Abstract
Aims
To evaluate the impact of the COVID-19 pandemic on patient admissions to Italian cardiac care units (CCUs).
Methods and Results
We conducted a multicentre, observational, nationwide survey to collect data on admissions for acute myocardial infarction (AMI) at Italian CCUs throughout a 1 week period during the COVID-19 outbreak, compared with the equivalent week in 2019. We observed a 48.4% reduction in admissions for AMI compared with the equivalent week in 2019 (P < 0.001). The reduction was significant for both ST-segment elevation myocardial infarction [STEMI; 26.5%, 95% confidence interval (CI) 21.7–32.3; P = 0.009] and non-STEMI (NSTEMI; 65.1%, 95% CI 60.3–70.3; P < 0.001). Among STEMIs, the reduction was higher for women (41.2%; P = 0.011) than men (17.8%; P = 0.191). A similar reduction in AMI admissions was registered in North Italy (52.1%), Central Italy (59.3%), and South Italy (52.1%). The STEMI case fatality rate during the pandemic was substantially increased compared with 2019 [risk ratio (RR) = 3.3, 95% CI 1.7–6.6; P < 0.001]. A parallel increase in complications was also registered (RR = 1.8, 95% CI 1.1–2.8; P = 0.009).
Conclusion
Admissions for AMI were significantly reduced during the COVID-19 pandemic across Italy, with a parallel increase in fatality and complication rates. This constitutes a serious social issue, demanding attention by the scientific and healthcare communities and public regulatory agencies.
Keywords: COVID-19, SARS-CoV2, Acute myocardial infarction, STEMI, Cardiac care units
Introduction
The ongoing pandemic caused by the novel SARS-CoV-2 has already been associated with thousands of deaths worldwide. Italy was one of the first Nations in Europe to be affected.1 During data collection, the most affected area in Italy was the north of the country, where the healthcare system was overwhelmed with the huge number of patients in need of mechanical ventilation or intensive care.2 As a way to contain the disease, the government established a stepwise strategy starting from the complete lockdown of initial foci in northern Italy on 20 February 2020 and subsequent adoption of progressively more stringent lockdown measures of the entire nation as of 11 March.3,4
Already during the initial outbreak, many healthcare workers noticed a reduction in patient admissions for acute myocardial infarction (AMI), raising concern among cardiologists across Italy.
Methods
We conducted a multicentre, observational, nationwide survey aimed at evaluating consecutive patients with AMI admitted to Italian intensive cardiac care units (CCUs) throughout a 1 week period during the COVID-19 outbreak in Italy: 12–19 March. The same data were also collected for the equivalent week of 2019. All consecutive AMI patients admitted during the 1 week window were included, independently of their age. AMI was defined according to the Fourth Universal Definition of Acute Myocardial Infarction.5 Major complications were defined as cardiogenic shock, life-threatening arrhythmias, and cardiac rupture/ventricular septal defect (VSD) or severe functional mitral regurgitation.
Data were analysed for two pre-specified groups of patients: (i) ST-segment elevation myocardial infarction (STEMI); and (ii) non-ST-segment elevation MI (NSTEMI). Additional analyses were planned on patients with CCU admission for heart failure (HF), atrial fibrillation (AF), failure of the implantable device (DF), and pulmonary embolism (PE), even though the collection of these data was optional.
The Italian Society of Cardiology (Società Italiana di Cardiologia, SIC) invited all affiliated and associated Italian hospitals to participate through the CCU Academy network (https://www.sicardiologia.it/sito/publicFiles/2019_11_27_Roma_UTIC%20programma.pdf) including academic and non-academic hospitals with CCUs receiving AMI patients.
Data collection and data quality
Data on the number of patients admitted for each of the above-reported diagnoses at CCUs were recorded, along with patients’ age and gender. Collection of data about patients admitted for AMI in both 1 week periods in 2020 and 2019 was mandatory for participation in this survey. Information on admission for HF, AF, DF, and PE was optional, together with the total delay from symptom onset to coronary angiography and the time from first medical contact to revascularization for STEMI patients.
