A 50-year-old woman was admitted to the Accident & Emergency department of Baqiyatallah hospital in Tehran (Iran), with symptoms of fever, dyspnoea, dry cough, and fatigue for the past 4 days.
At physical examination, she had enhanced body temperature (38.1 °C), a heart rate of 100 b.p.m., a respiratory rate of 22 breaths/min, and O2 saturation of 92%. Laboratory tests revealed an increased white blood cell count (WBC = 13.5 × 103/μL), increased platelets (PLT = 475× 103/μL), polynuclear (80%); partial thromboplastin time (PTT = 5 s), PTLab/INRLab (=1.31 s); prothrombin test (PT = 18.2 s); and D-dimer (10 ng/mL). Further elevated values were found for C-reactive protein (CRP = 30.3 mg/L), erythrocyte sedimentation rate (ESR = 57 mm/h); serum glutamic-pyruvic transaminase (SGPT = 108 μL); lactate dehydrogenase (LDH = 983μL); and amylase serum (278 μL). Reverse transcription–PCR for COVID-19 was positive and the patient was given oxygen and treated with hydroxychloroquine, dimenhydrinate, and naproxen.
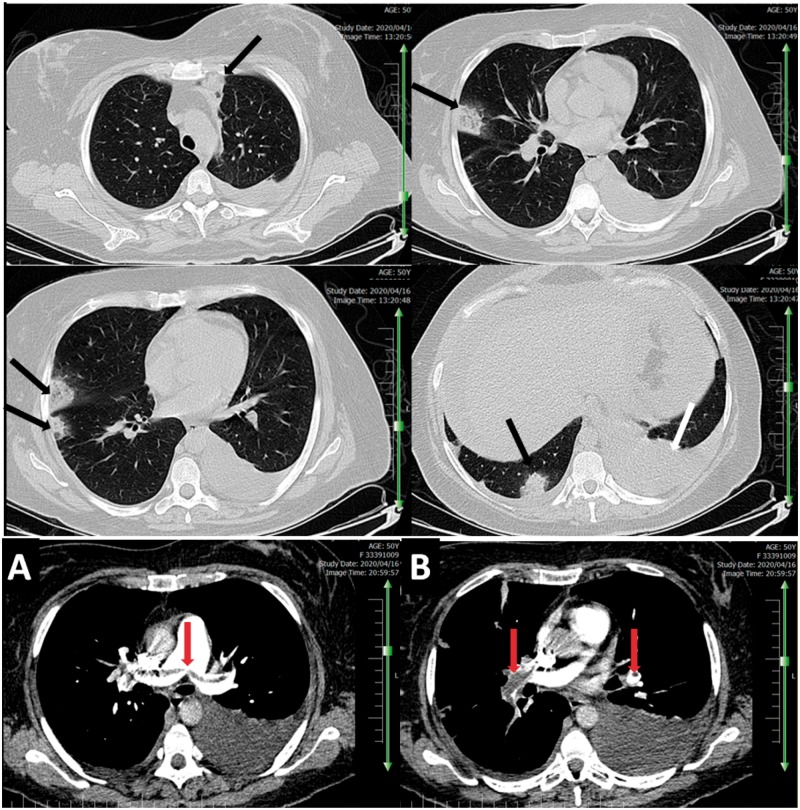
On day 2 after admission, a chest CT scan without contrast evidenced bilateral diffuse multiple patchy and subpleural consolidations with left pleural effusion—radiological findings consistent with COVID-19 pneumonia (Panel A). On day 3 following admission, the patient suddenly developed severe dyspnoea, with O2 saturation decreasing to 74%. A chest computed tomography angiography (CTA) was performed, which revealed a large saddle pulmonary embolism in the main pulmonary artery (MPA), right pulmonary artery (RPA), and left pulmonary artery (LPA) (Panel B). From day 3 of hospitalization, the patient received anticoagulation therapy with heparin and antithrombotic treatment.
The patient remained in hospital for a further 7 days before being discharged in stable condition, with O2 saturation increased to 98%, body temperature of 37.2 °C, negative PCR, and normal laboratory tests.