Abstract
Aim
To assess the impact of COVID-19-related lockdown in India on alcohol-dependent persons.
Method
We examined the change in the incidence of severe alcohol withdrawal syndrome presenting to hospitals in the city of Bangalore.
Results
A changepoint analysis of the time series data (between 01.01.20 to 11.04.20) showed an increase in the average number of cases from 4 to 8 per day (likelihood ratio test: χ2 = 72, df = 2, P < 0.001).
Conclusion
An unintended consequence of the lockdown was serious illness in some patients with alcohol use disorders.
INTRODUCTION
At the time of this writing, at least 1.9 million individuals in 184 out of 193 countries have suffered from coronavirus disease 2019 (COVID-19), and 0.1 million have succumbed to it (Centre for Systems Science and Engineering, 2020). In an attempt to control the spread of infection, most countries have restricted movement and curtailed business (‘lockdown’), including the closure of alcohol vends (Juliana Kaplan, 2020). An unintended (but not unforeseeable) consequence of this ‘dry period’ could be an increase in the incidence of severe alcohol withdrawal syndrome (AWS) (Schuckit, 2014).
In India, the production, transport, sale and limit of personal possession of beverages with more than 0.5 per cent are regulated by state excise laws (Monika Arora, 2013). These laws allow the government to prohibit functioning of alcohol vends, pubs and traditional liquor outlets by issuing an order. Contravention of excise orders attracts criminal proceedings. For example, in the state of Karnataka, sale of liquor during prohibition attracts imprisonment up to 5 years (Karnataka Excise Act, 1965). Thus, state governments can effect an alcohol ban at short notice. We have previously reported how an alcohol ban in the context of elections led to an increase in the incidence of AWS (Narasimha et al., 2018).
The first COVID-19 case in India was reported on 30 January 2020. The government of India instituted a 21-day lockdown on 24 March 2020. The exempted activities include those related to food, groceries, healthcare, communication and basic amenities. Even before this, the state of Karnataka went into lockdown on the evening of 21 March 2020. During the lockdown, all states and union territories banned alcohol.
Alongside, health services have undergone two significant changes to prevent COVID-19 transmission. First, non-emergency services have been shut down (Ministry of Health and Family Welfare, 2020a). Second, patients suspected with COVID-19 are seen only in dedicated hospitals or earmarked areas of a non-dedicated hospital (Ministry of Health and Family Welfare, 2020b).
In this background, we report the changes in the incidence of severe AWS presenting to psychiatry emergency services, following non-availability of alcohol due to the COVID-19 lockdown. We specifically focus on alcohol withdrawal seizures, delirium tremens (DT) and withdrawal hallucinosis. While withdrawal hallucinosis is not considered a complicated withdrawal state, in our practice it is associated with a high risk of self-harm and progression to delirium tremens (Narasimha et al., 2019).
METHODS
Data were collected from the psychiatry emergency services of a government-funded tertiary-level hospital in Bangalore, National Institute of Mental Health and Neurosciences. Bangalore is a metropolitan city with an estimated population of 12.3 million; it is the capital of the southern state of Karnataka.
We collected the number of emergency department (ED) visits per day for alcohol withdrawal seizures (F 10.31), delirium tremens (F 10.40 and F 10.41) and alcohol withdrawal hallucinosis (F 10.52) between 01 January 2020 to 11 April 2020 (102 days) (WHO, 1992). We hypothesized that the number of ED visits for severe AWS would change following the onset of lockdown on 22 March 2020. To empirically test this hypothesis, we have used a changepoint analysis to examine the presence of distinct segments in the time series. Changepoint detection is an established method of detecting disease outbreaks (Texier et al., 2016). We have used binary segmentation with a minimum segment length of 7 days to identify a maximum of five segments, the type of penalty is Bayes’ information criterion (BIC), and the number of daily visits is modelled with Poisson distribution (Killick and Eckley, 2014). Analyses are done in R software with ‘changepoint’ package. We must note that events with low counts do not follow a normal distribution; therefore, we cannot compare the mean number of visits between pre-lockdown and post-lockdown period to draw an inference.
To rule out a ‘time of the year’ effect due to cultural or economic reasons, we graphically compare the number of ED visits with severe AWS between 01 March 2019 and 11 April 2019 and the corresponding dates in 2020.
RESULTS
Change in the number of severe AWS cases
As shown in Fig. 1, the time series (count vs date) consists of three segments with a substantial difference in the mean number of severe AWS cases per day (denoted with μ). Segment 1 (January 1 to March 22) shows the usual (μ1 = 4) number of severe AWS cases. Following the lockdown on 22 March 2020, there is an increase in the counts (μ2 = 8) which is followed by the current period where the counts are lower than usual (μ3 < 1). Also, there is no corresponding peak last year, which rules out a recurring phenomenon.
Fig. 1.
