The recent diffusion of a novel coronavirus (severe acute respiratory syndrome coronavirus 2, SARS-CoV-2) has been defined as a pandemic by the World Health Organization on March 11, 2020. This brutal infection is responsible for a syndrome named coronavirus disease 19 (COVID-19) that manifests with unspecific respiratory symptoms of variable severity, ranging from mild to life-threatening (1).
As the nation with the highest death toll and the new epicenter of a shifting pandemic, Italy is now trying to deal with one of the largest COVID-19 clusters outside of Asia. The Italian Ministry of Health has confirmed 63 927 infected patients, with 50 418 active cases, 20 692 recovered patients, 3204 intensive care unit admissions, and 6077 deaths, as of March 23. No one nation in the world can be adequately prepared to deal with such a difficult and dramatic challenge, and therefore sharing experiences between countries might help to build knowledge and face the situation in the best possible way (2). Most of the Italian COVID-19 figures are clustered in northern regions, the area where Parma University Hospital belongs. Herein, we aim to present our radiology experience in this fight against COVID-19 outbreak in Italy.
Radiology preparedness for COVID-19 pandemic
This rapidly evolving emergency must be handled quickly and needs dynamic decisions. Likewise, the overall hospital workflow, including imaging departments, should be specifically reorganized to both ensure the safety of their workforces and cover the expanding clinical needs, always keeping in mind that constrained resources may be a factor in such a decision-making process. Robust virus containment strategies should be implemented, considering that specific protected areas for the evaluation of patients with suspected or confirmed COVID-19 are essential to avoid secondary patient and staff exposures. Non-urgent procedures (e.g., systematic assessment of chronic diseases and screening procedures) should be postponed to minimize the risk of potential exposures and to reduce staff. Notably, staff reduction is focused on maintaining the minimum required, with as many employees as possible working from home. All department employees should also be aware of the recommended infection prevention techniques, such as frequent thorough handwashing and regular cleaning of fomites, as well as “social distancing strategies” (e.g., decreasing foot traffic in radiology reading rooms and canceling all departmental meetings). Personal protective equipment (PPE) must be made readily available in advance of the expected epidemic, and all employees must be trained on appropriate procedures for PPE use.
Safety for healthcare workers performing radiology exams
The main route of viral transmission is respiratory droplets, and rigorous protective measures are essential to limit the extent of transmissibility and guarantee healthcare workers’ safety while performing the imaging exams. As a mainstay in the prevention of the spread of COVID-19, patients must wear surgical mask during examinations and transport to and from the imaging department. In case of close contact with patients under investigation for COVID-19, the guidelines from the European Centre for Disease Prevention and Control (ECDC) recommend wearing a long-sleeved water-resistant gown, gloves, surgical mask, or if available a respirator, and eye protection (goggles or face shield) (3, 4). Hands disinfection with an alcohol-based solution is always required before using these protective tools.
Whenever possible, chest radiography must be performed with a portable device to avoid the movement of patients with suspected COVID-19. The “x-ray zones”, including radiographic and computed tomography (CT) rooms, should be adequately isolated, and subjects with suspected COVID-19 pneumonia should follow a well-delineated route to reach them. Only a radiographer should be in the radiographic or CT room to perform the exam, while radiologists should remain at the reading console in another decontaminated room. The detector of mobile x-ray, CT gantry, and every potentially contaminated surface must be disinfected after examination, using detergent solutions suggested by machine vendors, not to damage devices in use.
The role of imaging
The decision-making paths about clinical and diagnostic management of COVID-19 strongly depend on locally available resources, and a tailored approach is always needed to be able to take care of the massive number of hospital referrals during this pandemic. The real-time reverse transcription-polymerase chain reaction (RT-PCR) of viral nucleic acid is the reference standard for the diagnosis of COVID-19. However, this method still suffers from some limitations, notably the limited sensitivity (e.g., 60%–70%) (5, 6), the potential shortage, and delay with respect to the need for rapid decision-making for patients with clinically overt pneumonia. In such a setting, tools of thoracic imaging valuably assist the management of symptomatic patients selected from a first-line dedicated triage for respiratory symptoms.
There is still no consensus upon the integrated use of chest radiography or CT for the clinical assessment and management of subjects with suspected COVID-19 pneumonia. Chest radiography might have limited sensitivity for COVID-19 pneumonia because it is prone to miss subtle ground-glass opacification (the main pattern of the disease) even when they are quite diffuse in extent (7). Nevertheless, chest radiography is still helpful for the follow-up, evaluation of potential supervening complications (8), and the first-line evaluation of patients with a high pre-test probability of overt COVID-19 pneumonia.
