Abstract
Older people are particularly affected by the COVID19 outbreak because of their vulnerability as well as the complexity of health organisations, particularly in the often-compartmentalised interactions between community, hospital and nursing home actors. In this endemic situation, with massive flows of patients requiring holistic management including specific and intensive care, the appropriate assessment of each patient’s level of care and the organisation of specific networks is essential.
To that end, we propose here a territorial organisation of health care, favouring communication between all actors. This organisation of care is based on three key points:
To use the basis of territorial organisation of health by facilitating the link between hospital settings and geriatric sectors at the regional level.
To connect private, medico-social and hospital actors through a dedicated centralised unit for evaluation, geriatric coordination of care and decision support. A geriatrician coordinates this multidisciplinary unit. It includes an emergency room doctor, a supervisor from the medical regulation centre (Centre 15), an infectious disease physician, a medical hygienist and a palliative care specialist.
To organise an ad hoc follow-up channel, including the necessary resources for the different levels of care required, according to the resources of the territorial network, and the creation of a specific COVID geriatric palliative care service.
This organisation meets the urgent health needs of all stakeholders, facilitating its deployment and allows the sustainable implementation of a coordinated geriatric management dynamic between the stakeholders on the territory.
Keywords: COVID19, geriatrics, healthcare organisation, ethics, palliative care, decision-making, older people
Introduction
Older people are particularly affected by the COVID 19 outbreak [1]. There are several reasons for this. From a medical point of view, immunosenescence particularly exposes older adults to infectious risks and, in particular, to risks related to viruses [2]. The highly contagious nature of this virus on the one hand, and its relatively high virulence and respiratory tropism on the other hand, exposes older persons, especially those with several chronic conditions or impairments, to life-threatening risks [3]. Social reasons are also involved, such as the isolation of some older adults and the concentration of the virus within certain facilities [4–7].
As a result, the organisation, particularly in nursing homes, aggravates all the risks associated with COVID 19. At home, in the same way, formal and informal caregivers are themselves often contaminated and contaminating. Finally, the hospital is faced with an increased flow of patients with hemodynamic or respiratory insufficiency, including younger people requiring specific treatments and intensive care, and the frailest older peoples are at risk of being excluded from active care. This is reinforced by the atypical symptomatology of COVID in geriatric settings [8,9], with a high proportion of diarrhoea prior to signs of respiratory impairment appearing [10,11]. These signs, which are specific to geriatric patients, can delay diagnosis, especially when the reliability of the interview is compromised by delirium that may be added to pre-existing cognitive impairments. In these instances, there exists a major risk of:
Wrongfully considering a patient with non-specific signs as not being COVID-positive and, either hospitalising the patient in the conventional geriatric sector or returning him to an institution, favouring the transmission of SARS-CoV-2 to previously unaffected frail older people.
Considering, by default, an excessive limitation of care, particularly under the pressure of anticipating the need that beds be available for younger and/or less frail people. The massive inflow of patients and the compartmentalisation between the different stakeholders in the hospital and ambulatory care systems creates communication difficulties, which may lead to a potential failure to assess the appropriate level of personalised care needs [12].
Increasing psychological disorders or pathologies in relatives, doctors and nursing staff after the outbreak, with potentially complicated bereavements and burn-out syndromes, as soon as arbitrary medical decision-making appears.
Considering all of these points, and after analysis of decisions taken regarding limitations in access to intensive care services in other institutions or countries due to a lack of available or anticipated beds, we felt it necessary to propose changes in the organisation of care on our territory, in a centralised and coordinated approach, to allow generalised access to geriatric expertise.
The objective of this new healthcare organisation is to allow a multiprofessional discussion and to integrate geriatric competence into the organisation of care, both at the individual level (help in defining personalised level of care needs) and at the territorial organisation level to promote the appropriate use of different types of services and thus make the process more fluid by adapting it in real time.
This organisation of care is based on three key points:
To use the basis of a territorial organisation of health care by facilitating the link between hospital and geriatric sectors at the regional level.
To connect private services, nursing homes and hospital actors through a dedicated centralised unit for evaluation, geriatric coordination and decision support.
Organise an ad hoc follow-up channel, including the necessary resources for the different levels of care required, according to the resources of the territorial network, including the creation of a specific COVID geriatric palliative care service.
Methods: COVID geriatric healthcare organisation model
Who?