At each site, a coordinating investigator was responsible for screening consecutive patients admitted to the CCU and for data collection. Data were collected at single centres from their institutional records using case report forms provided by the coordinating unit. Data on CCU admissions and patient-related information were cross-checked against records of catheterization laboratories and COVID-19 wards of the same institution. Centres that did not use electronic records of admissions were asked to verify data with their Department of Management. After collection, participating centres submitted filled-in case report forms to the coordinating unit at Magna Graecia University, in charge of reporting all data onto the central electronic database. Data were finally checked for missing or contradictory entries and for values out of the normal range at the coordinating centre.
Statistical analysis
Categorical variables are presented as absolute numbers, percentages, and risk ratio (RR) with 95% confidence interval (95% CI), and compared by the χ2 test. Continuous variables are presented as mean and standard deviation (SD) and compared by the Student’s t-test, and weighted regression analysis was used to assess the impact of factors on case fatality and complication rates. IBM SPSS Statistics 23 was used for all analyses.
Results
A total of 54 hospitals participated in the study. Of these, 28 (51.9%) were academic hospitals and 26 (48.1%) non-academic hospitals. Among them, 48 (88.9%) were coordinating hubs within the STEMI network, 51 (94.4%) had cardiac catheterization facilities, and 32 (59.3%) had a cardiac surgery unit.
A total of 319 AMIs were registered during the 2020 week, with a 48.4% reduction (95% CI 44.6–52.5) compared with the equivalent week in 2019 (P < 0.001), when 618 patients were hospitalized for the same diagnosis (Figure 1). More detailed results are reported in Table 1. Looking at single subgroups, weekly STEMI admissions were reduced from 268 in 2019 to 197 in 2020 (26.5% reduction; 95% CI 21.7–32.3; P = 0.009). No difference was registered in mean patient age (65.1% in 2019 vs. 66.5 in 2020; P = 0.495). Within the STEMI subgroup, a lower proportion of women were registered in 2020 (20.3%) compared with 2019 (25.4%) (P < 0.001). The reduction of admissions for STEMI was higher among women (41.2%; P = 0.011) than men (17.8%; P = 0.191). The reduction in admission for STEMI was comparable among academic (21.5%) and non-academic hospitals (19.5%) (P = 0.473). Coronary angiography rates were comparable between 2020 and the previous year (94.9% vs. 94.5%; P = 0.562).
Figure 1.
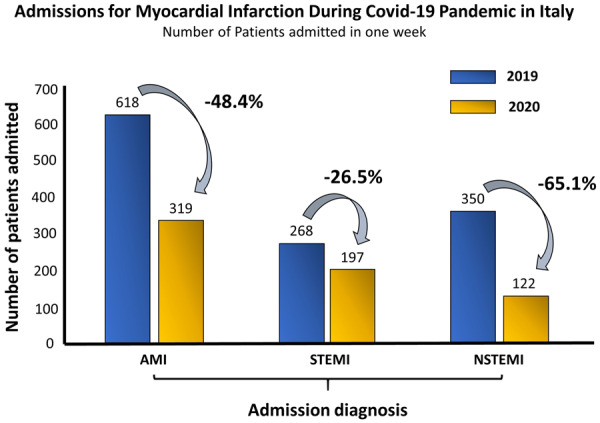
Admissions for acute myocardial infarction across Italy. The figure reports the number of admissions registered among Italian cardiac care units (CCUs) during the week 12–19 March 2020, in the midst of the COVID-19 emergency (yellow bars) and during the same week of the previous year (blue bars) for comparison.
Table 1.
