To the Editor:
According to the Global Healthcare Security (GHS) Index, the United States was the most prepared nation in the world to deal with pandemics (October, 2019).1 Now in the midst of the COVID-19 crisis, it is ironic that the United States has had more cases and deaths than any other nation.2 The same report found that other countries were even less prepared and there were major gaps in global healthcare security.1,2
Governments have had to make difficult decisions during this pandemic, balancing health against economic collapse. The decision to proceed with social distancing, banning nonessential travel, and closing large portions of the economy has been widely adopted around the world recognizing this will likely have long-standing economic consequences.3-5
The aim of our study was to explore the impact of this pandemic on neurosurgeons with the hope of improving preparedness for future crisis.
We created a 20-question survey designed to explore demographics (nation, duration and scope of practice, and case-burden), knowledge (source of information), clinical impact (elective clinic/surgery cancellations), hospital preparedness (availability of personal protective equipment [PPE] and cost of the supplies), and personal factors (financial burden, workload, scientific and research activities). The survey was first piloted with 10 neurosurgeons and then revised.
Surveys were distributed electronically in 7 languages (Chinese, English, French, German, Italian, Portuguese, and Spanish) between March 20 and April 3, 2020 using Google Forms, WeChat used to obtain responses, and Excel (Microsoft) and SPSS (IBM) used to analyze results. All responses were cross-verified by 2 members of our team. After obtaining results, we analyzed our data with histograms and standard statistical methods (Chi-square and Fisher's exact tests and logistic regression).
Participants were first informed about the objectives of our survey and assured confidentiality after they agreed to participate (Helsinki declaration).6
We received 187 responses from 308 invitations (60.7%), and 474 additional responses were obtained from social media-based neurosurgery groups (total responses = 661). The respondents were from 96 countries representing 6 continents (Figure 1A-1C).
FIGURE 1.
Demographics. A, A bar chart graph showing the participants’ distribution according to the region. B, A bar chart graph showing the participants’ distribution according to the COVID-19 country's case load. C, A bar chart graph showing the participants’ distribution according to the practice setting.
Ethical Committee
Ethics board approval was waived by the ethical committee of the neurosurgery department at Cairo University.
PERCEPTION AND KNOWLEDGE
The respondents from higher income nations (odds ratio [OR] = 2.25, CI = 0.12-42.20) and those with a greater burden of illness (OR = 5.25, CI = 0.36-75.94) were more likely to appreciate the seriousness of the pandemic. Some of this perception is likely related to a nation's overall investment in healthcare. Clearly, nations with robust epidemic surveillance systems will be forewarned of upcoming threats and be able to inform their healthcare workforce.
It was concerning to recognize that in some regions, particularly Africa, the knowledge regarding this pandemic was largely acquired from less credible sources (social media/television) (P < .001, OR = 4.85, CI = 2.09-11.24). Neurosurgeons from lower income nations reported lesser use of rigorous sources than wealthier nations (P < .05, OR = 0.60, CI = 0.42-0.86), suggesting that investment is needed to better disseminate high-quality information.
HOSPITAL PREPAREDNESS
Forty-six percent of respondents felt their hospitals were “insufficiently prepared” (Figure 2). Increased hospital preparedness was significantly seen more frequently among neurosurgeons from higher income nations (P < .05, OR = 4.92, CI = 1.25-19.29). The perception of better preparedness was most evident in the Eastern Mediterranean (P < .05, OR = 2.84, CI = 1.11-7.27) when compared to Africa. When we compared responses from individuals in exclusively private practice (P < .05, OR = 2.21, CI = 1.23-4.00) or governmental practice settings (P < .05, OR = 1.63, CI = 1.07-2.48), the perception of well preparedness was more likely than those who practiced in both settings.
FIGURE 2.
A bar chart graph showing the distribution according to the hospital preparedness.