The model of care organisation is based on the creation, within our University Hospital, a regional geriatric reference centre, of a specialised, multidisciplinary geriatric evaluation unit in health organisation. This unit, led by three geriatricians, includes an emergency doctor, a supervisor from the Emergency Call Reception and Regulation Centre (CRRA15), an infectious disease physician, a medical hygienist and a palliative care specialist.
In order to meet the needs of the health organisations’ assessment and adaptation, as well as individual level of care-related requests, the three geriatricians who lead the unit have ethical training and a daily practice, which includes collaborative decision-making. The other professionals of the geriatric evaluation unit can be involved in the second step of the process, depending on the need.
What?
The geriatric assessment and coordination unit is based on a call centre through a unique phone number, created especially for the current situation. This line was opened on 18 March 2020 and is dedicated to:
Nursing homes and facilities for dependent or disabled older people,
General practitioners for their older patients living at home,
Local hospitals without adequate technical facilities (intensive care units, resuscitation).
In order to optimise telephone-based advice, a pre-call information-gathering guide was elaborated and communicated to all involved target stakeholders. This guide includes:
socio-demographic data,
the presence of known advanced-care planning,
designation of a trustworthy person,
clinical information including active co-morbidities, current therapies, and symptoms,
the presence of identified cases in the patient/caregiver’s environment,
biological or radiological data if available
the latest known data on the patient’s autonomy and functional independence.
As soon as this phone line was opened, a mobile palliative care team from our University Hospital provided direct call information about this new line to all targeted partners. The next day, an e-mail containing an information note specifying the objectives of this geriatric evaluation and coordination unit, as well as the information-gathering guide that had been drawn up, was sent to all the facilities and hospitals caring for vulnerable persons, as well as to the Medical Boards of the four departments of our area, in agreement with the concerned Regional Health Agency.
What for?
The objectives of this unit were defined following the needs assessment for our region.
Three levels were considered:
-
(i) Territorial organisation:
(a) Promote COVID+ screening of people at risk and/or contacts;
(b) Provide healthcare professionals necessary and useful information on hygiene measures to be put into place at home or in healthcare institutions and help them adapt isolation measures according to their particular situation.
-
(ii) Individual support to define appropriate levels of care:
(a) Allow discussions, on a case-by-case basis, to determine the required levels of care for people aged 75 and over;
(b) Allow diagnostic or therapeutic management assistance if necessary;
(c) Provide assistance in guiding these patients through the care pathway by providing real-time monitoring of the care pathways throughout the territory;
(d) Encourage the appropriate use of traditional geriatric networks for COVID negative patients needing geriatric care, after assessment of clinical needs and available resources for outpatient or inpatient management.
(iii) Coordination between stakeholders: To allow the transmission of information between the different actors such as the medical regulation centre (centre 15), general practitioners, nursing homes and hospitals, hygienists, palliative care physicians and geriatricians.
How?
In order to implement the various missions of the COVID geriatric unit, several mechanisms have been set up:
-
(i) In order to ensure the continuous sharing of medical information between the different actors, it appeared necessary to allow the transmission of complete information (geriatric evaluation included) to the emergency services and/or the supervision of the medical regulation call centre (Centre 15), which could receive a second call for a patient before or after the solicitation of the unit.
(a) To do this, a room dedicated to this geriatric evaluation unit has been provided, with installation on three workstations of the CENTAURE15® medical regulation call software.
-
(ii) To promote territorial support:
(a) Integration of regional COVID screening needs on the centralised COLOMBE software (CENTRE15—Coronavirus: NCOV Patient List for Infectious Diseases and Entrance Office), created prior to the case arriving at our unit for epidemiological identification needs, and linked to the CENTAURE15® software, to facilitate the centralisation of data. Once the patient is recorded in this database, the referring hygienist, in conjunction with dedicated interns, calls back the structures to organise the screening (ambulatory with travel or directly in the facility by a dedicated mobile unit).
(b) In addition to our unit, we have implemented various relay units in local hospitals in the whole area. Each unit operates on an identical model, with the designation of a referent pair, or even threesome when possible, which includes a geriatrician, a palliative care physician and a referent hygienist. These local teams have also created a hotline number that allows the University Hospital unit to reach them directly if necessary. It both optimises the transfer of information and provides a local relay for the monitoring of community situations.