Admissions for specific diagnoses
| 2019 |
2020 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Centres | Adm | SexF | Age | Adm | SexF | Age | Change | 95% CI | P-value | |
| AMI | 54 | 618 | 176 | 67.1 ± 9.5 | 319 | 76 | 68.0 ± 9.0 | 48.4% | 44.6–52.5 | <0.001 |
| STEMI | 54 | 268 | 68 | 65.4 ± 9.7 | 197 | 40 | 66.5 ± 10.2 | 26.5% | 21.7–32.3 | 0.009 |
| NSTEMI | 54 | 350 | 108 | 68.9 ± 9.3 | 122 | 36 | 69.6 ± 8.1 | 65.1% | 60.3–70.3 | <0.001 |
| HF | 50 | 154 | 59 | 72.3 ± 10.1 | 82 | 30 | 72.9 ± 9.7 | 46.8% | 39.5–55.3 | 0.005 |
| AF | 48 | 88 | 29 | 70.0 ± 7.5 | 41 | 17 | 64.6 ± 12.3 | 53.4% | 43.9–64.9 | 0.017 |
| DF | 49 | 19 | 6 | 76.9 ± 5.4 | 7 | 3 | 70.6 ± 15.2 | 63.2% | 0.45–0.89 | 0.349 |
| PE | 34 | 17 | 6 | 69.1±13.3 | 12 | 2 | 70.8 ± 11.2 | 29.4% | 0.14–0.61 | 0.667 |
Absolute number of patients admitted during the 2019 (light blue columns) and the 2020 (yellow-shaded columns) index weeks are reported, along with sex and age. Percentage change in admissions in 2020 compared with 2020 is reported (Change). 95% confidence intervals (95% CI) are also reported, followed by the P-value.
Every line reports data on a single disease: AMI = acute myocardial infarction; STEMI = ST-segment elevation myocardial infarction; NSTEMI = non-ST-segment elevation myocardial infarction; HF = heart failure; AF = atrial fibrillation; DF = device failure; PE = pulmonary embolism; Adm = admissions; SexF = number of females.
Figure 2.

Case fatality rates for acute myocardial infarction. The figure reports case fatality rates among patients admitted for AMI during the week 12–19 March 2020, in the midst of the COVID-19 emergency (yellow bars) and during the same week of the previous year (blue bars).
The STEMI case fatality rate during the pandemic was substantially increased to 13.7% compared with the 4.1% registered in 2019 (RR = 3.3, 95% CI 1.7–6.6; P < 0.001) (Table 2). Major complications were registered in 18.8% of cases in 2020 and in 10.4% in 2019 (RR = 1.8, 95% CI 1.1–2.8; P = 0.025) (Table 3).
Table 2.
Case fatality rate
| 2019 |
2020 |
||||||
|---|---|---|---|---|---|---|---|
| Centres | Adm | Dead (%) | Adm | Dead (%) | RR (95% CI) | P-value | |
| AMI | 54 | 618 | 17 (2.8) | 319 | 31 (9.7) | 3.6 (2.0–6.4) | <0.001 |
| STEMI | 54 | 268 | 11 (4.1) | 197 | 27 (13.7) | 3.3 (1.7–6.6) | <0.001 |
| NSTEMI | 54 | 350 | 6 (1.7) | 122 | 4 (3.3) | 1.9 (0.5–6.7) | 0.309 |
Absolute number of patients admitted and the number of deaths during the 2019 (light blue columns) and the 2020 (yellow-shaded columns) index weeks are reported. Risk ratios are reported in the next column, together with their 95% confidence intervals (95% CI), followed by the P-value.
Every line reports data on a single disease: AMI = acute myocardial infarction; STEMI = ST-segment elevation myocardial infarction; NSTEMI = non-ST-segment elevation myocardial infarction; Adm = admissions; RR = risk ratio.
Table 3.
Major complications rates
| 2019 |
2020 |
||||||
|---|---|---|---|---|---|---|---|
| Centres | Adm | Complications | Adm | Complications | RR (95% CI) | P-value | |
| AMI | 54 | 618 | 46 (7.4) | 319 | 50 (15.7) | 2.1 (1.4–3.1) | <0.001 |
| STEMI | 54 | 268 | 28 (10.4) | 197 | 37 (18.8) | 1.8 (1.1–2.8) | 0.009 |
| NSTEMI | 54 | 350 | 18 (5.1) | 122 | 13 (10.7) | 2.1 (1.05–4.1) | 0.037 |
Absolute number of patients admitted and the number of major complications during the 2019 (light blue columns) and the 2020 (yellow-shaded columns) index weeks are reported. Risk ratios are reported in the next column, together with 95% confidence intervals (95% CI), followed by the P-value.
