Abstract
Objective
The study sought to evaluate early lessons from a remote patient monitoring engagement and education technology solution for patients with coronavirus disease 2019 (COVID-19) symptoms.
Materials and Methods
A COVID-19–specific remote patient monitoring solution (GetWell Loop) was offered to patients with COVID-19 symptoms. The program engaged patients and provided educational materials and the opportunity to share concerns. Alerts were resolved through a virtual care workforce of providers and medical students.
Results
Between March 18 and April 20, 2020, 2255 of 3701 (60.93%) patients with COVID-19 symptoms enrolled, resulting in over 2303 alerts, 4613 messages, 13 hospital admissions, and 91 emergency room visits. A satisfaction survey was given to 300 patient respondents, 74% of whom would be extremely likely to recommend their doctor.
Discussion
This program provided a safe and satisfying experience for patients while minimizing COVID-19 exposure and in-person healthcare utilization.
Conclusions
Remote patient monitoring appears to be an effective approach for managing COVID-19 symptoms at home.
Keywords: remote patient monitoring, patient education, telehealth, Covid-19, patient generated data
INTRODUCTION
Background and Significance
Since the coronavirus disease 2019 (COVID-19) outbreak began in December 2019, this pandemic has provided numerous challenges requiring healthcare systems and societies worldwide to respond in unprecedented ways to protect both patients and staff and to prepare for surges of critically ill patients. Healthcare systems are reporting their initial experiences including establishing safe COVID-19 testing options using drive-through methods,1 converting to a hospital incident command center structure for rapid prioritization and clear decision making,2 canceling elective surgeries,3 shifting or delaying other routine care,4 and aggressively converting in-person care to virtual options with significant telehealth transformation.5–8
In Minnesota, our healthcare system’s experience with COVID-19 included the previously described measures. We also notably created a dedicated COVID-19 hospital in 2 weeks to rapidly cohort hospitalized COVID-19 patients.9 Soon after the first case of COVID-19 appeared in the state of Minnesota on March 1, 2020, we also experienced rapidly increasing volumes at urgent care clinics and overwhelming numbers of calls with questions and appointment requests in a matter of days (call wait times went from 30 seconds to over 30 minutes). To combat this, we aggressively marketed the use of asynchronous, protocol-based e-visits for both COVID-19 and non–COVID-19 symptoms and observed a shift to e-visits by mid-March of over 4000% (from 50 to >2000 e-visits daily) and on-demand video visits. This increase in demand for virtual care was further complicated and necessitated by extremely limited COVID-19 testing options, so patients with COVID-19 symptoms were presumed to be infected and instructed to self-quarantine. With guidelines rapidly changing, patients reached out repeatedly for updated information, reassurance, and to understand when to seek care or additional evaluation. Together, these challenges uncovered a need to more systematically monitor and engage with presumed COVID-19 patients safely at home with the goal of narrowing in-person emergency care to those needing it most.
The use of remote patient monitoring (RPM) and engaging patients around their care at home has been previously described for chronic disease management and more episodic care such as after discharge following surgical procedures. For chronic diseases, RPM appears to be accepted by patients and to enhance management of congestive heart failure,10 chronic obstructive pulmonary disease,11 and a range of other chronic conditions.12 To date, there has been widespread interest in using RPM for COVID-19 patients,5 but little is known about the outcomes, acceptability, and lessons around program implementation.
OBJECTIVE
We sought to describe an integrated health system’s initial experience with a COVID-19 RPM program using an interactive engagement technology. Core areas we sought to explore included lessons from rapid technology deployment, program staffing, and program acceptability by both patients and staff.
MATERIALS AND METHODS
Setting
M Health Fairview is an integrated academic healthcare system with 12 hospitals (2071 beds), 56 primary care clinics, 100+ specialties, and 34 000 employees located in the urban Twin Cities area of Minnesota as well as with locations extending north to rural Minnesota and parts of western Wisconsin.