(iii) For individual support in making decisions regarding appropriate levels of care, decision support criteria were defined on a collegial basis.
A flowchart was created as a decision support for emergency physicians (see Figure 1). It is based on the ‘Clinical Frailty Scale’ (CFS) [13,14], which is now systematically administered on admission of a person over 75 years of age to the emergency department, or on admission to the COVID+ clinical unit (AIR unit), or if necessary for individualised orientation assistance on phone calls to the geriatric unit by general practitioners or local hospitals.
Figure 1. Flow chart of the evaluation unit based on an assessment of frailty.
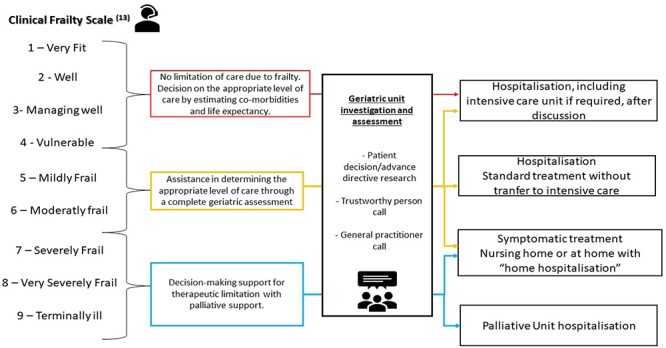
The decision-support thresholds are defined as follows:
CFS 1 to 4: No limitation of care due to frailty, except for specific elements for which a particular discussion takes place with the geriatric support-unit staff.
CFS 5 to 6: Decision-making support concerning the level of care in real time, 24 h a day, integrating the opinion of the resuscitation doctors if requested, depending on the clinical condition, by the geriatric evaluation unit and its health professionals.
CFS 7 to 9: Decision-making support for therapeutic limitation with palliative support either at the place of residence (in telephone contact with the mobile palliative care team), or a decision to be hospitalised in a dedicated COVID palliative care unit
Creation of dedicated follow-up pathway, with the opening of a dedicated COVID+ palliative care department
Once the level of care has been determined, the resulting orientation for follow-up is at one of four levels:
COVID negative or non-suspect patients, but requiring geriatric care, or at least geriatric advice, in particular because of difficulties in home care secondary to the reduction in healthcare services: preservation of a ‘traditional’ geriatric admission pathway, or maintenance of a ‘traditional’ home care system with the introduction/adaptation of home care if necessary, in connection with regional health authorities in order to have a vision of the health resources that can be mobilised.
Need for COVID+ care without any signs of immediate elevated risk level and without limitation of the level of care: integration of the COVID+ medical unit, within the university hospital or dedicated units in local hospitals, depending on the patient’s location and the availability of downstream resources (information in real time by daily feedback from referring pairs or by the regulation centre at centre 15 for ad hoc orientation, and connection, via the local correspondence unit, for adapted and early care).
Necessity of COVID+ management in intensive care from the outset, according to the clinical evaluation and the geriatric admission record on the unit, and without limitation of level of care with regard to frailty (CFS): transfer to an intensive care unit according to collegial discussion with the intensive care team.
Need for palliative care support for COVID+ or suspected COVID+ patients with therapeutic limitation from the outset in view of the overall assessment and frailty, or the ineffectiveness of the initial measures and/or oxygen therapy: to this end, a dedicated COVID palliative care unit was inaugurated on 20/03 in the palliative care department, more specifically dedicated to the management of complex situations. This unit currently has 17 beds. The team organises the care of patients to optimise symptomatic management of end of life, to break the isolation of the patient imposed by the outbreak, and to support families in this very particular situation.
On this unit, hygiene measures have been adapted to enable families to visit their loved ones, with specific conditions regarding visiting times and protective equipment. Indeed, as this sector is only dedicated to COVID+ patients, there is no isolation per room. Isolation procedures here have been put into place at a whole department level, allowing us to limit the use of personal protective equipment to a minimum. An airlock is organised at the entrance of this unit and adequate protective equipment is provided to families to respect all hygiene measures (precautions against droplets and contacts). In view of the specific arrangements for accompanying a COVID infected dead body, with immediate placement in a coffin, the CHU communication service has been asked to provide a camera to take a photograph of the deceased, if the family so wishes, as is done in obstetrics in the case of stillborn children, to allow the family to grieve.