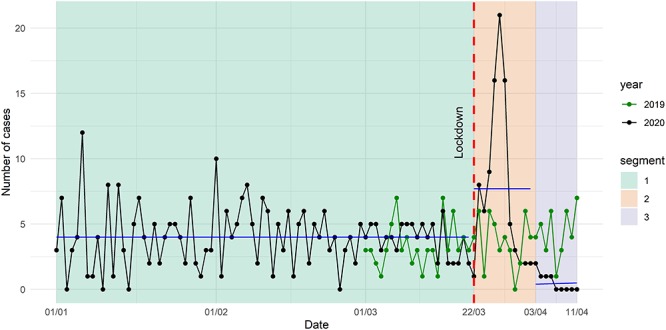
Change in the number of severe alcohol withdrawal syndrome cases (delirium tremens, seizures and hallucinosis) seen in the emergency department following COVID-19-related lockdown. Blue solid lines show the mean number of visits in each segment during the year 2020; on the evening of 21 March 2020 (red interrupted line).
The BIC of an intercept-only model (y ~ 1, family = Poisson) is 556 (df = 101) with residual deviance of 256. The BIC of a three-segment model (y ~ 1|segment, family = Poisson) is 488 (df = 99) with a residual deviance of 187. The likelihood ratio test shows that a three-segment model is significantly more likely (χ2 = 72, df = 2, P < 0.001).
Sociodemographic and clinical profile of the patients
Ninety-six, middle-aged (mean [M] = 43 and standard deviation [SD] = 9 years) male patients suffering from severe AWS have sought help between 22 March 2020 and 11 April 2020 as compared to 79 cases between 01 March 2020 and 21 March 2020. DT with or without seizures was the most common presentation (N = 77, 80%), followed by withdrawal seizures (N = 16, 17%) and withdrawal hallucinosis (N = 12, 12%). A majority of these patients (N = 73, 76%) belonged to below poverty line (i.e. were deemed in need of nutritional support and other welfare schemes by the government). All patients reported daily heavy alcohol use (M = 18, SD = 4 standard units of alcohol).
A majority of these patients (N = 92, 95%) reported COVID-19-related lockdown as the reason for cessation of alcohol use; head injury (N = 2) and vomiting (N = 2) were the reason for the remaining four patients. Case notes reflect that a majority (N = 77, 80%) reported closure of alcohol vends as the specific reason for cessation.
Importantly, most of the DT patients were very sick at the time of presentation. Three had a history of head injury, four had symptoms suggestive of Wernicke’s encephalopathy, and all had signs of dehydration. Worryingly, 42% of these patients (N = 40) had at least one of these symptoms: fever, cough, shortness of breath, vomiting or diarrhoea and sore throat or rhinitis.
DISCUSSION
Lockdown in Karnataka commenced on 21 March 2020. We analysed the pattern of treatment-seeking for severe AWS in our ED between 01 January 2020 and 11 April 2020. Using a changepoint analysis, we could demonstrate that the pattern of severe AWS-related visits changed significantly. The first changepoint coincided with the onset of lockdown and heralded a significant increase in the number of visits. The second changepoint is on 03 April 2020, marking a decrease in severe AWS-related visits reflecting the natural course of alcohol withdrawal. Before discussing the implications of these findings, we must consider explanations unrelated to COVID-19.
We do not see a similar pattern in the month of March and April of 2019; this rules out a seasonal trend. Theoretically, if several health facilities stop functioning, there can be a displacement of caseload to the remaining facilities. However, the majority of these patients are below the poverty line, and it is unlikely that they would have chosen private hospitals in normal times. We note that 70–75% of patients seen in our outpatient, inpatient and ED come from below the poverty line. To our knowledge, EDs in all government hospitals in the city of Bangalore are functioning. Most patients reported the alcohol ban during lockdown as the reason for abrupt cessation. Travel restrictions and unavailability of routine medical care likely prevented some of these patients from seeking medical attention at an earlier stage. Informal sources of alcohol are widespread in India; the current lockdown is perhaps affecting these clandestine operations also (see Benegal, 2005). In summary, multiple effects of COVID-19 related to lockdown are the likely explanation of our findings. Media reports from other parts of the country indicate suicides (Jayakumar, 2020), liquor theft (Haider, 2020) and deaths due to consumption of toxic alcohol (G.C. Shekhar, 2020). Similar concerns have emerged from Thailand after the unavailability of alcohol during lockdown (Saengow, 2020).
COVID-19 pandemic and the measures to contain it will have profound effects on the epidemiology and the treatment gap of addictive disorders (Marsden et al., 2020). Justifiably the focus of the field is on protocols for opioid substitution therapy (Ali et al., 2020); we aver that severe alcohol withdrawal is an equal, if not a more pressing concern. We show that following lockdown, EDs may have to cope with twice the usual number of severe AWS cases for up to 10 days. In addition to taxing already strained ED resources, severe alcohol withdrawal, especially DT, presents many challenges.