COVID-19 RPM solution overview
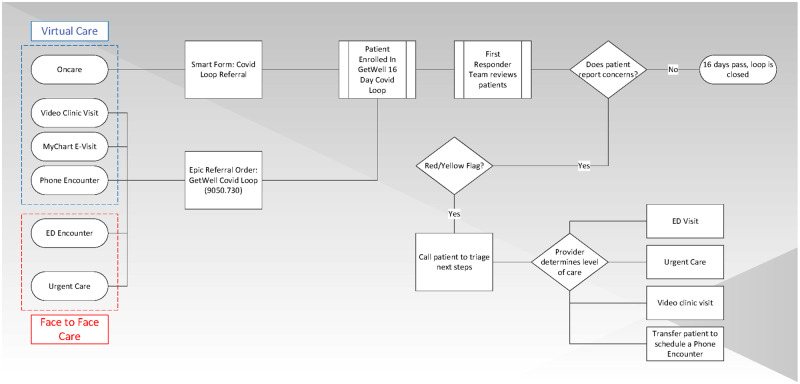
A patient education and RPM solution with COVID-19 specific content was configured and deployed (GetWell Loop; GetWellNetwork, Bethesda, MD) (Figure 1). The solution included critical steps of enrollment, engagement, monitoring with first responder escalation, and treatment completion. Prior to the COVID-19 outbreak, this platform was being used for enhanced recovery after surgery programs to offer educational materials and to engage patients around monitoring their pain control, diet, and other self-care. The COVID-19 specific program was able to repurpose this tool to handle the rapid influx of patients allowing for escalation protocols to first responders.
Figure 1.
COVID-19 remote patient monitoring program overview. ED: emergency department.
Engagement solution
Within GetWell Loop, patients are enrolled in a specific “loop,” which contains a set of patient education messages, reminders, and questions specific to a disease state or surgical procedure. Loops vary by duration and frequency of check-ins with the patient. For our COVID-19 loop, patients were given information about COVID-19, reminders about social distancing and hygiene, and daily check-in questions each morning to assess their symptoms. Information was supplied to patients through a scrolling newsfeed, where they also had the option of sending comments and questions to their care team. Symptom monitoring questions answered with potentially concerning results (eg, reporting severe shortness of breath) were flagged with either a red or yellow alert and routed to a dashboard for action by a member of the first responder team. Several weeks after our initial go live, there were 2 updates to the program’s content including a question that assessed pulse oximetry data, and the length of the RPM monitoring duration was adjusted from 18 days to 16.
Enrollment
Patients that were enrolled were either screened for COVID-19 through one of our virtual care platforms (online, phone, video) or at an urgent care or emergency department visit. To promote the program, system communications were sent to inform providers about the program as a care option for patients with confirmed or suspected COVID-19. We enabled a referral order within our EHR to gather the patients’ required information and developed a batch process to automate enrollment. Patients then receive an email with information on how to activate and begin the COVID-19 program. Nurse educators reached out to patients who had not yet activated their accounts to encourage them to do so.
Monitoring with first responder escalation
In order to staff this application and provide a valuable training opportunity across this and several other virtual care platforms, a virtual health rotation at the University of Minnesota was rapidly created for medical students and residents from multiple local programs including Internal Medicine, Medicine-Pediatrics and Family Medicine residencies. Residents and students on this rotation, with supervision from faculty, comprised the main workforce of the first responder team from 8 Am to 5 Pm during the peak volume of patient responses. The 8 Am to 5 Pm hours were typically covered by 3-4 medical students, 2-4 residents, and 1-2 dedicated supervising physicians who would either respond to patients with text comments or a phone call if an alert or comment was particularly concerning or complicated. Within the first few days, it was apparent that despite a notification to the patient to call the MHealth triage line for alerts or comments outside of 8 Am to 5 Pm, patients were still routinely sending messages in the RPM application after-hours. In response to this, we expanded the workforce to include providers already doing 24/7 virtual care to respond to these urgent after-hours alerts from 5 Pm to 8 Am. Additionally, as volumes rose in the first several weeks, the 8 Am to 5 Pm workforce was expanded to include a nurse practitioner supervising 2 nurse practitioner students.