Every line reports data on a single disease: AMI = acute myocardial infarction; STEMI = ST-segment elevation myocardial infarction; NSTEMI = non-ST-segment elevation myocardial infarction; Adm = admissions; RR = risk asratio.
Among STEMI patients, 21 (10.7%) were SARS-CoV2 positive. The case fatality rate among SARS-CoV2-positive STEMIs was substantially higher (28.6%) compared with all other STEMI patients registered during the same week in 2020 (11.9%). Nevertheless, the STEMI fatality rate in 2020 remained significantly higher than in 2019 even after excluding SARS-CoV2-positive patients (P = 0.018).
Both patient- and system-related declared delays were substantially increased during the COVID-19 outbreak. In fact, the time from symptom onset to coronary angiography was increased by 39.2% in 2020 compared with the equivalent week in 2019, while the time from first medical contact to coronary revascularization was increased by 31.5%.
Weekly hospitalizations for NSTEMI went down from 350 in 2019 to 122 in 2020 (65.4% reduction; 95% CI 60.3–70.3; P < 0.001) (Figure 1). No difference was registered in mean patient age (68.9 in 2019 vs. 69.6 in 2020; P = 0.812). The proportion of female patients among NSTEMI cases was similar in 2020 (29.8%) and 2019 (30.9%). The reduction of admission for NSTEMI was also similar among women (66.7%; P < 0.001) and among men (65.4%; P < 0.001). The proportion of NSTEMI patients undergoing percutaneous coronary intervention (PCI) was reduced by 13.3% (P = 0.023) from 2019 (76.7% of NSTEMIs) to 2020 (66.1% of NSTEMIs). The reduction in admissions for NSTEMI was comparable among academic (66.4%) and non-academic hospitals (58.7%) (P = 0.163). The NSTEMI case fatality rate was 3.3% during the pandemic, compared with 1.7% in 2019 (RR = 1.9, 95% CI 0.5–6.7; P = 0.309). Major complications were registered in 10.7% of cases in 2020 and in 5.1% in 2019 (RR = 2.1, 95% CI 1.05–4.1; P = 0.037). Among NSTEMI patients, 12 (9.8%) were SARS-CoV2 positive. No deaths were registered among these.
Since the time course of the COVID-19 outbreak was not synchronous across Italy, we divided the country into three macro-areas to look for possible variations. However, a similar reduction in AMI admissions was registered in North Italy (52.1%), Central Italy (59.3%), and South Italy (52.1%).
A similar reduction in hospitalizations was also registered for HF. In fact, only 82 patients were hospitalized for HF during the 2020 week, compared with 154 during the equivalent week in 2019 (46.8% reduction, 95% CI 39.5–55.3; P = 0.005). The mean age of HF patients was 72.3 ± 10.1 years in 2019 and 72.9 ± 9.7 in 2020 (P = 0.769). The reduction of admissions for HF was similar among men (44.1%; P = 0.017) and women (49.2%; P = 0.010).
A substantial reduction in hospitalizations was noted for AF. In fact, a total of 41 AF-related hospitalizations were registered during the 2020 week, with a 53.4% reduction (95% CI 43.9–64.9) compared with the equivalent week in 2019 (P = 0.017), when 88 patients were hospitalized for the same diagnosis. The mean age of AF patients was 70.0 ± 7.5 years in 2019 and 64.6 ± 12.3 in 2020 (P = 0.139).
Finally, a 29.4% reduction (95% CI 0.45–0.89) was registered for DF (P = 0.349) while a 63.2% reduction (95% CI 0.14–0.61) was found for PE (P = 0.667).