Results
The implementation of this system was accomplished within four working days, with the support of the regional health authorities, the responsiveness of the hospital centre (administrative, emergency doctors and IT services) and a rapid communication sent to all actors. Indeed, during this intense period, the geriatric referral network, centralised at the CHU’s centre of expertise and available to local partners, facilitated a phased approach and an appropriate transfer of skills.
Initial user data, after 16 days of implementation, show the relevance of the care systems as the unit received 235 calls.
In the first 8 days, the platform received 141 calls of which 73% (N = 104) concerned requests to help determine the level of care. During the following 8 days, the platform received 94 calls of which 90% were related to level of care (N = 85). Other calls relayed concerns regarding hygiene and screening issues that were passed on to corresponding teams in the local hospital centres. In addition, COVID screening services was extended to include non-hospital laboratories in order to improve territorial coverage. This generated calls for questions from these professionals on the strategies to be adopted.
Of the 189 calls to help determine the level of care:
Ninety-nine patients were living in nursing homes.
Of these, 11 required transfer to hospital (11%). Nine were admitted to the emergency department and then hospitalised for standard care. For two residents, admission was necessary to administer symptomatic palliative care that could not be properly provided in their institutions. In this case, it was a direct admission to the palliative care unit of the university hospital;
Of the 88 residents who were not transferred to the hospital, 83 were provided with possible on-site symptomatic management (oxygen therapy, hydration and pain or delirium relief if necessary). Concerning these 88 residents, only eight had written advance-care planning. For all others, trustworthy persons or legal representatives were contacted, as well as their general practitioners, to assist in decision-making regarding the level of care to be provided in an effort to allow collegial patient care management.
Eighteen patients resided in seniors’ residences. Two of them were transferred to a hospital for standard care in COVID+ unit, two others received hospitalisation at home.
Seventy-two calls were about home situations. Of these, 38 were transferred to the hospital for direct care in a COVID+ unit, while 34 were given medical support at home, either by the general practitioner and liberal nurses or by a complete home hospitalisation service (4 cases).
The other 46 calls dealt with various issues: hygiene, drug supply, feedback on organisational problems in the region. The content of the questions evolved over time, as the system was progressively being put in place:
Earlier calls dealt with issues related to the proper use of barrier measures as well as the symptoms that should justify isolation and the modalities of diagnostic testing. Each question was the subject of a multidisciplinary consultation within the unit to enable the distribution of a ‘reference document’, validated by the health authorities as well as the professionals concerned and widely distributed throughout the territory thanks to the partners set up. This made it possible to avoid overloading the hotline and to maintain direct access to a geriatrician.
The issues then evolved, reflecting the effective dissemination of the initial information. The second week was particularly highlighted by questioning around clinical issues like anticoagulation pursuit or individual deconfinement measures after clinical improvement. Once again, a reference document was set up and disseminated throughout the territory.
After these 16 days using the system, the current occupancy rate of beds dedicated to COVID+ is 91%. The occupancy rate of COVID intensive care beds is 76% after the organisation of medical transport to other hospitals in France, Germany and Switzerland, to avoid saturation of the intensive care beds.
The proposed model facilitated a multidisciplinary assessment that respected the city/hospital link, including those involving emergency situations, which guaranteed an ethical approach to care and ad hoc support, regardless of the determined level of care requirements. After all the geriatric assessments were carried out, for the moment, no patient who was eligible for intensive care was disqualified because of age. Moreover, this model frees the traditional geriatric sector (COVID-) to maintain appropriate care for a particularly vulnerable population as it suffers the consequences of confinement, with an increased risk of decompensation (especially neurocognitive) due to changes in routine care [9].
Discussion
This model allowed inter-acculturation of all teams participating in the geriatric assessment and coordination unit: geriatricians, palliative care physicians, emergency physicians, infectious disease physicians and hygienists. No other studies have to our knowledge so far looked at more specific clinical and biological conditions in the older adult. Throughout the calls received, it has been proposed that barrier measures be implemented as soon as digestive signs appear, often a few days before respiratory signs. Tests carried out in the event of COVID suspected cases based on digestive signs were positive for those tested. Our feeling is that this has resulted in less spread in nursing homes than in some other areas affected. This would require further investigation to confirm or disprove this perception.
