with extent of lung irradiation. Validation of these findings will be critical as the COVID-19 pandemic continues.
Introduction
As of April 23, 2020, more than 2.6 million cases of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) coronavirus disease 2019 (COVID-19) infection have been documented worldwide, with nearly 200,000 deaths.1 Two reports from China suggest that, among patients with COVID-19 infection, cancer history is a risk factor for severe adverse events, including death.2,3 Larger series have demonstrated that advanced age and medical comorbidities are powerful predictors of death from COVID-19.4,5 These factors are also associated with cancer incidence, which may explain the link between cancer history and poor outcomes with COVID-19 infection. Alternatively, cancer or cancer treatments may directly impair patients’ ability to overcome COVID-19 infection.
Lung tissue may be exposed to therapeutic radiation when treating primary lung cancers or thoracic metastases or incidentally when treating other primary tumors, such as breast cancer or esophageal cancer. Radiation can cause lung epithelium injury and cytokine release, leading to acute or subacute inflammation (pneumonitis), which can be followed by aberrant wound healing (fibrosis).6 These changes can reduce pulmonary function and could conceivably impair patients’ ability to withstand COVID-19 pneumonia. In this report, we assess if extent of prior lung irradiation is a risk factor for death due to COVID-19 infection.
Methods
In this institutional review board–approved study, we used the electronic medical record from a single urban medical center to identify all patients who had tested positive for COVID-19 up until April 6, 2020, and were previously treated with therapeutic radiation in our department. Positive COVID-19 (SARS-CoV-2) status was determined based on reverse transcription quantitative polymerase chain reaction assay. Patient demographics, radiation therapy dose, and volume data for the lungs of all patients who received any thoracic radiation therapy, and clinical outcomes as of April 22, 2020 were tabulated.
The primary study outcome is overall survival (OS) duration, defined as the time from positive COVID-19 testing until death from any cause. Patient characteristics and extent of previous lung irradiation (quantified as mean radiation therapy dose delivered to the lungs) were tested as predictors of OS using univariate Cox proportional hazards models. Multivariable modeling was not performed due to our limited sample size and strong correlation between key potential prognostic factors (eg, mean lung radiation therapy dose and lung cancer diagnosis). Kaplan-Meier curves were generated to depict survival distributions in various patient subgroups, and comparisons were performed using log-rank testing.
We performed normal tissue complication probability (NTCP) modeling using a logistic function7 to further examine the relationship between mean lung radiation therapy dose and the actuarial rate of death 14 days after COVID-19 testing. Data were sorted into 3 groups based on mean lung dose, and the actuarial 14-day mortality rate for each group was calculated. These 3 data points were fit to the NTCP model using least-squares optimization. We used a bootstrap resampling method to formulate 95% confidence bounds for the NTCP curve.8 Finally, 10,000 iterations were performed.
Statistical analyses were performed using Matlab (The Mathworks, Natick, MA) and STATA (StataCorp, College Station, TX).
Results
We identified 107 patients who had positive COVID-19 tests at our institution and had previously received radiation therapy for cancer in our department. Patient characteristics are summarized in Table 1. The median follow-up duration after COVID-19 testing for surviving patients is 7 days (range, 0.5-39 days). Twenty-four deaths have been observed, occurring a median of 3 days after COVID-19 testing (range, 0.5-14 days). The actuarial survival rate 14 days after COVID-19 testing is 66%.
Table 1.
Patient and treatment characteristics
| Sex, n (%) | |
| Male | 53 (50%) |
| Female | 54 (50%) |
| Age, median (range), y | 70 (30-95) |
| Ethnicity, n (%) | |
| Non-Hispanic | 61 (57%) |
| Hispanic | 38 (36%) |
| Other/unknown | 8 (7%) |
| Primary cancer site,∗ n (%) | |
| Breast | 28 (26%) |
| Prostate | 27 (25%) |
| Lung | 14 (13%) |
| Gynecologic | 7 (7%) |
| Head and neck | 6 (6%) |
| Hematologic | 4 (4%) |
| Other | 23 (21%) |
| Interval from last RT to COVID-19 testing, n (%) | |
| <1 mo | 10 (9%) |
| 1 mo to 1 y | 18 (17%) |
| 1-5 y | 35 (33%) |
| >5 y | 44 (41%) |
| Mean lung radiation therapy dose, median (range) | 0.2 Gy (0-16.6 Gy) |
| Mean lung radiation therapy dose, n (%) | |
| 0 Gy | 52 (49%) |
| 0-4 Gy | 30 (28%) |
| >4 Gy | 25 (23%) |
Abbreviations: COVID-19 = Coronavirus Disease 2019; RT = radiation therapy.
Two patients had head and neck cancer and a second primary cancer diagnosis (lung, prostate).