Discussion
The main finding of the present study is the dramatic reduction in the number of hospitalizations for AMI across Italy during the COVID-19 pandemic. In fact, admissions for AMI were halved during the pandemic compared with the equivalent period of the previous year. The identification of the mechanisms leading to the reduction in admissions for myocardial infarction are beyond the scope of the present work. Nevertheless, it is tempting to speculate that probably a multiplicity of factors, rather than a unique mechanism, contributed to the phenomenon. First, it is possible that the fear of contagion at the hospital has discouraged access to emergency medical services (EMS), particularly after the media diffused the news that the infection was largely spread across hospitalized patients and healthcare personnel due to the lack of personal protection equipment. The similar reduction in AMI admissions across Italy, despite the fact that one might have expected a stronger impact in the North, the most affected area, seems to point in that direction.2 A second hypothesis is linked to the fact that the emergency medical system was focused on COVID-19 and most healthcare resources were relocated to manage the pandemic. This might have induced an attitude towards deferral of less urgent cases, at both the patient and the healthcare system levels. In line with this hypothesis, the reduction in hospitalizations for STEMI (26.5%) was less striking than with NSTEMI (65.1%). These results are in line with contemporary findings, where an estimated 38% reduction in STEMI activations was reported by US cardiac catheterization laboratories,6 while a 40% reduction was noticed in Spain.7 Of note, this seems to also be true for the in-hospital management of AMI patients. In fact, despite the proportion of patients undergoing primary PCIs remaining very high among those admitted for STEMI also during the COVID-19 pandemic, the rate of PCI performed among admitted NSTEMI patients dropped significantly. Despite some CCUs being switched to COVID-19 beds, the reduction of admission for AMI was not linked to the lack of non-COVID-19 beds, as CCU beds in non-COVID-19 areas remained available. Finally, we cannot completely exclude that a true reduction in the incidence of acute cardiovascular disease as the potential result of low physical stress and widespread prevalence of the resting state during the quarantine, especially in the initial phase of the social containment, might have partly contributed to the lower number of admissions for AMI. However, this latter hypothesis is not entirely in line with the delay that we and others observed between symptom onset and hospital admissions for STEMI.8
It should also be pointed out that in this COVID-19 outbreak, the time from first medical contact to coronary revascularization was substantially increased in STEMI patients. This is a very important issue since it has been previously demonstrated that primary PCI and reperfusion therapies are necessary, but not sufficient: the efficiency of the care pathway in expediting each step of the process matters tremendously for STEMI patients,10–13 but is also very relevant to other coronary syndromes.14 In this regard, the substantial increase in case fatality and complication rates observed during the pandemic points in the same direction.
These data return a frightening picture of about half of AMI patients not reaching out to the hospital at all, which will probably significantly increase mortality for AMI and bring with it a number of patients with post-MI HF, despite the fact that acute coronary syndrome management protocols were promptly implemented.15 In addition to that, the higher case fatality and major complication rates registered during the hospitalization in this report must sound an alarm bell to healthcare professionals and public regulatory agencies. The higher reduction of admissions for STEMI among women (41.2%) compared with men (25.4%) extends the proportion of the problem, as the already intolerable gender gap in the treatment of AMI is further widened by this social emergency and will most probably result in a further increase in cardiovascular mortality and morbidity among women.10,11 The lower admission rate for HF (46.8%), PE (63.2%), DF (29.4%), and AF (53.4%) is also worrisome.
Study limitations
Collecting clinical data during a pandemic emergency is challenging and is exposed to several risks. First, the organization of in-hospital cardiology assistance has certainly been impacted by the situation, as many hospitals underwent functional reorganization to assist COVID-19 patients. For this reason, to avoid under-reporting, we asked participating centres to cross-check their records against records from their catheterization laboratories and COVID-19 wards, as well as with their medical management. Nevertheless, a residual risk might have persisted. Secondly, the management of the pandemic drained most resources, and extensive data collection was not possible, especially during the initial phase. For this reason, we had no choice but to leave out non-essential but potentially relevant variables, such as infarct size, clinical risk scores, or the time from symptom onset to admission for NSTEMI cases. For the same reason, the study period was limited to 2 weeks. Despite no relevant differences in weather conditions and no environmental alerts being recorded between those weeks in 2019 and 2020, the use of such a short period for data collection still represents a source for potential bias. Finally, as this is an observational study, we just describe a phenomenon. No demonstration of cause can be drawn from this study.
