Abstract
Background
Healthcare workers (HCWs) at the frontline are facing a substantial risk of infection during the coronavirus disease 2019 (COVID-19) outbreak.
Methods
We acquired information and data on general information on and infection and death status of HCWs in Wuhan during the COVID-19 outbreak and completed statistical analyses.
Results
We obtained the data on 2457 infected cases among HCWs in Wuhan, China. More than half of the infected individuals were nurses (52.06%), whereas 33.62% of infected cases were doctors and 14.33% of cases were medical staff. In particular, the case infection rate of nurses (2.22%) was remarkably higher than that of doctors (1.92%). Most infected cases among HCWs were female (72.28%). A majority of the infected HCWs (89.26%) came from general hospitals, followed by specialized hospitals (5.70%) and community hospitals (5.05%). The case infection rate of HCWs (2.10%) was dramatically higher than that of non-HCWs (0.43%). The case fatality rate of HCWs (0.69%) was significantly lower than that of non-HCWs (5.30%).
Conclusions
The infection risk of HCWs is clearly higher than that of non-HCWs. HCWs play an essential role in fighting the pandemic. The analysis of the infection status of HCWs is essential to attract enough attention from the public, provide effective suggestions for government agencies, and improve protective measures for HCWs.
Keywords: healthcare workers, infection, COVID-19
The present study is the first work to investigate the infection status of healthcare workers during the COVID-19 outbreak. The analysis of the infection status of healthcare workers is essential to gain knowledge and improve protective measures.
On 31 December 2019, a series of patients affected with pneumonia of an unknown etiology were identified in Wuhan, China [1]. Subsequently, the disease was named coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) on 12 January 2020 [2]. On 11 March 2020, the WHO announced that the COVID-19 outbreak could be characterized as a “pandemic,” as the highly infectious virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread increasingly worldwide [3]. This is the third serious coronavirus outbreak in less than 20 years, following the severe acute respiratory syndrome (SARS) in 2002–2003 and the Middle East respiratory syndrome (MERS) in 2012 [4, 5]. The number of confirmed cases continues to increase. Globally, on 16 April 2020, there were a total of 1 991 562 reported cases of COVID-19 in 213 countries and 130 885 deaths [6].
Facing a substantial risk of SARS-CoV-2 infection, healthcare workers (HCWs) at the frontline have been fighting COVID-19, saving human lives, with great effort and sacrifices. According to the published articles, a large number of HCWs have been infected with SARS-CoV-2 worldwide, and have even died of COVID-19 [7–9]. The COVID-19 pandemic has a marked impact on the physical and mental health of HCWs [10]. It is crucial to understand that we cannot stop the COVID-19 pandemic without HCWs. Therefore, effective protection for HCWs is currently of the upmost importance.
To the best of our knowledge, no published work on the infection status among HCWs with COVID-19 has been identified so far. In this study, we obtained data from government official reports and carried out a data analysis of the infection status of the HCWs in Wuhan during the COVID-19 outbreak. By conducting this cross-sectional study, we aim to provide some thoughts and recommendations to protect HCWs worldwide.
METHODS
Sources of Data
As of 26 January 2020, the Red Cross Society of China implemented the Humanitarian Aid Fund to provide financial assistance for all the infected and dead HCWs due to COVID-19 nationwide. We retrieved and acquired the data of all infected cases and deaths among HCWs in Wuhan from the HCW lists supported by the Humanitarian Aid Fund from the Red Cross Society of China up until 26 March 2020 (https://www.redcross.org.cn/html/NewsList.html?type=news&cla=newrdjz). We collected the total number of laboratory-confirmed cases and deaths with COVID-19 in Wuhan from publicly available disease databases of the National Health Commission of China (http://www.nhc.gov.cn/xcs/yqtb/list_gzbd_2.shtml). Information on the permanent population in Wuhan, including all the HCWs, originated from the statistical bulletin released by the Wuhan Statistics Bureau, Hubei Province (http://tjj.wuhan.gov.cn/details.aspx?id=4615). All of the HCWs from other parts of China sent to Wuhan to assist were excluded from the present study. According to the scope of the database, all infected cases and deaths among HCWs in Wuhan from the HCW lists supported by the Humanitarian Aid Fund are included in all of the laboratory-confirmed cases and deaths in Wuhan from publicly available disease databases of the National Health Commission of China, who are part of the permanent population in Wuhan reported by the statistical bulletin released by the Wuhan Statistics Bureau. Based on the various sources, we established a dataset after record cleaning, exclusion of duplicate cases, and completion of missing information as described previously [11]. All case records contain national identification numbers and therefore all cases have records in the dataset and no records are duplicated.