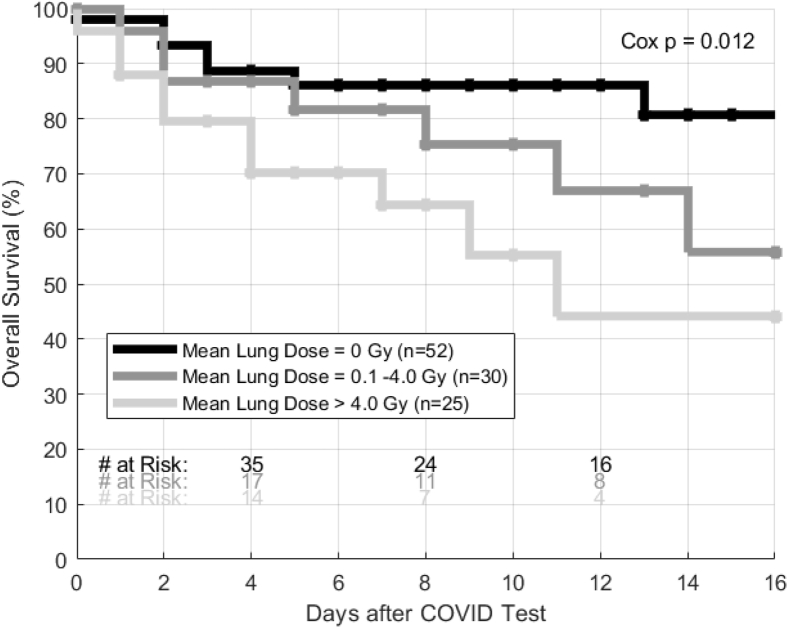
Cox proportional hazards models demonstrated a significant association between mean radiation therapy dose delivered to the lungs and risk of death (hazard ratio [HR] = 1.12 per Gy, 95% confidence interval [CI], 1.04-1.20, P = .002, Table 2). Kaplan-Meier curves depicting this association are shown in Figure 1. Lung cancer diagnosis was also associated with increased risk of death (HR = 2.96; 95% CI, 1.09-9.27; P = .034). Compared with patients who received radiation therapy at least 5 years before COVID-19 infection, patients who received radiation therapy 1 month to 1 year before COVID-19 infection had increased risk of death (HR = 3.42; 95% CI, 1.29-9.03; P = .013).
Table 2.
Cox proportional hazards models describing predictors of overall survival duration after COVID-19 testing
| Characteristic | Hazard ratio (95% CI) | P value |
|---|---|---|
| Sex | ||
| Male | [reference] | 0.037 |
| Female | 2.48 (1.06-5.81) | |
| Age, per y | 1.01 (0.98-1.05) | 0.370 |
| Ethnicity | ||
| Non-Hispanic/other/unknown | [reference] | - |
| Hispanic | 0.66 (0.26-1.66) | 0.374 |
| Primary cancer site | ||
| Breast | [reference] | - |
| Prostate | 0.13 (0.02-1.10) | 0.061 |
| Lung | 3.18 (1.09-9.27)∗ | 0.034∗ |
| Other | 1.07 (0.38-3.01) | 0.900 |
| Interval from last RT to COVID-19 testing | ||
| <1 mo | 0.40 (0.05-3.22) | 0.386 |
| 1 mo to 1 y | 2.96 (1.03-8.51)∗ | 0.044∗ |
| 1-5 y | 1.52 (0.57-4.09) | 0.405 |
| > 5 y | [reference] | - |
| Mean lung radiation therapy dose, per Gy | 1.12 (1.04-1.20)∗ | 0.002∗ |
| Mean lung radiation therapy dose | ||
| 0 Gy | [reference] | - |
| 0-4 Gy | 2.02 (0. 17-5.75) | 0.856 |
| > 4 Gy | 3.42 (1.29-9.03)∗ | 0.013∗ |
Abbreviations: COVID-19 = Coronavirus Disease 2019; RT = radiation therapy.
Statistical significance at the 5% level.
Figure 1.
Kaplan-Meier curves showing overall survival for patients grouped by mean lung radiation therapy dose received. Abbreviation: COVID = Coronavirus Disease 2019.
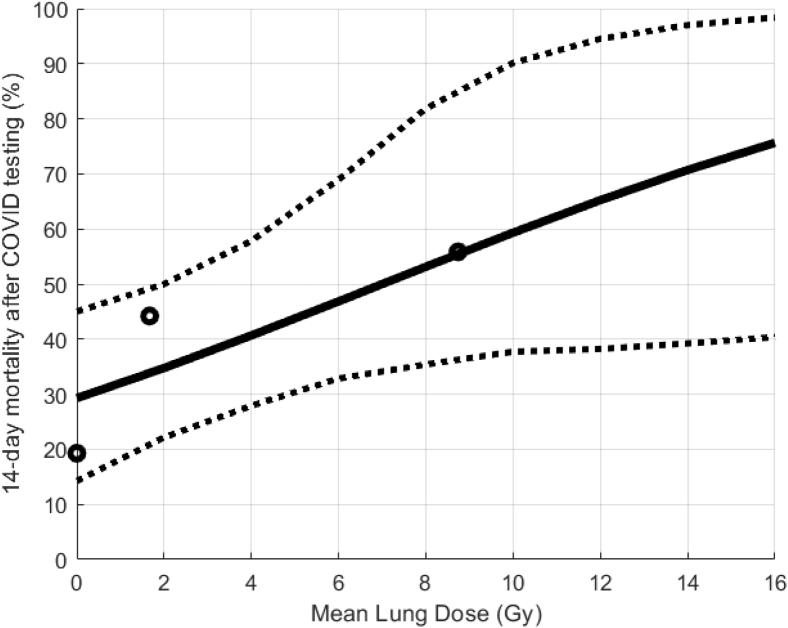
NTCP modeling results are depicted in Fig 2. Although a logistic (s-shaped) model was applied, mortality risk appears to increase linearly as a function of mean lung radiation therapy dose. For cancer patients without any prior lung exposure to radiation therapy, the predicted mortality rate is approximately 30%. A mean lung radiation therapy dose of 7 Gy yields a predicted COVID-19 mortality rate of approximately 50%, and a mean lung radiation therapy dose of 15 Gy yields a predicted COVID-19 mortality rate of approximately 75%.