First, consider this: a typical DT patient in Karnataka is likely to be an unemployed, probably homeless person suffering from electrolyte abnormalities, structural brain lesions, malnutrition and not in a state to provide travel or contact history (Ferguson et al., 1996; Eyer et al., 2011). In addition to this, vomiting, fever and tachypnoea are commonly seen in DT (Schuckit, 2014). Given this, should the patient be managed as a suspected COVID-19 patient? Depending on the availability of resources and government policies, ED teams managing severe AWS cases will face tough choices. For example, when we faced this surge, our centre did not have in-house testing, and isolation facilities were in the process of being set up. Till 20 March 2020, the government testing strategy was limited to patients with international travel history or close contact with a confirmed case. Although subsequent revisions included all patients with ‘severe acute respiratory illness’, percolation of this guideline and increase in testing capacity lagged for several days. We now know that random samples collected from patients with no history of international travel or close contact with COVID-19 cases were turning out positive as early as 15 February 2020 (Gupta et al., 2020). We were concerned about the crowding in the ED, exposure of other patients and their attenders to patients who were coughing and febrile and safety of the doctors and nurses. As a result of these complexities, we had to discharge most of these patients within 36 hours.
Second, patients with severe AUD are at a higher risk of contracting COVID-19 as they may fail to comply with protective measures. They are also more likely to have a severe form of illness due to comorbid conditions and immunosuppressed state. Therefore, a large number of AUD cases visiting ED in these times are dangerous for patients as well as ED staff.
Third, we are concerned that these patients may fail to get treatment at all. During lockdown public transport is unavailable, health services are in flux, and professionals that do not have Personal Protective Equipment (PPE). will be reluctant to examine and treat patients with respiratory symptoms. There are reports that hospitalizations and quality of care for ST-elevation myocardial infarctions (STEMI) have decreased during COVID-19 pandemic (Tam et al., 2020). AUD patients are even more likely to slip through the cracks as they tend to come from disadvantaged backgrounds and face stigma.
What are the solutions? The solutions will have to be context-specific. For example, Scottish health services disseminated information to guide patients in gauging their risk of severe AWS and planning safe domiciliary detoxification (Scottish Health Action on Alcohol Problems, 2020). This strategy may work in a higher income, well-connected population. Most of our patients reported that they wished to stockpile and gradually reduce, but they did not have the money to buy alcohol on the last day. Nevertheless, planning, foreseeing an increase in severe AWS and ensuring that addiction treatment services are not disrupted are reasonable steps in all settings.
ACKNOWLEDGEMENTS
The authors acknowledge the assistance of Dr. Shruti Nair, Dr. Pawan Kumar Khadse, Dr. Kamaldeep Sadh and Dr. Deepak Ghadigaonkar in the treatment of some of the cases reported in this manuscript.
CONFLICT OF INTEREST
This work has not received any funding support. None of the authors has any conflict of interest to declare.
References
- Ali F., Baldacchino, Alexander M., et al. (2020). COVID-19 and Substance Use Disorders: Recommendations to a Comprehensive Healthcare Response. An International Society of Addiction Medicine (ISAM) Practice and Policy Interest Group Position Paper [Online]. Available: https://figshare.com/articles/COVID-19_and_Substance_Use_Disorders_Recommendations_to_a_Comprehensive_Healthcare_Response/12033567(10 April 2020, date last accessed). [DOI] [PMC free article] [PubMed]
- Benegal V. (2005) India: alcohol and public health. Addiction 100:1051–6. [DOI] [PubMed] [Google Scholar]
- Centre for Systems Science and Engineering (2020). Coronavirus COVID 19 Global Cases [Online] Baltimore, Maryland: John Hopkins University; Available: https://coronavirus.jhu.edu/map.html(10 April 2020, date last accessed). [Google Scholar]
- Eyer F, Schuster T, Felgenhauer N, et al. (2011) Risk assessment of moderate to severe alcohol withdrawal–predictors for seizures and delirium tremens in the course of withdrawal. Alcohol Alcohol 46:427–33. [DOI] [PubMed] [Google Scholar]
- Ferguson JA, Suelzer CJ, Eckert GJ, et al. (1996) Risk factors for delirium tremens development. J Gen Intern Med 11:410–4. [DOI] [PubMed] [Google Scholar]
- Shekhar GC. (2020) Lockdown Impact: From After Shave to Paint Varnish, Alcohol Alternatives Prove Fatal In Tamil Nadu [Online] Outlook Publishing; Available: https://www.outlookindia.com/website/story/india-news-coronavirus-lockdown-impact-from-after-shave-to-pain-varnish-alcohol-alternatives-prove-fatal-in-tamil-nadu/350176(10 April 2020, date last accessed). [Google Scholar]
- Government of Karnataka (1965) Karnataka Excise Act, Section 32 [Online] Available: https://www.lawyerservices.in/Karnataka-Excise-Act-1965-SECTION-32-Penalty-for-illegal-import-etc(10 April 2020, date last accessed).