The case infection rate (CIR) was defined as the percentage of the cumulative number of laboratory-confirmed COVID-19 infections divided by the total number of HCWs or non-HCWs in Wuhan. The case fatality rate (CFR) was defined as the percentage of the cumulative number of deaths divided by the total number of laboratory-confirmed COVID-19 infections among HCWs or non-HCWs in Wuhan.
Data collection and analysis of these cases were determined by the National Health Commission of China to be part of an outbreak investigation. The study was thus deemed exempt from institutional review board approval.
Definition of COVID-19
All COVID-19 cases were confirmed based on the diagnostic criteria of the recommendations by the National Health Commission of China (http://www.nhc.gov.cn/xcs/zhengcwj/202003/4856d5b0458141fa9f376853224d41d7/files/4132bf035bc242478a6eaf157eb0d979.pdf). According to the national diagnostic criteria, a confirmed case was defined as both (1) fulfilling 2 clinical criteria plus 1 epidemiological clue, or all 3 clinical criteria, and (2) having throat-swab specimens that tested positive for SARS-CoV-2 using real-time reverse transcriptase–polymerase chain reaction (RT-PCR) assay. The clinical criteria were as follows: (1) fever and/or symptoms of acute respiratory infection, (2) radiographic evidence of pneumonia, and (3) low or normal white blood cell count or low lymphocyte count. Epidemiological clues included the following: (1) residence in Wuhan city within 14 days prior to symptom onset; (2) close contact with a confirmed or probable case of COVID-19 within 14 days prior to symptom onset; (3) close contact with persons who had fever or symptoms of acute respiratory infection or a local community with reported cases, within 14 days prior to symptom onset; and (4) if a cluster of persons with similar symptoms was identified [12]. The laboratory protocol for SARS-CoV-2 real-time RT-PCR assay was described previously [13]. All the HCW and non-HCW cases were laboratory confirmed as described previously [8, 14]. The tests were screened by Wuhan Center for Disease Control (CDC) and confirmed by Hubei Provincial CDC.
Statistical Analysis
The confirmed COVID-19 cases among HCWs were categorized according to the following parameters: sex, occupation type, hospital type, infection status, and death status. The occupation types of HCWs include nurses, doctors, and medical staff. Medical staff are defined as other HCWs working in hospitals except for nurses and doctors, such as pharmacists, laboratory technicians, and medical imaging technicians. Categorical variables are represented as frequencies and percentages and were analyzed by χ 2 test or Fisher’s exact test. All statistical analyses were performed using SPSS (Statistical Package for the Social Sciences) version 23.0 software (SPSS, Inc). A 2-sided α of less than .05 was considered statistically significant. The analyses were adjusted for multiple comparisons for type I error with Bonferroni adjustment approaches.
RESULTS
In early 2020, the population was 11.212 million people in Wuhan, and there were 117 100 HCWs, including 43 100 doctors, 57 700 nurses, and 16 300 medical staff. As of 26 March 2020, a total of 50 006 infected cases were confirmed in Wuhan, and the Humanitarian Aid Fund provided humanitarian assistance for 2457 HCWs from 145 hospitals in Wuhan. Among the 2457 HCWs, 17 died of COVID-19.
Demographic data and general information on infection status are summarized in Table 1. A total of 72.28% of the HCWs were female. More than half of the infected individuals were nurses (52.06%), while 33.62% of infected cases were doctors and 14.33% of cases were medical staff. A majority of the infected HCWs (89.26%) came from general hospitals, followed by specialized hospitals (5.70%) and community hospitals (5.05%) (Table 1).