In conclusion, while healthcare systems along with public opinion, media, and patients were focused on the COVID-19 pandemic, a worrying reduction in admissions for AMI was observed across Italy with a parallel increase in case fatality and complication rates. Timely adoption of countermeasures must be considered to avoid a large and long-standing social impact.
Acknowledegements
We thank all participating centres and the researchers that collected the data: Filippo Angelini (CCU, AOU S. Giovanni Battista, Turin), Francesco Barillà (CCU B ‘A. Reale’, Umberto I University Hospital, Rome), Antonio Bartorelli (Centro Cardiologico Monzino, IRCCS and Department of Biomedical and Clinical Sciences ‘Luigi Sacco’, University of Milan, Milan), Francesco Benedetto (Bianchi Melacrino Morelli Hospital, Reggio Calabria), Paola Bernabò (Ospedali Galliera, Genova), Leonardo Bolognese (CCU, Ospedale S. Donato, Arezzo), Martina Briani (CCU, Humanitas Research Hospital, Rozzano), Luisa Cacciavillani (Azienda Ospedaliera, Padova), Alice Calabrese (CCU, ASST Papa Giovanni XXIII, Bergamo), Paolo Calabrò (CCU, AORN S. Anna e S. Sebastiano, Vanvitelli University, Caserta), Luigi Caliendo (CCU, ASL Napoli 3 - Nola), Leonardo Calò (Policlinico Casilino, Rome), Gianni Casella (UTIC, Ospedale Maggiore, AUSL Bologna, Bologna), Gavino Casu (CCU, Ospedale S. Francesco, Nuoro), Claudio Cavallini (AO di Perugia, Perugia), Quirino Ciampi (CCU, AO ‘Fatebenefratelli’, Benevento), Marco Ciccone (CCU, Policlinico di Bari, University of Bari, Bari), Michele Comito (CCU, Ospedale G. Jazzolino, Vibo Valentia), Elena Corrada (CCU, Humanitas Research Hospital, Rozzano), Filippo Crea (CCU, Policlinico A. Gemelli, Catholic University, Rome), Antonello D’Andrea (CCU, ‘Umberto I’ Hospital, Nocera Inferiore), Maurizio D’Urbano (CCU, Ospedale di Legnano, Legnano), Raffaele De Caterina (CCU, CCU AOU Pisana, University of Pisa), Gaetano De Ferrari (CCU, AOU S. Giovanni Battista, Turin), Roberto De Ponti (CCU, OSPEDALE ASST Sette Laghi, Varese), Alessio Della Mattia (CCU, AAS 5 ‘Friuli Occidentale’, Pordenone), Carlo Di Mario (CCU, AOU Careggi, University of Florence, Firenze), Luca Donnazzan (CCU, Ospedale di Bolzano, Bolzano), Giovanni Esposito (CCU, AOU Policlinico Federico II, Federico II University, Naples), Francesco Fedele (CCU A, Umberto I University Hospital, Rome), Alessandro Ferraro (CCU, AO Pugliese Ciaccio, Catanzaro), Gennaro Galasso (CCU, AOU S. Giovanni di Dio e Ruggi D’aragona, Salerno), Nazzareno Galiè (AOU S. Orsola, University of