Figure 2.
Normal tissue complication probability model of 14-day mortality after Coronavirus Disease 2019 (COVID) testing (solid line). Data points represent subsets of patients with mean lung radiation therapy dose of 0 Gy, <4 Gy, and > 4 Gy. Dashed lines represent 95% confidence intervals.
Discussion
In this analysis of emerging data from the COVID-19 pandemic, we found that prior radiation therapy for cancer is associated with a mortality risk of approximately 35%. This is consistent with prior reports that cancer history is a poor prognostic factor in the setting of COVID-19 infection.2,3,9 We are the first to report that extent of previous lung irradiation may be a critical prognostic factor in cancer patients with COVID-19.
If validated with longer follow-up in our patients and in other data sets, our findings could have profound implications as the COVID-19 crisis evolves. Patients with a history of prior lung irradiation who acquire COVID-19 may benefit from a low threshold for hospitalization and intensive supportive care. Patients with prior lung irradiation could be alerted to be particularly attentive to measures that can reduce COVID-19 exposure risk. Vaccines or other preventative interventions to minimize infection risk or disease severity could preferentially be offered to individuals with prior lung irradiation.
We examined mean lung radiation therapy dose as a prognostic factor in this analysis. We found that other metrics, including lung V20Gy (percentage of lung receiving at least 20 Gy) and lung V5Gy, showed similar predictive value as mean lung dose (data not shown). Larger studies will be needed to select the most important dosimetric factor and examine the effect of daily fraction size. Additional work will also be required to quantify the individual contributions of lung cancer diagnosis and prior lung irradiation as risk factors in COVID-19 patients.
Interestingly, we found that receipt of radiation therapy between 1 month and 1 year before COVID-19 diagnosis was associated with increased mortality risk. This timeframe overlaps the typical acute phase of radiation pneumonitis, which involves the induction of proinflammatory cytokines and chemokines that recruit immune cells to lung tissue, where inflammation causes damage to lung parenchyma, epithelial cells, vascular endothelial cells, and stroma.10 Similar pathways are engaged in severe COVID-19 cases,11 supporting the hypothesis that prior lung radiation therapy may increase the severity of COVID-19 pneumonia.
Limitations of this study include its relatively limited sample size and short follow-up duration. Validation of our findings in additional data sets is imperative. Future analyses will examine how prior lung irradiation affects the clinical presentation of patients with COVID-19, investigate outcomes other than mortality, and explore if specific interventions may be particularly effective in COVID-19 patients with a history of lung irradiation.
Footnotes
Sources of support: none.
Disclosures: None of the authors have any conflicts of interest that are related to this work.
Research data are not available at this time.
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China [epub ahead of print]. Ann Oncol. [DOI] [PMC free article] [PubMed]
- 4.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liang WH, Guan WJ, Li CC, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicenter) and outside Hubei (non-epicenter): A nationwide analysis of China [epub ahead of print]. Eur Respir J. [DOI] [PMC free article] [PubMed]
- 6.Kong F.-M., Ten Haken R., Eisbruch A., Lawrence T.S. Non-small cell lung cancer therapy-related pulmonary toxicity: An update on radiation pneumonitis and fibrosis. Semin Oncol. 2005;32(2 Suppl 3):S42–S54. doi: 10.1053/j.seminoncol.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Okunieff P., Morgan D., Niemierko A., Suit H.D. Radiation dose-response of human tumors. Int J Radiat Oncol Biol Phys. 1995;32:1227–1237. doi: 10.1016/0360-3016(94)00475-z. [DOI] [PubMed] [Google Scholar]
- 8.Deasy J.O., Chao K.S., Markman J. Uncertainties in model-based outcome predictions for treatment planning. Int J Radiat Oncol Biol Phys. 2001;51:1389–1399. doi: 10.1016/s0360-3016(01)02659-1. [DOI] [PubMed] [Google Scholar]
- 9.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lierova A., Jelicova M., Nemcova M. Cytokines and radiation-induced pulmonary injuries. J Radiat Res. 2018;59:709–753. doi: 10.1093/jrr/rry067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]