Table 1.
General Information on the Infection Status of Healthcare Workers in Wuhan
| Parameters | Total, N | Confirmed Cases, n (%) | CIR, % | χ 2 | P |
|---|---|---|---|---|---|
| Sex | 0.289 | .591 | |||
| Female | 84 078 | 1776 (72.28) | 2.11 | ||
| Male | 33 022 | 681 (27.72) | 2.06 | ||
| Types of occupation | 11.168 | .004a | |||
| Nurse | 57 700 | 1279 (52.06) | 2.22 | 10.871 | .001b |
| Doctor | 43 100 | 826 (33.62) | 1.92 | 3.594 | .058c |
| Medical staff | 16 300 | 352 (14.33) | 2.16 | 0.192 | .661d |
| Types of hospital | 699.034 | <.001e | |||
| General hospital | 74 944 | 2193 (89.26) | 2.93 | 262.406 | <.001f |
| Specialized hospital | 17 565 | 140 (5.70) | 0.80 | 14.114 | <.001g |
| Community hospital | 24 591 | 124 (5.05) | 0.50 | 477.685 | <.001h |
Abbreviation: CIR, case infection rate.
aDenotes a comparison among 3 types of occupations.
bDenotes a comparison between nurses and doctors.
cDenotes a comparison between doctors and medical staff.
dDenotes a comparison between nurses and medical staff.
eDenotes a comparison among 3 types of hospitals.
fDenotes a comparison between general hospital and specialized hospital.
gDenotes a comparison between specialized hospital and community hospital.
hDenotes a comparison between general hospital and community hospital.
Our findings showed that no statistically significant difference was found in the CIR of HCWs by sex (P = .591). There was a statistically significant difference in the CIR among 3 types of occupation and hospital (P = .004 and P < .001, respectively). The CIR of doctors was statistically significantly lower than that of nurses (P = .001), while the CIR was similar but not statistically significantly different between nurses and medical staff or between doctors and medical staff (P = .661 and P = .058, respectively). The CIR of specialized hospitals or community hospitals was remarkably lower than that of general hospitals (P < .001 and P < .001, respectively), while the CIR of community hospitals was clearly lower than that of specialized hospitals (P < .001) (Table 1). The CIR of HCWs was dramatically higher than that of non-HCWs (P < .001). The CFR of HCWs was significantly lower than that of non-HCWs (P < .001) (Table 2).
Table 2.
Comparison of Case Infection Rate and Case Fatality Rate Between Healthcare Workers and Non–Healthcare Workers in Wuhan
| Parameters | Non-HCWs | HCWs | χ 2 | P |
|---|---|---|---|---|
| Infection status | ||||
| Infected individuals, n | 475 49 | 2457 | 7275.207 | <.001 |
| Noninfected individuals, n | 11 047 351 | 114 643 | ||
| CIR, % | 0.43 | 2.10 | ||
| Death status | ||||
| Deaths due to infection, n | 2518 | 17 | 102.890 | <.001 |
| No deaths due to infection, n | 45 031 | 2440 | ||
| CFR (%) | 5.30 | 0.69 |
Abbreviations: CFR, case fatality rate; CIR, case infection rate; HCW, healthcare worker.
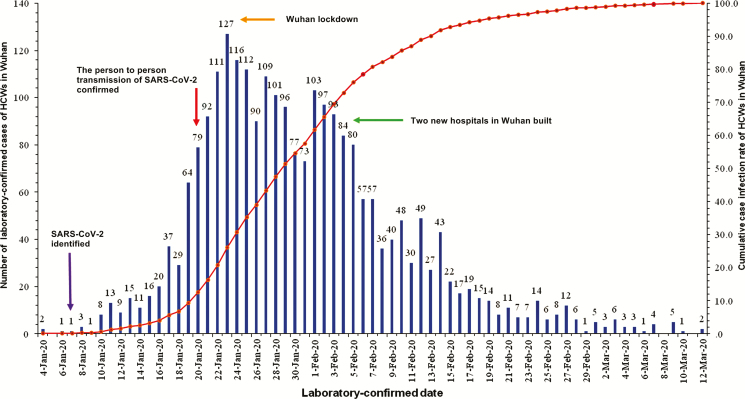
Figure 1 shows the distribution of laboratory-confirmed date and case number for HCWs affected with COVID-19. The majority of cases were confirmed between 20 January 2020 and 5 February 2020, while a few cases (<10) were daily confirmed after 28 February 2020.