Treatment completion and patient satisfaction
Patients could choose to opt out at any time if their symptoms resolved or if they were no longer interested in participating. Patients that completed their treatment course via either method were also administered 2 satisfaction survey questions asking whether they would be likely to recommend their doctor to a friend or family member and what they thought their care team did well. A Net Promoter Score was calculated for the recommendation question and was defined as promoters (extremely likely) minus subtractors (neutral, slightly unlikely, and extremely unlikely).13
RESULTS
Between March 18 and April 20, 2020, 3701 patients were offered the COVID-19 RPM program. Of those who activated the system, 1496 patients (62% women; median 38 years of age) completed the program, and 757 are currently active. The overall activation rate was 61.2% (see Table 1). A majority of patients who enrolled in the program were first seen and referred via an asynchronous online e-visit (n = 3178, 88.8%). Emergency or hospital encounters (n = 167, 4.58%) and office visits (n = 158, 3.9%) made up the remainder of the enrollees.
Table 1.
Usage statistics
| Version 1 (18 d) March 18-27, 2020 | Version 2 (16 d) March 27-April 10, 2020 | Version 3 (Pulse Ox) April 10-20, 2020 | Overall March 18-April 20, 2020 | |
|---|---|---|---|---|
| Enrolled | 1666 | 1378 | 657 | 3701 |
| Activated | 993 | 915 | 347 | 2255 |
| Activation, % | 59.6 | 66.4 | 53.5 | 60.9 |
| Currently active | 1 | 411 | 345 | 757 |
| Completed | 992 | 504 | 0 | 1496 |
| Total alerts | 318 | 1451 | 534 | 2303 |
| Red alerts | 252 | 255 | 371 | 878 |
| Comments | 2107 | 2182 | 324 | 4613 |
| Interactions | 5080 | 4902 | 788 | 10 770 |
| Checked in, % | 94.5 | 93.9 | 91.4 | 93.8 |
There have been 10 770 patient check-ins within the RPM solution in which patients interacted with or acknowledged content. Of all the patients who activated their accounts, 94% checked in at least once. Overall, each patient had an average of 1.0 alerts and 2.0 comments throughout their course of enrollment. Alert and comment volumes peaked at 12:00 Pm daily and there are at most 3.25 alerts and 18.99 comments per hour per 100 patients (see Table 2). Of the activated patients, 91 had an emergency department visit (median of 7 days into enrollment) and 13 were admitted to the hospital (median of 6 days into enrollment).
Table 2.
Alert and comment heat maps
| Ending at | 3:00 Am | 6:00 Am | 9:00 Am | 12:00 Pm | 3:00 Pm | 6:00 Pm | 9:00 Pm | 12:00 Am |
|---|---|---|---|---|---|---|---|---|
| Total red alerts per 100 active patients | ||||||||
| Monday | 0.29 | 0.75 | 1.91 | 3.25 | 0.87 | 1.28 | 0.46 | 0.41 |
| Tuesday | 0.07 | 0.97 | 1.56 | 3.13 | 1.27 | 1.34 | 0.22 | 0.37 |
| Wednesday | 0.14 | 0.42 | 1.47 | 3.02 | 0.70 | 1.05 | 0.42 | 0.14 |
| Thursday | 0.00 | 1.55 | 1.30 | 2.91 | 1.12 | 1.05 | 0.81 | 0.31 |
| Friday | 0.06 | 0.91 | 1.09 | 2.54 | 0.97 | 0.91 | 0.48 | 0.54 |
| Saturday | 0.06 | 0.84 | 1.10 | 2.45 | 1.68 | 1.16 | 0.58 | 0.19 |
| Sunday | 0.00 | 0.41 | 1.03 | 2.81 | 1.30 | 0.96 | 0.27 | 0.00 |
| Total patient comments per 100 active patients | ||||||||
| Monday | 0.87 | 1.10 | 7.07 | 17.10 | 10.84 | 6.26 | 2.61 | 2.38 |
| Tuesday | 0.07 | 0.67 | 5.81 | 18.99 | 10.50 | 6.33 | 3.20 | 2.01 |
| Wednesday | 0.35 | 0.70 | 6.45 | 15.71 | 8.20 | 6.24 | 2.17 | 1.19 |
| Thursday | 0.37 | 0.93 | 5.52 | 17.61 | 9.80 | 5.46 | 1.55 | 1.43 |
| Friday | 0.79 | 0.73 | 4.90 | 15.97 | 9.86 | 6.29 | 3.39 | 1.69 |
| Saturday | 0.52 | 0.65 | 3.81 | 13.88 | 8.59 | 6.07 | 3.42 | 1.61 |
| Sunday | 0.21 | 0.82 | 4.18 | 14.13 | 8.37 | 4.73 | 3.36 | 1.99 |
