During this COVID-19 outbreak, doctors stressed the need to ensure the safety of staff during management of the airway in patients. Then some experts published a viewpoint paper entitled ‘COVID-19 outbreak: less stethoscope, more ultrasound’.1 There’s nothing wrong with that. However, this viewpoint may mislead doctors to abandon their stethoscopes. The reasons to abandon were: first, many medical workers were infected during the epidemic, so they were afraid to get close to the patients. At the same time, it is not practical for medical staff to use conventional stethoscopes after wearing protective clothing; and secondly, ultrasound equipment can not only be handheld, but also provides detection data and imaging.1
As the largest military hospital participating in the first-line treatment of COVID-19, we have been working for >60 days from the outbreak. Based on our clinical experience, we would like to emphasize: do not discard the stethoscope from your hands during the COVID-19 outbreak. The reasons are as follows.
First, patients with COVID-19 are not allowed to be accompanied by their families as there is a risk of cross-infection during hospitalization. At the same time, patients are often afraid of this disease because of a higher mortality rate. They therefore need more humane care. The stethoscope can serve as a bridge between doctor and patient and is more than just an instrument for diagnosis. It allows for interaction with our patients, to listen to their histories, their lifestyles, and their bodies, at this time. Auscultation can shorten the distance between doctors and patients, which makes it easier to gain their trust and establish a better doctor–patient relationship.2
Secondly, there is a trend in some countries nowadays of specialization between ultrasound physicians and clinicians. If ultrasound doctors are called to the bedside this may lead to an increased risk of infection by COVID-19. The virus may also be carried by the ultrasound doctor to the next patient who also needs a bedside ultrasound examination. Additionally, some non-infectious disease doctors such as ultrasound physicians have only participated in the front line of an anti-epidemic after brief training in some areas where medical resources are scarce. In these difficult times, it may be not be possible to have sufficient ultrasound doctors to perform the examinations needed.
Thirdly, auscultation of the lungs to determine whether the lungs are infected is the doctor’s first procedure. Relying on equipment is often not suitable without first making a detailed physical examination, as this could lead to misdiagnoses.3 Fuster listed six instances where a stethoscope showed, and an ultrasound missed, a diagnosis at his own clinic in 48 h.2 Specifically, the stethoscope can dynamically understand the progression of pneumonia with COVID-19 while the ultrasound cannot. In reality, much time is needed to train medical practitioners in depth, in order to obtain high ultrasound diagnostic accuracy. Additionally, community hospitals or remote village clinic doctors do not have enough knowledge of ultrasound medicine.
Fourthly, there is a need to find the cause immediately, instead of searching for ultrasound equipment in clinical emergencies. For example, the patient is suddenly obstructed by dried mucus plugs whilst on a ventilator. It is the stethoscope as a diagnostic tool near the bed or worn on us, not the ultrasound equipment, that would save his/her life at that critical moment. Also, using a stethoscope may make it easier than using ultrasound equipment to determine if a gastric tube is in the stomach or not.
Fifthly, doctors need to give a preliminary diagnosis after making a complete physical examination, instead of producing a cold and expensive examination list. Examination using expensive equipment is not suitable for preliminary diagnosis or real-time monitoring of patients. Mosby’s Medical and Nursing Dictionary defines the physical examination as: ‘An investigation of the body to determine its state of health using any or all of the techniques of inspection, palpation, percussion, auscultation, and olfaction. The physical examination, medical history, and initial laboratory tests constitute the data base on which a diagnosis is made and on which a plan of treatment is developed’.4
Last, but not least, handheld ultrasound equipment or the ultrasound pocket device are expensive, and so they would not be owned by every community hospital or remote village clinic doctor. However, these doctors battled in the front line of epidemic prevention and were also faced with a higher risk of infection every day.
We would like to share a method for preparing a simple substitute to the traditional stethoscope. This simple stethoscope can be prepared with a sterilized paper tube around an empty potato chips cylindrical packet. It can be placed on each bed to prevent cross-contamination. It is economical, safe, and free (Figures 1–3), and none of our medical workers had been infected with SARS-CoV-2.
Figure 1.
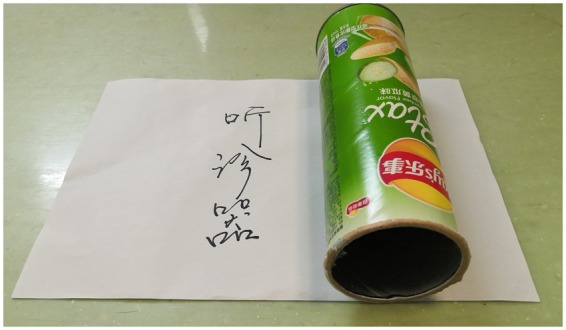
A simple stethoscope made using an empty potato chips cylinder (20–30 cm × 5–8 cm) covered by a piece of sterile A4 paper.
Figure 2.
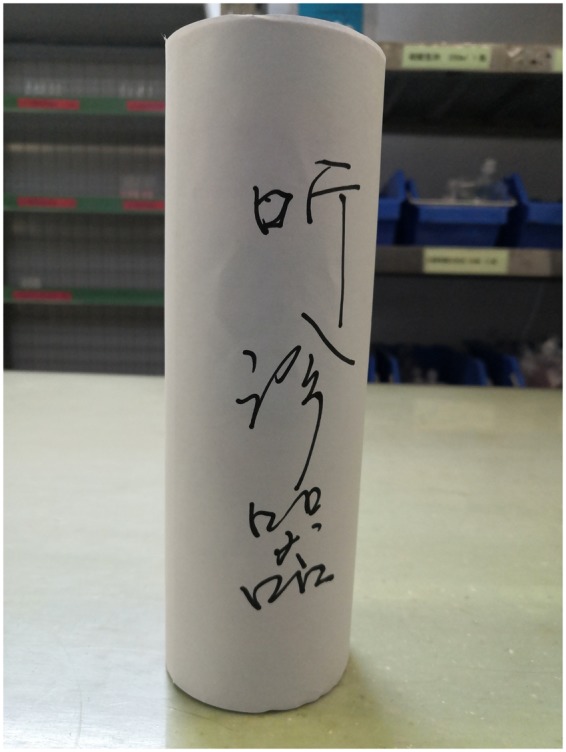
This simple stethoscope would be placed at the end of the bed with an eye-catching label after being disinfected.
Figure 3.

In use to detect bronchospasm which is impossible to detect by ultrasound equipment.
In addition, we would like to mention some knowledge of new equipment. Contactless stethoscopes have been invented with the sounds collected and analysed directly through computers with the development of technology. What needs to be advocated is Bluetooth earphones. The new device is in two parts, a built-in Bluetooth drum and earplugs. The earplugs can be inserted into the ear before wearing protective clothing; sounds are transmitted wirelessly by the built-in Bluetooth drum. However, the stethoscope should not be thrown away during the COVID-19 outbreak.
Conflict of interest: none declared.
References
References are available as supplementary material at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