Figure 1.
Laboratory-confirmed date and cumulative case number of HCWs with COVID-19 in Wuhan from 4 January to 12 March 2020. Daily numbers of laboratory-confirmed cases are plotted by date of laboratory confirmation (blue) and cumulative percentage of laboratory-confirmed cases (red). Major epidemic response actions taken by the Chinese government are shown in arrows of different colors. Abbreviation: COVID-19, coronavirus disease 2019; HCW, healthcare worker; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
DISCUSSION
The present study provides the first insight into the infection status of HCWs in Wuhan during the COVID-19 outbreak. Healthcare workers had a significantly higher CIR than non-HCWs. In particular, the CIR of nurses was higher than that of doctors, suggesting differential effects of occupation types on infection status. It is known that nurses have more patient-contact time in general hospitals than doctors. In the early phase of the COVID-19 outbreak, the numbers of HCWs and personal protective equipment (PPE) were both insufficient, and the continuous working hours of HCWs were relatively longer. Therefore, the HCWs were exhausted physically and mentally. In this situation, decreased immunity and increased chance of infection could occur in HCWs. Therefore, it is recommended that HCWs at the frontline receive sufficient rest time to ensure adequate sleep, avoid overwork, and consume a nutritious diet and supplements to ensure adequate nutrition to increase body immunity and reduce the likelihood of infection.
The majority of infected HCWs in Wuhan worked in general hospitals. However, the CIR of HCWs in specialized and community hospitals was relatively low in Wuhan. This result in our study is consistent with that of some previous studies from a stomatological hospital, a women’s and children’s hospital, and an infectious disease hospital [14–16]. A potential explanation may be that routine use of PPE in specialized hospitals, including face shields, goggles, medical masks, and gloves, prevented further transmission of SARS-CoV-2 and limited cross-infection. Another potential explanation may be that fewer cases in community and specialized hospitals would create fewer opportunities for COVID-19 transmission.
In our study, HCWs in Wuhan had a lower CFR than non-HCWs. Recent studies indicated that cases aged over 65 years, with pre-existing comorbidities, might face a greater risk of a fatal outcome [17, 18]. However, in China, most in-service HCWs are under the age of 60. The use of PPE and hospital protocols would seem to be more related to the CIR than the CFR. Obviously, COVID-19 is serious and highly contagious. Further studies are needed to characterize this novel viral disease.
Our results indicate that most COVID-19 cases in HCWs in Wuhan were confirmed between 20 January 2020 and 5 February 2020. Person-to-person transmission was confirmed on 20 January 2020 and some infections in HCWs had been determined in Wuhan [19]. The lockdown in Wuhan, which started on 23 January 2020, has greatly prevented COVID-19 transmission [12]. It was reported that more than 40 000 HCWs from other provinces of the Chinese mainland arrived in Hubei Province to offer help. As of 31 March, none of them were identified to have been infected with SARS-CoV-2 [20]. This result indicates that a series of measures were effective in reducing infections in HCWs. With the rapid spread of the epidemic, 2 new hospitals (Huoshenshan and Leishenshan) were built in Wuhan and put into use in 10 days [21]. These facilities are specialized hospitals for infectious diseases, rather than simply units to receive and quarantine patients. Wuhan had also been building mobile Fangcang shelter hospitals (a Chinese name that came from Noah’s Ark) and creating tens of thousands of beds to centralize the quarantined patients and provide medical treatment for confirmed patients with mild symptoms. The combination of the construction of new infectious disease hospitals with mobile Fangcang shelter hospital construction could reduce infections in HCWs through controlling the source of infection to avoid cross-infection, relieving the huge pressure on the city’s medical system, providing different medical care for mild or critical patients to improve treatment efficiencies, effectively preventing nosocomial infections, and avoiding community infection due to home quarantine [22].