Bologna, Bologna), Massimiliano Gnecchi (Policlinico S. Matteo, Univeristy of Pavia, Pavia), Paolo Golino (CCU, University Vanvitelli, Naples), Bruno Golia (CCU, Clinica Mediterranea, Naples), Pasquale Guarini (Villa dei Fiori Hospital, Acerra), Ciro Indolfi (AOU Mater Domini, Magna Graecia University, Catanzaro), Sergio Leonardi (Policlinico S. Matteo, Univeristy of Pavia, Pavia), Nicola Locuratolo (CCU, Ospedale S. Paolo, Bari), Francesco Luzza (AOU Policlinico G. Martino, University of Messina, Messina), Vincenzo Manganiello (CCU, AO S. Giuseppe Moscati, Aversa), Maria Francesca Marchetti (CCU, AOU D. Casula, Monserrato), Giancarlo Marenzi (Centro Cardiologico Monzino, IRCCS and Department of Biomedical and Clinical Sciences ‘Luigi Sacco’, University of Milan, Milan), Alberto Margonato (CCU, Ospedale San Raffaele, University of Milan, Milan), Luigi Meloni (CCU, University Cagliari, Cagliari), Marco Metra (Spedali Civili, Brescia University, Brescia), Marco Milo (CCU, ASU GI, University of Trieste, Trieste), Annalisa Mongiardo (AOU Mater Domini, Magna Graecia University, Catanzaro), Luca Monzo (Policlinico Casilino, Rome), Carmine Morisco (CCU, AOU Policlinico Federico II, Federico II University, Naples), Savina Nodari (Spedali Civili, Brescia University, Brescia), Giuseppina Novo (CCU, AOUP P. Giaccone, University Palermo, Palermo), Stefano Pancaldi (UTIC 1, AOU S. Orsola, University of Bologna, Bologna), Matteo Parollo (CCU, CCU AOU Pisana, University of Pisa), Giovanni Paternò (CCU, AO S. Carlo, Potenza), Giuseppe Patti (CCU, Ospedale Maggiore, UPO, Novara), Silvia Priori (Policlinico S. Matteo, Univeristy of Pavia, Pavia), Amelia Ravera (CCU, AOU S. Giovanni di Dio e Ruggi D’aragona, Salerno), Antonio Giuseppe Rebuzzi (CCU, Policlinico A. Gemelli, Catholic University, Rome), Massimo Rossi (CCU, Ospedale di Locri), Marino Scherillo (CCU, AORN S. Pio, Benevento), Franco Semprini (UTIC 1, AOU S. Orsola, University of Bologna, Bologna), Michele Senni (CCU, ASST Papa Giovanni XXIII, Bergamo), Gerolamo Sibilio (CCU, AO S. Maria delle Grazie, Pozzuoli), Gianfranco Sinagra (CCU, ASU GI, University of Trieste, Trieste), Massimo Siviglia (Bianchi Melacrino Morelli Hospital, Reggio Calabria), Corrado Tamburino (CCU, University of Catania), Gianfranco Tortorici (UTIC, Ospedale Bentivoglio, AUSL Bologna, Bologna), Francesco Versace (CCU, Ospedale S. Maria Goretti, Latina), Bruno Villari (CCU, AO ‘Fatebenefratelli’, Benevento), Massimo Volpe (CCU, AO Sant’Andrea University Hospital, Rome).
Conflict of interest: none declared.