From the data that were available for the patients we had reached out to (N = 3270), 92% (n = 3142) had not been tested, 7.2% (n = 109) had tested negative, and 1% (n = 19) had tested positive. There were 300 patients that responded to the patient satisfaction questions within the application, of which 74% responded that they would be extremely likely to recommend their doctor, 18% were slightly likely, 5% were neutral, 0.7% were slightly unlikely, and 2% were extremely unlikely resulting in a Net Promoter Score of 66.5%.13 Patient comments about their satisfaction with the care team were predominantly positive about their experiences with the solution.
DISCUSSION
As with any rapid implementation, there are challenges that arise from building a plane while flying it, but overall our rapid deployment was largely successful for remotely monitoring and caring for potential COVID-19 patients. The RPM application did not require major modification to be used in this population health management use case, as the features within its former postsurgical use translated well. Things that could be improved include the capability to mass message patients, additional tools for measuring inflow and outflow of patients to the program, and a more streamlined process of enrolling patients.
The greatest success was patient feedback reporting that the program provided a sense of safety and a way to quickly access COVID-19–specific care. In examining satisfaction responses from patients, many patients expressed feeling cared for and protected during uncertain times. Testing and curative treatments are both largely unavailable today for COVID-19; however, this made it perhaps even more critical to support and monitor patients so that they were able to feel safe at home and could be advised to receive care when necessary. Future work should include a more robust analysis of patient experience as well as factors that influence patient decisions on whether to participate in this RPM system.
Anecdotally, patients reported avoiding an emergency department or urgent care visit because of the availability of a provider, but additional analysis will be necessary to establish if this RPM system significantly reduces unnecessary utilization of care. While it would have been ideal to be able to systematically test patients in the community and to automate the inclusion of those who were COVID-19 positive, the best that could be done feasibly was to enroll patients based on suspicion of their reported symptoms. It is clear that a massive increase in testing capacity is needed, which is exemplified in that over 91% of the population enrolled in the program have yet to be tested.
The newly created resident and medical student virtual care pandemic response rotation was another success, both for staffing this application and providing significant learning opportunities for medical resources who may have otherwise been sidelined. In addition, this intentional workforce of learners provides a way to ensure patients get consistent and current recommendations about care by providing updates for the students and residents each morning with any guideline changes and frequent didactic sessions on COVID-19 and virtual care topics. Some of the main challenges we experienced were titrating the program to ensure adequate staffing to match the widely variable number of newly enrolled patients and number of messages at any given time.
In condensing what typically requires a 4- to 6-month rollout process into a matter of 2 weeks, some limitations on helpful features were imposed. Our initial enrollment process was manual and inefficient. However, over the duration of the program, we added functionality to automate portions of the process and now have a real time interface solution. Customization of the technology platform was also extremely limited, making it difficult to introduce improvements. For example, while we identified early on the value of capturing pulse oximetry data for monitoring patients and studying the COVID-19 virus, this feature was not added until 3 weeks into the program. We are now planning to extend home monitoring with pulse oximetry to certain patients discharged from the hospital or emergency department.