- Gupta N, Praharaj I, Bhatnagar T, et al. (2020) Severe acute respiratory illness surveillance for coronavirus disease 2019, India. Indian J Med Res [Epub ahead of print]Available: http://www.ijmr.org.in/preprintarticle.asp?id=282179(10 April 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider T. (2020) Coronavirus in India: Liquor thefts on rise while city stays shut [Online] India Today Group; Available: https://www.indiatoday.in/mail-today/story/coronavirus-in-india-liquor-thefts-on-rise-while-city-stays-shut-1664119-2020-04-07(10 April 2020, date last accessed). [Google Scholar]
- Jayakumar 2020. Alcohol Non-Availability Kills More than Coronavirus in KERALA; Foreign Liquor Served as 'Medicine' [Online] India Today Group; Available: https://www.businesstoday.in/current/economy-politics/alcohol-non-availability-kills-more-than-coronavirus-in-kerala-foreign-liquor-served-as-medicine/story/399716.html[Accessed 23.04 2020]. [Google Scholar]
- Juliana Kaplan L. F., Mcfall-Johnsen Morgan (2020). A third of the Global Population is on Coronavirus Lockdown — Here's Our Constantly Updated List of Countries and Restrictions [Online]. New York: Insider Incorporated; Available:https://www.businessinsider.com/countries-on-lockdown-coronavirus-italy-2020-3?IR=T#panama-and-peru-both-implemented-measures-restricting-days-citizens-could-outside-by-gender-6(10 April 2020, date last accessed). [Google Scholar]
- Killick R, Eckley IA (2014) Changepoint: an R package for Changepoint analysis. J Stat Softw 58:19. [Google Scholar]
- Marsden J, Darke S, Hall W, et al. (2020) Mitigating and learning from the impact of COVID-19 infection on addictive disorders. Addiction [Epub ahead of print]. Available: http://www.ncbi.nlm.nih.gov/pubmed/32250482(10 April 2020, date last accessed). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare 2020a. Advisory for Hospitals and Medical Education Institutions [Online] New Delhi: Government of India; Available: https://www.mohfw.gov.in/pdf/AdvisoryforHospitalsandMedicalInstitutions.pdf(10 April 2020, date last accessed). [Google Scholar]
- Ministry of Health and Family Welfare 2020b. Guidance document on appropriate management of suspect/confirmed cases of COVID19 [Online] New Delhi: Government of India; Available: https://www.mohfw.gov.in/pdf/FinalGuidanceonMangaementofCovidcasesversion2.pdf10 April 2020, date last accessed). [Google Scholar]
- Monika Arora P. D., Nazar Gaurang, Gupta Himanshu, et al. 2013. Alcohol Marketing and Regulatory Policy Environment in India [Online] New Delhi: Public Health Foundation of India; Available: https://iogt.org/wp-content/uploads/2013/12/PHFI-Alcohol-Industry-Report.pdf(10 April 2020, date last accessed). [Google Scholar]
- Narasimha VL, Mukherjee D, Shukla L, et al. (2018) Election bans and alcohol banes: The impact of elections on treatment referrals at a tertiary addiction treatment facility in India. Asian J Psychiatr 38:27–8. [DOI] [PubMed] [Google Scholar]
- Narasimha VL, Patley R, Shukla L, et al. (2019) Phenomenology and course of alcoholic Hallucinosis. J Dual Diagn 15:172–6. [DOI] [PubMed] [Google Scholar]
- Tam CF, Cheung KS, Lam S, et al. (2020) Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes Circoutcomes120006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Texier G, Farouh M, Pellegrin L, et al. (2016) Outbreak definition by change point analysis: A tool for public health decision? BMC Med Inform Decis Mak 16:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saengow U. (2020) Rapid response: nationwide alcohol sales ban during COVID-19 pandemic: unique opportunity for epidemiology and alcohol policy. BMJ 369:m1439.32269023 [Google Scholar]
- Schuckit MA. (2014) Recognition and management of withdrawal delirium (delirium tremens). N Engl J Med 371:2109–13. [DOI] [PubMed] [Google Scholar]
- Scottish Health Action on Alcohol Problems (2020) Coronavirus (COVID-19) Pandemic: Advice for Heavy Drinkers on Cutting Back or Stopping Drinking Alcohol [Online] Available: https://www.shaap.org.uk/downloads/240-covid-advice-for-heavy-drinkers/download.html(10 April 2020, date last accessed).
- World Health Organisation (1992) ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organisation. [Google Scholar]