Contributor Information
Società Italiana di Cardiologia and the CCU Academy investigators group:
Filippo Angelini, Francesco Barillà, Antonio Bartorelli, Francesco Benedetto, Paola Bernabò, Leonardo Bolognese, Martina Briani, Luisa Cacciavillani, Alice Calabrese, Paolo Calabrò, Luigi Caliendo, Leonardo Calò, Gianni Casella, Gavino Casu, Claudio Cavallini, Quirino Ciampi, Marco Ciccone, Michele Comito, Elena Corrada, Filippo Crea, Antonello D’Andrea, Maurizio D’Urbano, Raffaele De Caterina, Gaetano De Ferrari, Roberto De Ponti, Alessio Della Mattia, Carlo Di Mario, Luca Donnazzan, Giovanni Esposito, Francesco Fedele, Alessandro Ferraro, Gennaro Galasso, Nazzareno Galiè, Massimiliano Gnecchi, Paolo Golino, Bruno Golia, Pasquale Guarini, Ciro Indolfi, Sergio Leonardi, Nicola Locuratolo, Francesco Luzza, Vincenzo Manganiello, Maria Francesca Marchetti, Giancarlo Marenzi, Alberto Margonato, Luigi Meloni, Marco Metra, Marco Milo, Annalisa Mongiardo, Luca Monzo, Carmine Morisco, Savina Nodari, Giuseppina Novo, Stefano Pancaldi, Matteo Parollo, Giovanni Paternò, Giuseppe Patti, Silvia Priori, Amelia Ravera, Antonio Giuseppe Rebuzzi, Massimo Rossi, Marino Scherillo, Franco Semprini, Michele Senni, Gerolamo Sibilio, Gianfranco Sinagra, Massimo Siviglia, Corrado Tamburino, Gianfranco Tortorici, Francesco Versace, Bruno Villari, and Massimo Volpe
References
- 1. Onder G, Rezza G, Brusaferro S.. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 2. Indolfi C, Spaccarotella C.. The outbreak of COVID-19 in Italy: fighting the pandemic. JACC Case Rep 2020;doi 10.1016/j.jaccas.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCloskey B, Zumla A, Ippolito G, Blumberg L, Arbon P, Cicero A, Endericks T, Lim PL, Borodina M; WHO Novel Coronavirus-19 Mass Gatherings Expert Group. Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. Lancet 2020;395:1096–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gagliano A, Villani PG, Cò FM, Manelli A, Paglia S, Bisagni PAG, Perotti GM, Storti E, Lombardo M.. 2019-ncov’s epidemic in middle province of northern Italy: impact, logistic & strategy in the first line hospital. Disaster Med Public Health Prep 2020;24:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hartikainen TS, Sörensen NA, Haller PM, Goßling A, Lehmacher J, Zeller T, Blankenberg S, Westermann D, Neumann J.. Clinical application of the 4th Universal Definition of Myocardial Infarction. Eur Heart J 2020;doi: 10.1093/eurheartj/ehaa035. [DOI] [PubMed] [Google Scholar]
- 6. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD.. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020; doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodriguez-Leor O, Cid-Alvarez B, Ojeda S, Martin-Moreiraa J, Rumoroso JR, Lopez-Palop R, Serrador A, Cequier A, Romaguera R, Cruz I, Perez de Prado A, Moreno R, en nombre de todos los participantes del Registro de Codigo Infarto de la ACI-SEC. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiologia intervencionista en Espana. REC Interv Cardiol 2020;doi.org/10.24875/RECIC.M20000120. [Google Scholar]
- 8. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, Lam YM, Chan C, Tsang TC, Tsui M, Tse HF, Siu CW.. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cenko E, van der Schaar M, Yoon J, Manfrini O, Vasiljevic Z, Vavlukis M, Kedev S, Miličić D, Badimon L, Bugiardini R.. Sex-related differences in heart failure after ST-segment elevation myocardial infarction. J Am Coll Cardiol 2019;74:2379–2389. [DOI] [PubMed] [Google Scholar]
- 10. Wijns W, Naber CK.. Reperfusion delay in patients with high-risk ST-segment elevation myocardial infarction: every minute counts, much more than suspected. Eur Heart J 2018;39:1075–1077. [DOI] [PubMed] [Google Scholar]
- 11. Stehli J, Martin C, Brennan A, Dinh DT, Lefkovits J, Zaman S.. Sex differences persist in time to presentation, revascularization, and mortality in myocardial infarction treated with percutaneous coronary intervention. J Am Heart Assoc 2019;8:e012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267–315. [DOI] [PubMed] [Google Scholar]
- 13. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119–177. [DOI] [PubMed] [Google Scholar]
- 14. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165. [DOI] [PubMed] [Google Scholar]
- 15. Cosentino N, Assanelli E, Merlino L, Mazza M, Bartorelli AL, Marenzi G.. An in-hospital pathway for acute coronary syndrome patients during the COVID-19 outbreak: initial experience under real-world suboptimal conditions. Can J Cardiol 2020;doi.org/10.1016/j.cjca.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