CONCLUSION
Overall, we were able to quickly and effectively implement an RPM program by repurposing an existing third-party application, and rapidly developed a resident and student rotation to staff it. Patients have been extremely grateful and positive about their experience using the tool and feel it has helped them stay safe at home. This demonstrates what can be accomplished through a shared imperative and effective partnerships between industry, healthcare delivery, and academia.
AUTHOR CONTRIBUTIONS
G.B.M., S.Ba., and S.P. conceived the idea for the program and oversaw its development. G.B.M., and S.P. oversaw and developed medical rotation. T.A. supported RPM program development, managed its implementation, and performed data analysis. S.Bi. supported development and integrated with existing resources. J.A.T. helped develop and manage medical rotation. G.B.M., S.P., T.A., and J.A.T. wrote case report in consultation with G.H. and E.L.
ACKNOWLEDGMENTS
Our heartfelt gratitude goes out to the tireless efforts of our information technology teams, the team at GetWell Loop, MHealth Fairview operational leaders, academic faculty at the University of Minnesota, medical students, doctor of nursing practice students, residents, and faculty in the M Health Fairview Virtual Care Rotation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Ton AN, Jethwa T, Waters K, Speicher LL, Francis D.. COVID-19 drive through testing: an effective strategy for conserving personal protective equipment. Am J Infect Control 2020; 48 (6): 731–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ross SW, Lauer CW, Miles WS, et al. Maximizing the calm before the storm: tiered surgical response plan for novel coronavirus (COVID-19). J Am Coll Surg 2020; 230 (6): 1080–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM.. Elective surgery in the time of COVID-19. Am J Surg 2020; 219 (6): 900–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of Virtual Care. J Am Med Inform Assoc 2020; 219 (6): 900–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mann DM, Chen J, Chunara R, Testa PA, Nov O.. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Topf MC, Shenson JA, Holsinger FC, et al. A framework for prioritizing head and neck surgery during the COVID-19 pandemic. Head Neck 2020; 42 (6): 1159–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. DiGiovanni G, Mousaw K, Lloyd T, et al. Development of a telehealth geriatric assessment model in response to the COVID-19 pandemic. J Geriatr Oncol 2020; 11 (5): 761–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vaccaro AR, Getz CL, Cohen BE, Cole BJ, Donnally CJ.. Practice management during the COVID-19 pandemic. J Am Acad Orthop Surg 2020; 28 (11): 464–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.M Health Fairview converts Bethesda Hospital into state’s first dedicated COVID-19 care facility. https://www.mhealth.org/blog/2020/march-2020/m-health-fairview-converts-bethesda-hospital-into-dedicated-covid-19-facility Accessed April 26, 2020.
- 10. Sohn A, Speier W, Lan E, et al. Assessment of heart failure patients’ interest in mobile health apps for self-care: survey study. JMIR Cardio 2019; 3 (2): e14332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Walker PP, Pompilio PP, Zanaboni P, Bergmo TS, et al. Telemonitoring in Chronic Obstructive Pulmonary Disease (CHROMED). A randomized clinical trial. Am J Respir Crit Care Med 2018; 198 (5): 620–628. [DOI] [PubMed] [Google Scholar]
- 12. Walker RC, Tong A, Howard K, Palmer SC.. Patient expectations and experiences of remote monitoring for chronic diseases: Systematic review and thematic synthesis of qualitative studies. Int J Med Inform 2019; 124: 78–85. CrossRef][10.1016/j.ijmedinf.2019.01.013] [DOI] [PubMed] [Google Scholar]
- 13. LaMalfa K. 5 Point Versus 11 Point Scales. https://www.maritzcx.com/blog/uncategorized/5-point-versus-11-point-scales-part-2/ Accessed April 26, 2020.