ELECTIVE SURGERIES AND CLINICS
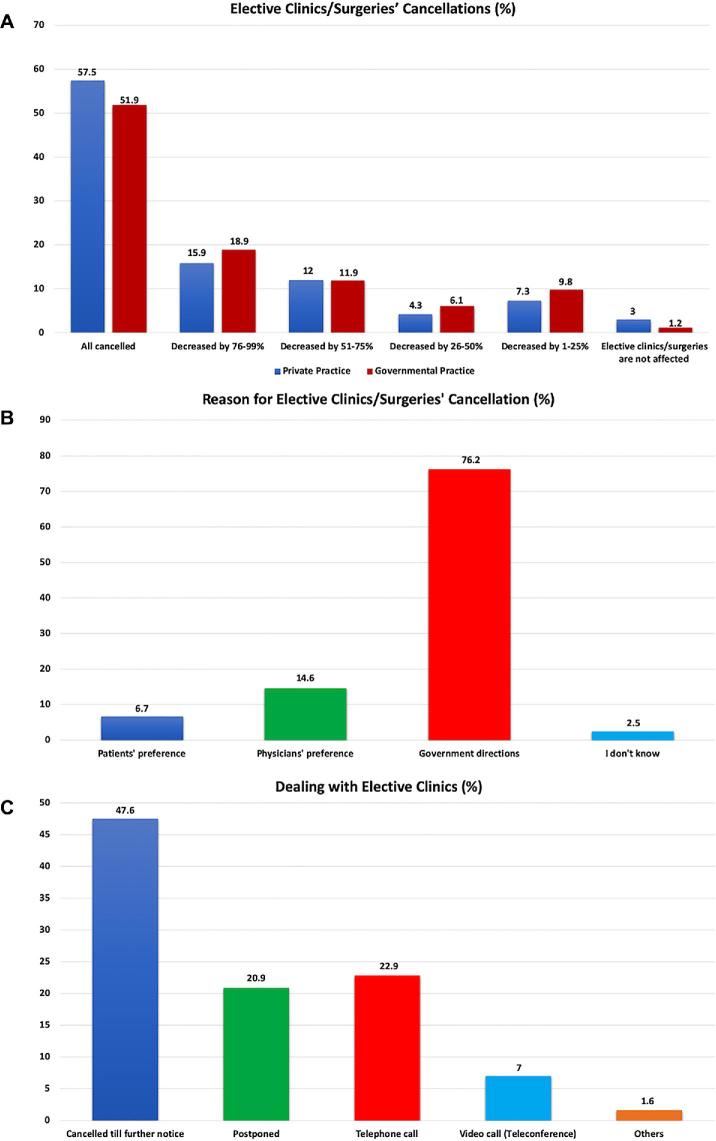
Healthcare delivery has transformed as well, with nonessential contact being prohibited. In private practices, elective surgery/clinic cancellations of >50% seemed to occur more frequently in non-African countries. In government-run facilities, such cancellations paradoxically occurred more frequently in lower prevalence regions (Figure 3A).
FIGURE 3.
Elective clinic/surgery cancellations. A, A bar chart graph comparing the distribution according to the percentage of elective clinic/surgery cancellations in the private and governmental sectors. B, A bar chart graph showing the distribution according to the main reason of elective clinic/surgery cancellations. C, A bar chart graph showing the distribution according to how they managed the elective clinics.
In private practice, it was patients and physicians who significantly motivated the surgery/clinic cancellations as opposed to government directives (P < .05, OR = 0.52, CI = 0.28-0.98). In governmental settings, it was government directives that led to these cancellations (P < .05, OR = 1.89, CI = 1.14-3.13). Cancellations also increased as nations acquired more COVID-19 cases in government settings (OR = 2.94, CI = 1.35-6.42) (Figure 3B).
Finally, regarding clinic appointments, there was a significantly higher rate of cancellation or rescheduling in upper middle income countries (P < .05, OR = 0.20, CI = 0.05-0.82) and insufficiently prepared hospitals (P < .05, OR = 0.61, CI = 0.40-0.93).
When our survey explored the adaptation of neurosurgeons to social distancing, we found varying responses (Figure 3C). There was a significantly increased utilization of telephone and teleconferencing over cancellations in private practice settings (P < .05, OR = 2.02, CI = 1.06-3.88), high-income countries (P < .05, OR = 2.64, CI = 1.02-6.19), and regions where the perception of the pandemic was more seriously appreciated (P < .05, OR = 3.20, CI = 1.37-7.50).
HOSPITAL SUPPLIES AND PERSONAL PROTECTIVE EQUIPMENT
We were also disturbed to find that price gouging during this international crisis was not only occurring in the public domain (eg, toilet paper) but also with hospital supplies. Of all respondents, 12.1% raised this concern regarding surgical implants.
When healthcare must be delivered, it is incumbent on our institutions to provide such care in the safest possible manner. This has been another challenge across the planet with a scarcity of essential medical equipment and personal protective equipment (PPE). We were alarmed to find that many of our respondents were not utilizing PPE (12%), and this was more common in lower income nations (P < .05, OR = 0.441, CI = 0.216-0.90). However, respondents from areas with lower burden of illness (151-1000 [P < .05, OR = 3.70, CI = 1.46-9.39] and 1001-10 000 [P < .05, OR = 2.93, CI = 1.21-7.15]) and a greater perception of threat (P < .05, OR = 3.47, CI = 1.32-9.12) were utilizing PPE more (Figure 4).