Finally, this proposed model is exportable, as it can be easily adapted to different healthcare systems, having already been shown to be effective on the territory where it was implemented. Moreover, it allows the sustainable implementation of a coordinated management of local actors, and thus encourages, over the long term, the development of fluid geriatric practices between the actors of sectors that all too often poorly collaborate.
Thus, at present, COVID has revealed how vulnerable the ageing population is, as well as the inadequacy of the healthcare system in caring for them. This emergency situation may help generate improved models of health organisations that were necessary for the current situation but that may also be sustainable for the future organisation of healthcare services. This model can be used as a framework.
A study is currently underway to evaluate the effectiveness of the implementation of this innovative system by trying to determine whether the responses provided by this call platform meet the objectives set. It is likely that further work, particularly concerning the satisfaction of professionals with the use of the line, would also be required. Finally, a vast qualitative study, conducted by the French national platform for end-of-life research, began a few days ago on the perceptions of older peoples, families, caregivers and professionals in all nursing homes in France.
Conclusion
Faced with these observations and the unprecedented scale of the COVID 19 outbreak and the human devastation it seems to generate, we wished to adapt the health organisation to this unthinkable reality with two key words: an organisation centred on the territories on the one hand, and on the possible care pathways of these older people at high risk of vital damage on the other hand, in compliance with an ethic of access to care and the most dignified conditions of care possible, in order to avoid any ageism in health care access. This has led us to set up a multidisciplinary geriatric evaluation and coordination unit to promote local assistance and the organisation of care, with the establishment of downstream pathways including the necessary resources for the different levels of care required, according to the resources of the territorial networks, including the creation of a specific COVID geriatric palliative care department.
Acknowledgments
The authors want to thank Carolina Bottari (Université de Montréal) for her review of the French to English translation. Also thanks to the Local Health Regional Agency (ARS Bourgogne Franche Comté) and the hospital administration for their support and responsiveness.
Declaration of Conflict of Interest
None.
Funding
None.
References
- 1. Coronavirus disease 2019 (COVID-19) Situation Report. Genève, Suisse: World Health Organization, 2020; Report No.: 51. [Google Scholar]
- 2. Tannou T, Koeberle S, Manckoundia P, Aubry R. Multifactorial immunodeficiency in frail elderly patients: contributing factors and management. Médecine Mal Infect 2019; 49: 167–72. [DOI] [PubMed] [Google Scholar]
- 3. Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun 2020; 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huhtinen E, Quinn E, Hess I, Najjar Z, Gupta L. Understanding barriers to effective management of influenza outbreaks by residential aged care facilities. Australas J Ageing 2019; 38: 60–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nicolay N, Boulet L, Le Bourhis-Zaimi M et al. . The role of dependency in a norovirus outbreak in a nursing home. Eur Geriatr Med 2018; 9: 837–44. [DOI] [PubMed] [Google Scholar]
- 6. Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc 2015; 16: 940–5. [DOI] [PubMed] [Google Scholar]
- 7. Harrison SL, Lang C, Whitehead C et al. . Trends in prevalence of dementia for people accessing Aged Care Services in Australia. J Gerontol A Biol Sci Med Sci 2020; 75: 318–25. [DOI] [PubMed] [Google Scholar]
- 8. Shahid Z, Kalayanamitra R, McClafferty B et al. . COVID-19 and older adults: what we know. J Am Geriatr Soc 2020. https://onlinelibrary.wiley.com/doi/abs/10.1111/jgs.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020. http://www.sciencedirect.com/science/article/pii/S246826672030061X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Luo S, Zhang X, Xu H. Don’t overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol 2020. http://www.sciencedirect.com/science/article/pii/S1542356520304018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tapé C, Byrd KM, Aung S, Lonks JR, Flanigan TP, Rybak NR. COVID-19 in a patient presenting with syncope and a normal chest X-ray. R I Med J 2020; 103: 50–1. [PMC free article] [PubMed] [Google Scholar]
- 12. Kunz R, Minder M. COVID-19 pandemic: palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Med Wkly 2020; 150:w20235 10.4414/smw.2020.20235. [DOI] [PubMed] [Google Scholar]
- 13. Rockwood K, Song X, MacKnight C et al. . A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wallis SJ, Wall J, Biram RWS, Romero-Ortuno R. Association of the clinical frailty scale with hospital outcomes. QJM Int J Med 2015; 108: 943–9. [DOI] [PubMed] [Google Scholar]


