A 64-year-old male, with no known cardiovascular risk factors, was brought to the Emergency Room with an acute ST-elevation myocardial infarction (STEMI). One week before, he was admitted to the hospital because of a COVID-19 bilateral pneumonia treated with lopinavir–ritonavir and hydroxicloroquine, without any antithrombotic prophylaxis, and was discharged after 7 days without specific treatment, because he had made good clinical progress, just hours before he returned to the hospital.
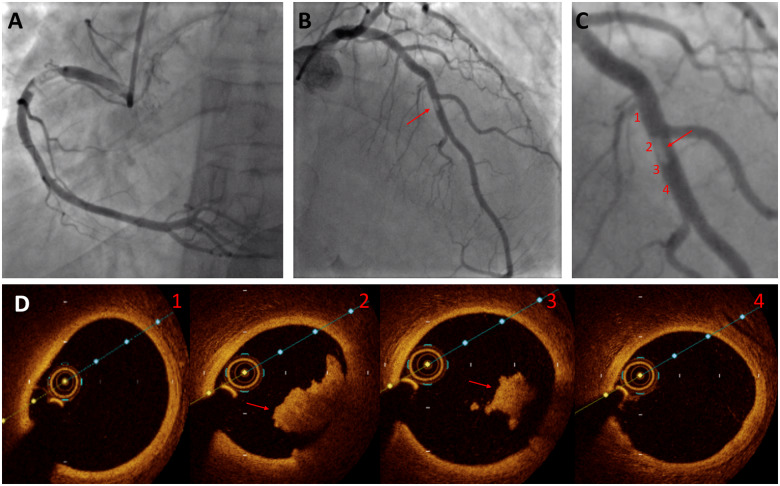
Coronary angiography showed a critical thrombotic stenosis of the proximal right coronary artery (RCA; Panel A) as well as a non-occlusive filling defect compatible with thrombus at the middle segment of the left anterior descending (LAD) coronary artery (Panels B and C). Thrombus aspiration to the RCA was performed, achieving thrombotic material, but significant underlying stenosis persisted so a drug-eluting stent was successfully implanted. Optical coherence tomography (OCT) was performed to the LAD (Panel D; the numbers of each frame show the level of the frame at the LAD as they are shown in Panel C) and confirmed the presence of a non-occlusive thrombus without underlying atherosclerotic plaque. Post-stenting OCT was performed to the RCA without the presence of atheroma. The decision was to manage LAD thrombus medically with low-molecular weight heparin for 7 days in addition to the double antiplatelet therapy. The reverse transcription–PCR for SARS-CoV-2 was still positive.
C-reactive protein was initially raised after the diagnosis of COVID-19 pneumonia and subsequently decreased until the day of STEMI. In contrast, D-dimer and platelets were still increasing on the morning he was discharged, probably indicating abnormal clotting activation which led to the multivessel coronary obstructions. This phenomenon suggests in situ thrombosis as the mechanism, as no significant atheroma was found and the possibility of coronary emboli does not match with the fact that the LAD thrombus was not occlusive (60% stenosis) and it was just attached to the wall. This complication of the SARS-CoV-2 infection has not been reported previously, but it is in consonance with previous reports of increasing thrombotic risk in other vascular territories such as the pulmonary or cerebral circulation.
Supplementary material is available at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.