Our study has some notable limitations. First, we compared all HCWs with non-HCWs regardless of their age, comorbidities, and other characteristics that could have influenced the infection rate; therefore, our results should be interpreted carefully. Second, the detection bias with access to testing among healthcare providers compared with others also could have inevitably affected our assessment. Finally, we likely missed asymptomatic cases among HCWs and non-HCWs.
CONCLUSIONS
The COVID-19 outbreak is ongoing globally, and the safety of HCWs should be ensured to end the pandemic. The analysis of the infection status of HCWs is essential to attract enough attention from the public, provide effective suggestions for government agencies, and improve protective measures for HCWs. Ensuring an adequate supply of PPE is just the first step. Other measures should be considered, including a nutritious food supply, adequate rest time, and societal, familial, and psychological support.
Notes
Author contributions. W. W. and X. W. conceived, designed, and coordinated the study; L. Z., X. W., C. Z., Q. L., S. L., and Q. S. were responsible for data collection and accuracy confirmation; L. Z., C. Z., and Q. L. made substantial contributions to data analysis and interpretation; L. Z. was in charge of the manuscript draft, with help from all authors; X. W. made substantial revisions to the manuscript; M. W., S. L., Q. S., and Q. Z. participated in data analysis.
Financial support. This work was supported by the National Natural Scientific Foundation of China (grant numbers 81870767, 81570978), the Project of Jiangsu Provincial Medical Youth Talent (grant number QNRC2016118), the Key Project of Science and Technology Department of Jiangsu Province (grant number BL2014018), the Preventive Medicine Project of Jiangsu Province (grant number Y2015004), and the Nanjing Medical Science and Technique Development Foundation (grant numbers ZKX17033, YKK16162).
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol 2020; 92:401–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 3. World Health Organization. WHO Director-General’s remarks at the media briefing on COVID-19- 11 March 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 4. de Wit E, van Doremalen N, Falzarano D, et al. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol 2016; 14:523–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Song Z, Xu Y, Bao L, et al. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses 2019; 11:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization. Coronavirus disease (COVID-19) outbreak situation–87. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200416-sitrep-87-covid-19.pdf?sfvrsn=9523115a_2.
- 7. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323:1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CDC COVID-19 Response Team. Characteristics of health care personnel with COVID-19—United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020; 323:1335. [DOI] [PubMed] [Google Scholar]
- 10. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feng D, de Vlas SJ, Fang LQ, et al. The SARS epidemic in mainland China: bringing together all epidemiological data. Trop Med Int Health 2009; 14(Suppl 1):4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ji T, Chen HL, Xu J, et al. Lockdown contained the spread of 2019 novel coronavirus disease in Huangshi City, China: early epidemiological findings. Clin Infect Dis. Published online April 7, 2020. doi: 10.1093/cid/ciaa390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res 2020; 99:481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khan S, Jun L, Nawsherwan, et al. Association of COVID-19 with pregnancy outcomes in health-care workers and general women. Clin Microbiol Infect. Published online April 8, 2020. doi: 10.1016/j.cmi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Novel Coronavirus Pneumon ia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly 2020; 2:113–22. [PMC free article] [PubMed] [Google Scholar]
- 18. Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. Published online April 23, 2020. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chan JF-W, Yuan S, Kok K-H, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhan M, Qin Y, Xue X, et al. Death from Covid-19 of 23 health care workers in China. N Engl J Med. Published online April 15, 2020. doi: 10.1056/NEJMc2005696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. New 1,000-bed Wuhan Hospital Takes its First Coronavirus Patients, (2020). The Guardian. Available at: https://www.theguardian.com/world/2020/feb/04/new-1000-bed-wuhanhospital-takes-its-first-coronavirus-patients.
- 22. Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet 2020; 395:1305–14. [DOI] [PMC free article] [PubMed] [Google Scholar]