FIGURE 4.
A bar chart graph showing the distribution of utilization of PPE.
ECONOMIC, SCIENTIFIC, RESEARCH IMPACT
The reduction in clinical services has also had an impact on surgeons. The majority of our respondents (71.4%) reported a decreased workload (Figure 5) and financial burden (62.5%) (Figure 6). These surgeons were more likely to be spine or peripheral nerve surgeons (P < .05, OR = 0.30, CI = 0.10-0.88) or from low-income nations (P < .001, OR = 0.28, CI = 0.15-0.54).
FIGURE 5.
A bar chart graph showing the distribution according to the change in the workload.
FIGURE 6.
A bar chart graph showing the distribution according to presence of financial burden.
Although emergency procedures are likely to be continuing in most countries, it is unusual for neurosurgeons to receive their reimbursement primarily from such care. Increased hospital preparedness (P < .05, OR = 0.50, CI = 0.30-0.82) and being government-employed (P < .001, OR = 3.41, CI = 1.79-6.48) seemed to protect against financial difficulties.
The implications of closures on wait-times and healthcare outcomes remain unknown, but delayed treatment will likely have long-term consequences. Responsibility for such consequences remains to be determined. Physicians, hospitals, governments, or nations may become targets for future liability. This too contributes to physician stress.
Half of respondents (50.4%) stated that their scientific activities had been suspended, while 26.7% reported cessation of research (Figure 7). Cancellation of educational activities was more likely in the Americas (P < .05, OR = 3.30, CI = 1.04-10.48) and Europe (P < .05, OR = 3.72, CI = 1.03-13.47). Cessation of research was more common in low-income nations (OR = 2.28, CI = 0.59-8.85) and countries with a COVID-19 caseload of 1001-10 000 (OR = 1.05, CI = 0.46-1.11).
FIGURE 7.
A bar chart graph comparing the distribution according to the changes in the scientific/educational activities and research activities.
In conclusion, our survey provides insight into the COVID-19 pandemic. We found that many neurosurgeons lacked credible knowledge and that their institutions were inadequately prepared. This has resulted in a paralysis of healthcare delivery, which has harmed patients. As we move forward, we must learn from our mistakes so we may be better prepared.
Global healthcare initiatives have already proven successful with human immunodeficiency virus (HIV) and malaria.7-10 Empowering lower income nations to proactively contain these epidemics has wider implications for global healthcare security. In the 1980s, such initiatives in Africa to combat acquired immunodeficiency syndrome (AIDS) were quickly translated into combating Ebola in 2014 and 2016.11,12 We all have benefited from such programs.
We encourage increased resource allocation for better pandemic preparedness. Neurosurgeons must develop disaster strategies to curtail future crises through collaboration and communication, which has never been seen before.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
Acknowledgments
Dedication: “To our brothers and sisters that have fallen to this invisible enemy. As we write this article hundreds of physicians throughout the world died at the frontline fighting the COVID-19 infection. In these unprecedented times our thoughts, actions and prayers are with them and their families.” Major contributors (arranged according to their contribution): Abdulkadir A Hussein, Mayrelis Llerena Bernal, Mostafa Elhalaby, Mohamed Akl, Soraia Sousa, Maria Cahua, Dante J. Morassutti, Shijie Zhou, HebatAllah Qassim, Shun Yao, Sameh Elmorsy, Zolo Yvan, Rene