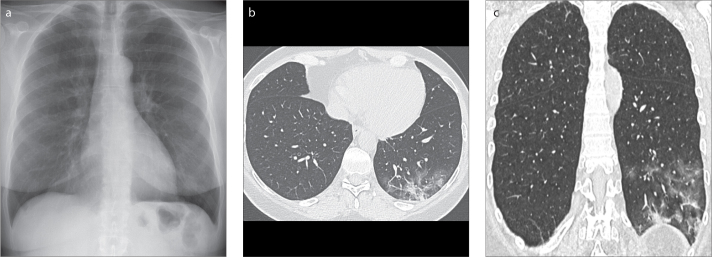
CT should not be used to screen COVID-19 (9). Its employment cannot prescind from the clinical evaluation. Despite unspecific findings of diffuse alveolar damage and the variable extent of organizing pneumonia generally seen in viral infections, the specific epidemic contingency makes CT a valid tool to attempt stratifying patients by imaging patterns and to assist during the clinical management of patients with unclear clinical scenarios or comorbidities. Notably, CT allows detecting subtle diffuse ground-glass opacities that are variably detected by radiography (Fig.), the continuous analysis of which might help in phenotyping the disease. The panoramic and detailed view of CT can also facilitate determining other potential causes of severe acute respiratory symptoms (e.g., lobar pneumonia, bronchiolitis, heart failure) (10).
Figure. a–c.
Chest radiography and high-resolution computed tomography (HRCT) in a 63-year-old man with COVID-19 pneumonia. He obtained a chest radiograph three days after the onset of the symptoms. (a) The frontal chest radiograph shows a very subtle opacity in the left lower lobe. (b) Axial and (c) coronal reformatted HRCT images clearly depict a ground-glass opacity admixed with consolidation in the subleural region of left lower lobe.
In case of immunocompromised patients or overlaps with preexisting lung disorders (e.g., extensive emphysema, lung fibrosis), COVID-19 pneumonia might lead to atypical patterns, reducing the diagnostic confidence on radiography as well as CT. In addition, radiologists and clinicians must be aware of the relationship between CT findings and the temporal evolution of the disease. In fact, up to approximately 50% of patients with COVID-19 may have normal CT scans 02 days after onset of flu-like symptoms (11), while subjects with normal CT may develop severe COVID-related pneumonia shortly (e.g., within two days) (12).
Conclusion
The COVID-19 outbreak represents a tough challenge for the medical system and inevitably radiology departments because imaging can play a valuable complementary role in the integrated diagnosis and clinical management of COVID-19 pneumonia. Radiology departments should carefully consider repurposing of their resources and guard the safety of their personnel first, while delivering clinical care.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gates B. Responding to Covid-19- A once-in-a-century pandemic? N Eng J Med. 2020 Feb 28; doi: 10.1056/NEJMp2003762. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.European Centre for Disease Prevention and Control (ECDC) Infection prevention and control for COVID-19 in healthcare settings. [Accessed March 31, 2020]. Third update - 31 March 2020. Available at: https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings.
- 4.European Centre for Disease Prevention and Control (ECDC) Guidance for wearing and removing personal protective equipment in healthcare settings for the care of patients with suspected or confirmed COVID-19. Feb, 2020. [Accessed March 31, 2020]. Available at: https://www.ecdc.europa.eu/en/publications-data/guidance-wearing-and-removing-personal-protective-equipment-healthcare-settings.
- 5.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 Feb 26; doi: 10.1148/radiol.2020200642. 200642. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020 Feb 19; doi: 10.1148/radiol.2020200432. 200432. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon SH, Lee KH, Kim JY, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:494–500. doi: 10.3348/kjr.2020.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill JR, Horner PE, Primack SL. ICU imaging. Clin Chest Med. 2008;29:59–76. doi: 10.1016/j.ccm.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 9.ACR Recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. [Accessed March 11, 2020]. Available at: https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection.
- 10.Dai W, Zhang H, Yu J, et al. CT Imaging and differential diagnosis of COVID-19. Can Assoc Radiol J. 2020 Mar 4; doi: 10.1177/0846537120913033. 846537120913033. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kanne JP. Essentials for radiologists on COVID-19: an update—Radiology Scientific Expert Panel. Radiology. 2020 Feb 27; doi: 10.1148/radiol.2020200527. 200527. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernheim A, Mei X, Huang M, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 Feb 20; doi: 10.1148/radiol.2020200463. 200463. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]