Introduction
At the end of 2019, a novel strain of the coronavirus emerged in Wuhan, China and caused a respiratory infection named coronavirus disease 2019 (COVID-19).1 Due to the rapid worldwide spread of the virus, the World Health Organization (WHO) officially declared COVID-19 a pandemic on 11 March 2020.2 In order to minimize the spread of the disease, many countries enacted precautionary measures, such as restrictions on gatherings and social distancing, following WHO guidelines.3
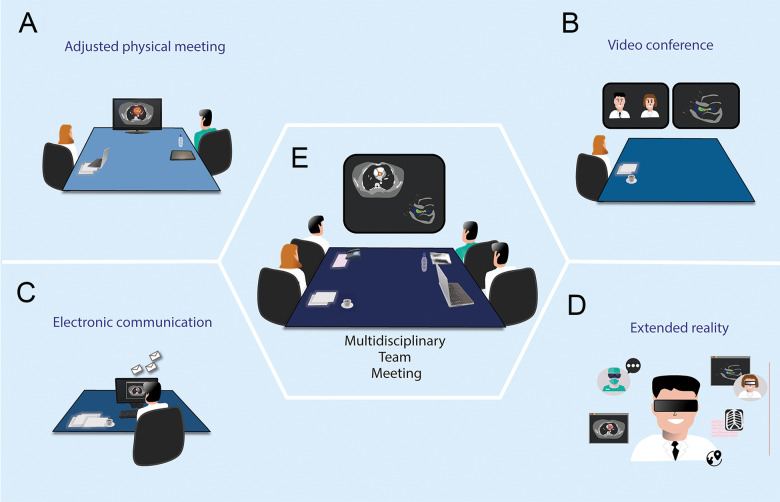
In daily clinical practice, the coming together of physicians for multidisciplinary team (MDT) meetings is essential for good patient care. Examples in the cardiovascular field are Heart Team evaluations for coronary revascularization, valvular pathologies, and endocarditis, which have been recommended by the European Society of Cardiology (ESC).4–6 Although these meetings are necessary and by definition not restricted, they could potentially increase the risk of spreading the virus, which should be prevented at all costs, particularly between healthcare professionals. In order to continue to provide good patient care while minimizing the risk of spreading the virus, other alternatives for conducting MDT meetings should be considered. In this article, we present four alternative methods (Figure 1), along with their benefits and drawbacks (Table 1).
Figure 1.
Options for physician meetings in this digital era.
Table 1.
Benefits and drawbacks of the four alternative methods proposed for the Heart Team meetings
| Methods | Benefits | Drawbacks |
|---|---|---|
| Adjusted physical meeting |
|
Remaining risk of infection or transmission of microorganisms |
| Video conference |
|
|
| Electronic communication |
|
|
| Extended reality |
|
|
Alternative methods
Adjusted physical method
Presumably, physical meetings remain the most common method for physicians working in the same hospital to come together. However, these meetings should be adjusted to minimize viral transmission by avoiding any direct physical contact, restricting the number of participants and gathering in larger conference rooms. Before and after the meetings, participants should be reminded to sanitize their hands. Since the key characteristic of this method—the physical presence of the participants in the same area—remains unchanged and little effort is required from the participants, many physicians might prefer this approach during the COVID-19 pandemic. However, even if the risk of spreading the virus is relatively small, the risk still exists, and can be seen as a significant drawback.
Video conferencing
Video conferencing is an obvious alternative when physical meeting is not possible, with the benefit of eliminating the risk of viral spreading. Another advantage is the possibility to involve healthcare providers from other hospitals. However, there are a number of drawbacks, including connection issues, which could hamper communication and the loss of facial expression and body language, due to the often limited resolution during a video call. Other pitfalls may include the challenge of organizing the meeting and preventing miscommunication, the need for secured software, and finding a way for participants to watch the same screen as the presenter of the case.
Electronic communication
Another form of telemedicine is the use of electronic communication systems, such as electronic mail (E-mail) and the electronic health record (EHR). The proposed method could be achieved by communicating the designated case through EHR or E-mail with one person that coordinates the entire communication with all the participants. Using the EHR is preferable because it is usually a more secure data system than E-mail and the conclusion of the meeting is directly communicated to the attending physician. The benefits of this communication method are similar to those of video conferencing, with the addition of clearer communication since all participants are required to send a written response. However, a major drawback is the time-consuming nature of this type of communication, which is not desirable when decisions have to be made quickly. Needless to say, there is a loss of facial expression, tone, and body language.
Extended reality
Extended reality (XR) refers to all technologies that are used to create computer-generated digital three-dimensional interfaces that combine physical (real-world) and virtual images that allow users to view and interact with both realities simultaneously.7 XR interfaces can provide various types of human–machine interaction, including augmented reality (digital overlays on to the physically observed reality), virtual reality (fully digital/imagined virtual world), and mixed reality (a hybrid of virtual and digital worlds that is responsive to the user and the real world).8 Using wearables (e.g. remote controllers) and head-mounted devices (e.g. Microsoft Hololens, Oculus Rift), the user is able to view, engage, and interact with these digital interfaces.8,9
Due to recent advances in the field of XR, virtual reality has found application in medical education and communication.10,11 Regarding communication, there is a growing body of literature on the development of software and hardware platforms that offer communication facilitated by XR modalities.12,13 These technologies enable teleconferencing and communication through the addition of new dimensions and features, such as video avatars, virtual rooms, animations, and digital interaction.12–14 There have been recent news reports on the use of XR in a telemedicine conference between three surgeons facilitated by a mixed reality interface.15 The benefits of this method are similar to those of video conferencing with the addition that the virtual interaction could be comparable with physical interaction.
However, the main question remains of whether these platforms are suitable for medical telecommunication purposes. In the context of medical televirtuality, platforms should preferably meet some strict security requirements to protect medical records and patient data. In addition, the hardware and software should be easy to use and allow interaction between physicians. With the recent and rapid developments in these emerging technologies, it is vital to assume that the application of XR in medical televirtuality will become a reality in the near future.
Essential role of a coordinator
The coordinator should have the responsibility to gather all information needed for each meeting, invite the essential participants, explain the steps of the meeting, and coordinate the meeting so it will be run smoothly. The role of a coordinator is essential in all of the proposed methods, especially in those that are prone to miscommunication.
Conclusion
To minimize the risks of transmission during the COVID-19 pandemic, alternative communication methods for MDT meetings, such as adjusted physical meetings, video conferencing, electronic communication, and immersive telecommunication (extended reality), may be considered based on local needs and resources.
Supplementary Material
Acknowledgements
We thank all the following from Erasmus Medical Center Rotterdam for their contribution to this work: Dr Nelianne J. Verkaik, Microbiologist; Dr Tjebbe W. Galema, Cardiologist; Dr Carolina A.M. Schurink, Infectious Disease Specialist; Dr Margreet W.A. Bekker, Cardio-Thoracic Surgeon; Edris Mahtab MD, PhD, Cardio-Thoracic Surgeon; Ad J.J.C. Bogers MD, PhD, Cardio-Thoracic Surgeon; Ricardo P.J. Budde MD, PhD, Radiologist; and Jolien W. Roos-Hesselink MD, PhD, Cardiologist.
Conflict of interest: none declared.
References
References are available as supplementary material at European Heart Journal online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.