To the Editor:
With the outbreak of the global coronavirus 19 (COVID-19) pandemic, the world's population has been forced to rapidly adapt to a new reality. “Social distancing”—a term virtually unknown 6 mo ago, has now driven radical changes in many of our time-honored practices. As the COVID-19 crisis unfolded, it became apparent that the traditional face-to-face encounters, which are a cornerstone of neurosurgical practice, would be both unwise and unsafe. It was during these times that telehealth was quickly recognized as a part of the solution. While telehealth was initially conceived as a means of serving rural and underserved areas, many subspecialties have now come to embrace it as a tool in delivering comprehensive healthcare.1-6
At our institution, much like at many other major academic centers, an extremely rapid roll-out of a telehealth program for the neurosurgical department was performed. In this letter, we present our experience with this implementation.
OVERVIEW
The quantitative data for this analysis were collected by querying the electronic medical record. Additionally, informal interviews were also conducted with residents, fellows, nurse practitioners, and administrators in an attempt to represent the multiple different perspectives on the telehealth implementation.
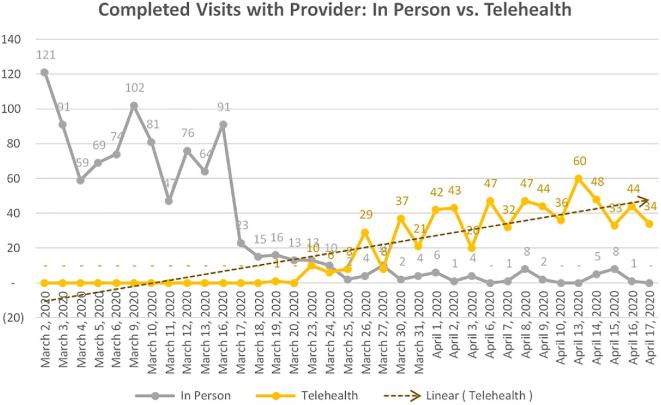
As the implications of the COVID-19 epidemic became apparent, our department began a self-imposed ramp-down of clinic activity by the second week of March. Using the weekly average clinic volume from March of 2019 as our “pre-COVID” baseline, this amounted to a 10% decline in face-to-face visits for the second week of March, a 62% decline for the third week of March, a 90% decline for the fourth week of March, and a 96% decline by the first and second weeks of April (Figure 1).
FIGURE 1.
Completed visits with the provider for both in-person and telehealth visits from March 2, 2020 until April 17, 2020. The dashed line is a linear trend line for the completed telehealth visits.
Acknowledging these changes and the growing need for an alternative means of ensuring ongoing care, our institution began to deploy telehealth capabilities. Within the first week of implementation, these efforts amounted to a 19% recapture in total patient visits. By the second and third weeks, this number increased to 52% of baseline activity, and by the fourth week, 70% of baseline activity had been recaptured.
TECHNICAL CHALLENGES
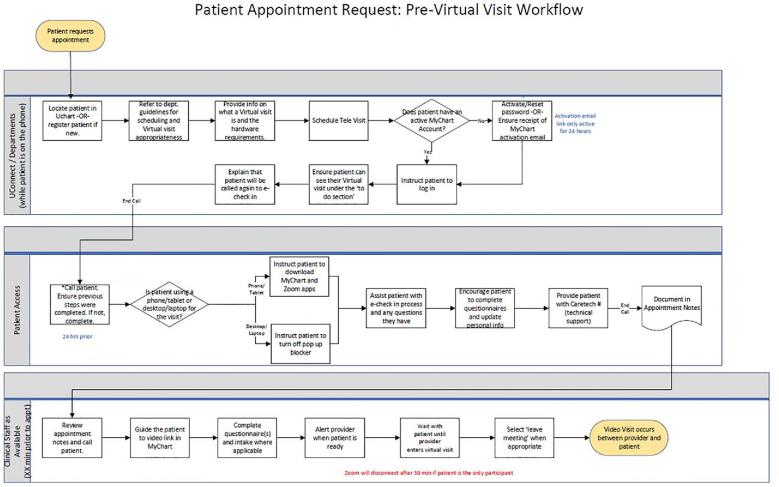
While there are various technological platforms that can be employed for a telehealth program, our university utilized the Zoom (Zoom Video Communications Inc, San Jose, California) application in conjunction with our electronic medical record platform (Epic, Epic Systems Corporation, Verona, Wisconsin). This meant that our patients needed to download not 1 but 2 separate applications in order to participate in a Zoom encounter. Therefore, to ensure clear and consistent steps were followed prior to each visit, a detailed workflow for a process map was created (Figure 2). Additionally, advanced encryption and restricted link distribution were used to ensure information security and patient confidentiality.
FIGURE 2.
Process map illustrating the telehealth workflow for the Department of Neurosurgery.
One of the major technological challenges faced early on was the uploading of patient images into our Picture Archiving and Communication System (PACS). In order to circumvent the traditional loading of images via disks, we were able to rapidly execute an agreement with a company providing an image-sharing platform—Ambra (Ambra Health, New York, New York). Since Ambra is already being utilized by 65 hospital systems in the state of Florida, this represented a tremendous opportunity to improve clinic workflow for both patients and clinicians.