Marquez-Franco, Negru Ancuta, Mohammad Altarawneh, Luca Ricciardi, Aigerim Zhumadildina, Rana Aziz, Mohammad Fathy Adel, Reem Elwy, Abdallah Elkhateeb; Contributors (alphabetical order): Aaron C Sigler, Abasin Aziz, Abbas Taskeen, Abdallah Ouammou, Abdelfatah Alaosta, Abdelghani Benmoussa, Abdelhafid Kechicheb, Abdelhafidh Slimane, Abdelmalek Adel, Abdufarrukh Karimov, Abdullah Alawad, Abdulqader Alsaiwed, Abdurrhim Elashaal, Abenezer Aklilu, Abhirama Chandra Gabbita, Achal Gupta, Adefisayo Adekanmbi, Adel AlZahrani, Adil Belhachmi, Adriel Salazar Lopez, Ahmad Gooda, Ahmed Abdul Aziz, Ahmed Aly, Ahmed Belal, Ahmed Cheema, Ahmed El Damaty, Ahmed ElGhamry, Ahmed A.M. Ezzat, Ahsan Khan, Al-Qatawneh Omar, Al-Rammahi Ammar Mohammed, Ala' Marji, Ala’a Al-Mousa, Alejandro Mende Vivetos, Alejandro Rochin, Alessandra de Moura, Alexander Gotin, Alexandros Apostolou, Ali Saud Alabid, Amal Rizky, Amitendu Sekhar, Amr Mohamed, Anan Shtaya, Andres Almendral, Andrew Huh, Andrew Jea, Andrew Koivuniemi, Ansar Ahmed, Anton van Aswegen, Antonio Romano, Antonio Uehara, Anurag Pundir, Arturo Alvarez, Ashwani Kumar, Asif Shafiq, Azedine Medhkour, Binoy kumar, Bipin chaurasia, Boniface Kivevele, Boniface Kivevele, Boris Djurovic, Brad Bohnstedt, ByungChan Jeon, Carlos Giménez, Carlos Lisboa Neto, César Peñate Ahuath, Chandrasekhar Yandrapati, Chirag Solanki, Chudy Nwafuluaku, Claire Karekezi, Constantine Constantoyannis, Crishian Cruz, Daniel Cabezas, Daniel Curry, Davi Solla, David Ojeda, Delenda madiha, Dhaval Shukla, Dipesh Batra, Diptiranjan Satapathy, Doriam Perera, Anurag Sihag, David YC Chan, Edgar Sotillo, Eduardo Barreto, Edwin Huerto Jara, Elena Beretta, Elshan Huseynzade, Emad Algwefie, Emmanuel Batista, Emmanuel E. Albano Jr, Enrique Coritza, Enrique Luna, Ezz Mansor, Fauzan Hashmi, Felix Millan, Fernando Oviedo, Firas Ejielat Qurayyat, Flavio axpuac, Fran Arteaga, Francesco Cozzi, Francisco Villegas, Francisco Yépez, Franco Falco, Franklin Meza, Furqan Nizami, Gebreagziabher Gebrekirstos, Ghulam Mustafa, Gino Mendoza, Gokmen Kahilogullari, Goksin Sengul, Griselda Ramírez, Habchi Nawel, Haitham Kandel, Hamzeh albadawi, Hany Elnemr, Harleen Luther, Harshavardhan Raorane, Hazem Gouda, Hector Farid Escorcia, Hesham Edwal, Higa Pedro Fiorito, Homoud AlDahash, Horacio Barea, Hossam Anaswh, Hugo Miranda, Humayun Rashid, Hussam Abou-Al-Shaar, Iakob Tsertsvadze, Ibrahim Althobaiti, Ibrahim Omran, Ignatius Esene, Ihor Poliakh, Ihsan Dogan, Jacques Favre, Jaime Hernández, Jaime Rimoldi, Jakob Kraschl, James Miller, Javier Miranda, Javier Sánchez, Jeffrey Raskin, Jehan Zeb, Jeremy Omoro, Jesse Savage, Jesus Esteban, Jorge Chasipanta, Jose Gimenez, Juan Carlos Reina Gama, Juan Marelli, Juan Sales, Juan Solivera, Julio César Delgado, Julio Eulogio, Julius Höhne, Juvenal Huanca, Karl Balsara, Khadjimurad, Khaldoun Al-sabouni, Kodela Atchiyyanaidu, Koral Erdoğan, Korawit Wangsirikul, Kuldeep Vala, Kyle Swanson, Lai Fung LI, Laura Baeza, Leonardo Fiori, Lorena Figueroa, Louis Valéry, Ludy Farfán, Luis E Perez Garza, Magyory Mujica, Maher Hassounah, Mainul Hossain, Mallyolo Pelayo, Manuel S. Gadea Nieto, Marcos Vilca-Aguilar, Mariela Infante, Mario Flavio Dávila, Maurice George, Max Kuzmich, Maykell Queiroz, Mbaye Thioub, Al Amin Salek, Medaglia Stefano, Mehmet Aydogan, Mehul Modi, Mian Awais, Michihiro Tanaka, Milan Analia, Miracle C. Anokwute, Mitesh V. Shah, Moh Albalta, Mohamed Abdelrahman, Mohamed Amine, Mohamed Ellabbad, Mohamed Elmaghrabi, Mohammad Baraka, Mohammad Elbaroody, Mohammad Shahnawaz Bari, Muhammad Adil, Muhammad Emaduddin, Muhammad Irfan Khan, Mustafa Alnkhly, Mustafa