BARRIERS TO ACCEPTANCE
Previous research has discussed the concept of “eReadiness” and “telehealth readiness.”7-9 “eReadiness” refers to a community's willingness to participate in telehealth and can be measured by capacity for change, along with perceived need for change.7-9 With regard to “capacity for change,” our institution was well-positioned due to previously allocated resources for a telehealth implementation. The second component of eReadiness, “perceived need for change,” was also generally less of an issue due to the state-wide “shelter-in” place order.
Age may also play a role in widespread adoption, as patients with advanced age may be constrained due to a lack of technological savvy. In these cases, we used one of the following 2 solutions: (1) the visit was converted into a telephone visit, or (2) the patients were instructed to present to the emergency room (if symptoms were concerning). Socioeconomic factors also clearly play a role in accessibility to telehealth. Indeed, while many of us take our smartphones and laptops for granted, these are resources that many individuals in underserved areas may not have access to.
To gauge the true patient experience in the long term, we have also worked to institute the Press Ganey “Telemedicine for Medical Practice Survey,” which more accurately reflects the challenges and experiences of a virtual encounter.10 This new survey will include the traditional postclinic questions along with questions specific to a telehealth setting.10
PATIENT SELECTION
While telehealth has many benefits, there are clearly some patients who are more well-served than others. Indeed, while the spine service achieved an almost 60% recapture of the weekly volume, the brain tumor service achieved only a 30% recapture rate. Multiple reasons may explain this striking discrepancy. First, spine patients are likely aware of symptoms resulting from their pathology such as pain or weakness and thus are likely to seek out specialist evaluation. In contrast, outpatient cranial imaging for softer indications (such as nonacute headaches) that lead to incidental discovery of brain tumors is likely to be less often approved, decreasing their diagnoses and referral to neurosurgical oncologists. Additionally, many referring subspecialists such as medical oncologists and neurologists may have a reduced clinic volume, further decreasing the discovery of new brain tumors. A second possible explanation for a larger percentage of patients seen compared to baseline in spine than cranial is that spine patients are often booked for clinic appointments many weeks out and therefore there is a larger backlog of patients waiting to be seen.
CONCLUSION
Telehealth implementation for outpatient neurosurgical clinic visits is feasible during the COVID-19 pandemic era with a careful analysis of technical considerations and patient selection.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. Dr Levi receives grant support from the NIH/NINDS and the Department of Defense, and teaching honoraria from the AANS and Medtronic. Dr Wang is a consultant for DePuy Synthes Spine, K2M, Stryker, and Spineology; he is a patent holder with DePuy Synthes Spine; and he has direct stock ownership in ISD and Medical Device Partners. Dr Urakov is a consultant for Medtronic. Dr Ivan is a consultant to and receiving research funding from Medtronic and the NX Development Corporation.
REFERENCES
- 1. Casey M, Hayes PS, Heaney D et al.. Implementing transnational telemedicine solutions: a connected health project in rural and remote areas of six northern periphery countries series on European collaborative projects. Eur J Gen Pract. 2013;19(1):52-58. [DOI] [PubMed] [Google Scholar]
- 2. Fraser HS, McGrath SJ.. Information technology and telemedicine in Sub-Saharan Africa. BMJ. 2000;321(7259):465-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Higgins CA, Conrath DW, Dunn EV. Provider acceptance of telemedicine systems in remote areas of Ontario. J Fam Pract. 1984;18(2):285-289. [PubMed] [Google Scholar]
- 4. Handschu R, Littmann R, Reulbach U et al.. Telemedicine in emergency evaluation of acute stroke: interrater agreement in remote video examination with a novel multimedia system. Stroke. 2003;34(12):2842-2846. [DOI] [PubMed] [Google Scholar]
- 5. Utidjian L, Abramson E. Pediatric telehealth: opportunities and challenges. Pediatric Clinics. 2016;63(2):367-378. [DOI] [PubMed] [Google Scholar]
- 6. Sabesan S, Kelly J.. Implementing telehealth as core business in health services. Med J Aust. 2015;202(5):231-233. [DOI] [PubMed] [Google Scholar]
- 7. Bukachi F, Pakenham-Walsh N.. Information technology for health in developing countries. Chest. 2007;132(5):1624-1630. [DOI] [PubMed] [Google Scholar]
- 8. Khoja S, Scott RE, Casebeer AL, Mohsin M, Ishaq AF, Gilani S. e-Health readiness assessment tools for healthcare institutions in developing countries. Telemed J E Health. 2007;13(4):425-431. [DOI] [PubMed] [Google Scholar]
- 9. van Dyk L. A review of telehealth service implementation frameworks. Int J Environ Res Public Health. 2014;11(2):1279-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Press Ganey Associates, Inc Telemedicine for Medical Practice Surveys Frequently Asked Questions, 2018. https://www.pressganey.com/docs/default-source/default-document-library/telemedicine-for-medical-practice_faqs_040918.pdf. Last Accessed April 13, 2020. [Google Scholar]