K. Baskaya, Mustapha Bacha, Mynzhylky Berdikhojayev, Nathalie Ghomsi, Nauman Ahmed, Nicolae-Stefan Bogaciu, Nicolas Penet, Nicolás Samprón, Nicolas Villelli, Nicu Ribac, Nidal Abuhadrous, Nimesh Jain, Norally Santeliz, Noureddine Tebib, Nqobile Thango, Nurzhan Borykbayev, Oscar Angel Choque, Pablo Fiorillo, Pankaj Chauhan, Patrick Bärtschi, Paulo M Porto de Melo, Pavitra Patnaik, Pedro Brol, Perez López, Pham Ngoc Hai, Piermassimo Proto, Puneet Rana, Raffaele Nigro, Ramez Kirollos, Ramiro Pérez de la Torre, Ramy Kamel, Rav Tej Bathala, Rene Garcia Angelo, Ricardo Bermúdez, Ricardo Gómez-Espinosa, Rodolfo Rodas, Rolando Cárdenas, Sai Sudarsan Puduru, Sajid Khan, Salah Alakkad, Salih Jan, Samuel Akinola, Santos Edgar, Satish Kumar Tiwari, Sergey Danchuk, Shams Danish, Shamsuzzama, Shelly D. Timmons, Shokry Alakhras, Sidi Salem-Memou, Sohaib Ashraf, Sourabh Dixit, Stephen Santoreneos, Su Mo, Subir Dey, Sunil Munakomi, Suyale Liu, Syed Mohammad, Taher Janbek, Tan Bih Huei, Tao Xu, Tariq Harb, Timothée de Saint-Denis, Tsegazeab Laeke, Valeriy Cheburakhin, Ventura Jaquez, Victor Castellano, Vikas V, Viktor Aleinikov, Vincenzo Testa, Vinod Kumar, Vishwaraj Ratha, Waleed Dabbas, Wasim Saleh, Wenli Chen, Wesam elmajry, Xiaobin Fei, Yadhu K L, Yahya Elnaggar, Yalla Abolgasem, Yasser Al-Troudi, Yermek Kali.
REFERENCES
- 1. GHS Index Report and Model GHS Index. https://www.ghsindex.org/report-model/. Accessed April 16, 2020.
- 2. COVID-19 Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed April 17, 2020.
- 3. Rapid Risk Assessment: Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK – Eighth Update, April 8, 2020. European Centre for Disease Prevention and Control. https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-pandemic-eighth-update. Accessed April 12, 2020.
- 4. Community-Based Measures to Mitigate the Spread of Coronavirus Disease (COVID-19) in Canada, April 3, 2020. AEM. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html. Accessed April 12, 2020.
- 5. Fong MW Gao H Wong JY et al.. Early release—nonpharmaceutical measures for pandemic influenza in nonhealthcare settings—social distancing measures. Emerg Infect Dis 2020;26(5):976-984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Medical Association World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373-374. [PMC free article] [PubMed] [Google Scholar]
- 7. Harman S. The World Bank: failing the multi-country AIDS program, failing HIV/AIDS. Glob Gov. 2007;13(4):485-492. [Google Scholar]
- 8. Institute of Medicine (US) Committee on the US Commitment to Global Health The US Commitment to Global Health: Recommendations for the Public and Private Sectors. Washington (DC): National Academies Press; 2009. https://www.ncbi.nlm.nih.gov/books/NBK23788/. Accessed April 16, 2020. [PubMed] [Google Scholar]
- 9. Syed SB Dadwal V Rutter P et al.. Developed-developing country partnerships: benefits to developed countries? Global Health. 2012;8(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Orac CG. Health equity: challenges in low income countries. Afr Health Sci. 2009;9(Suppl 2):S49-S51. [PMC free article] [PubMed] [Google Scholar]
- 11. Vetter P Dayer J-A Schibler M et al.. The 2014-2015 Ebola outbreak in West Africa: hands on. Antimicrob Resist Infect Control. 2016;5(1):17. [Google Scholar]
- 12. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Global Health; Committee on Global Health and the Future of the United States Global Health and the Future Role of the United States. Washington (DC): National Academies Press; 2017. https://www.ncbi.nlm.nih.gov/books/NBK458470/. Accessed April 16, 2020. [Google Scholar]