Abstract
Historically, adolescents and young adults (AYA) diagnosed with cancer have been an understudied population, and their unique care experiences, needs, and outcomes were not well understood. Thus, 10 years ago, the National Cancer Institute supported the fielding of the Adolescent and Young Adult Health Outcomes and Patient Experiences (AYA HOPE) study to address this gap. We recruited individuals diagnosed at ages 15 to 39 with germ cell, Hodgkin and non-Hodgkin lymphoma, acute lymphoblastic leukemia, and sarcoma from Surveillance, Epidemiology, and End Results cancer registries into the first multicenter population-based study of medical care, physical, and mental health outcomes for AYAs with cancer in the United States. This review of the 17 published manuscripts showed low awareness of clinical trials and substantial impact of cancer on financial burden, education and work, relationships and family planning, and physical and mental health. It highlights the feasibility of a longitudinal population-based study and key lessons learned for research on AYAs with cancer in and beyond the United States.
Keywords: adolescent, cancer care, health outcomes, quality of life, young adult
1 |. INTRODUCTION
In 2005, the United States National Cancer Institute (NCI), with support from the Lance Armstrong Foundation (LIVESTRONG), convened a Progress Review Group to bring together experts in the field of adolescent and young adult (AYA) oncology.1 This led to the first national cohort study of AYAs with cancer in the United States (US), the Adolescent and Young Adult Health Outcomes and Patient Experience (AYA HOPE) study.2,3 Though AYA cancer care is examined globally,4 this study was designed to examine care and outcomes in the US, given its unique healthcare system. AYA HOPE had three goals: (1) to determine the feasibility of conducting a US-based study using medical records and survey data from AYAs with cancer identified by Surveillance, Epidemiology, and End Results (SEER) US population-based cancer registries; (2) to determine the impact of cancer on medical care, psychosocial and physical functioning; and (3) to identify current experiences, gaps, and needs for cancer care in this population. In total, the study yielded 17 peer-reviewed publications that garnered more than 200 unique citations at of the time of this report preparation. This review provides an overview of the AYA HOPE study and synthesizes the findings to summarize information from the largest US population-based cohort study of AYAs with cancer and to guide future research in the US and internationally.
2 |. AYA HOPE STUDY DESIGN AND METHODS
Study participants diagnosed between ages 15 and 39 were identified from seven NCI SEER cancer registries: Detroit, Iowa, Louisiana, Los Angeles, Seattle-Puget Sound, Northern California, and Greater California. Study participants (n = 524) were diagnosed between July 1, 2007, and October 31, 2008, with one of the following cancers: germ cell, Hodgkin lymphoma, non-Hodgkin lymphoma, acute lymphoblastic leukemia (ALL), or sarcoma (Ewing, osteosarcoma, or rhabdomyosarcoma). These cancer sites were chosen based on their high prevalence among AYAs, and because they represented cancers in young adults that were less represented in NCI’s population health grant portfolio. Medical records were collected from all facilities that participants reported receiving care. Clinic type, physician subspecialties, diagnostic procedures, tumor characteristics and stage, participation in clinical trials, detailed treatment information, and any comorbid conditions were obtained from each facility.
The survey was brief (15–20 minutes), administered 6 to 14 months after diagnosis via internet or paper, with phone follow-up of nonresponders. Survey questions investigated psychological and social impacts of cancer, health-related quality of life (HRQOL), healthcare delivery practice patterns, barriers to care (e.g., financial and insurance), decisions about clinical trial involvement, demographic, socioeconomic, and supportive care characteristics. The overall goal for the survey was to identify areas of physical, social, and mental functioning, along with patient-perceived gaps in health services, that suggested the need for future study. Approximately 10 to 12 months after the original survey, a follow-up survey was conducted. It included questions from the original survey examining certain domains over time (e.g., job and school-related adjustment, HRQOL), plus additional questions (e.g., follow-up care and fertility preservation decisions). The follow-up assessment examined the feasibility of recontacting patients for longitudinal data collection in AYA cancer patients in the US.
Our initial examination of results focused on recruitment and characteristics of the study participants.5 Across all registries, 525 (43%) of eligible patients responded, 39% refused, and 17% were lost to follow-up (see Figure 1). Variations in response rate existed between the registries (range, 30%–60%), although the overall response rate was consistent with other research on adolescents during the same timeframe.6 Though 87% of participants required additional mailing or telephone contact, 91% of AYAs who completed the initial survey completed the follow-up survey. We mailed participants a paper survey along with information on the web address to complete the electronic version. Three quarters of respondents completed the paper version, likely due in part to email addresses being unavailable from SEER registries. Thus, the extra step to type in a web address may have been a barrier to electronic completion, and those who completed it online were more educated and had higher incomes than paper/phone responders. Males (P < 0.01), Hispanics, and non-Hispanic blacks (P < 0.001) were less likely to participate in the study, but age, education, cancer site, and time since diagnosis were not associated with participation. These findings suggested that while longitudinal research on AYAs is feasible, additional efforts (such as targeted outreach, focus groups convened to explore identified barriers and potential solutions, and working within community settings) to target Hispanic, black, and male AYAs in future studies are needed.
FIGURE 1.
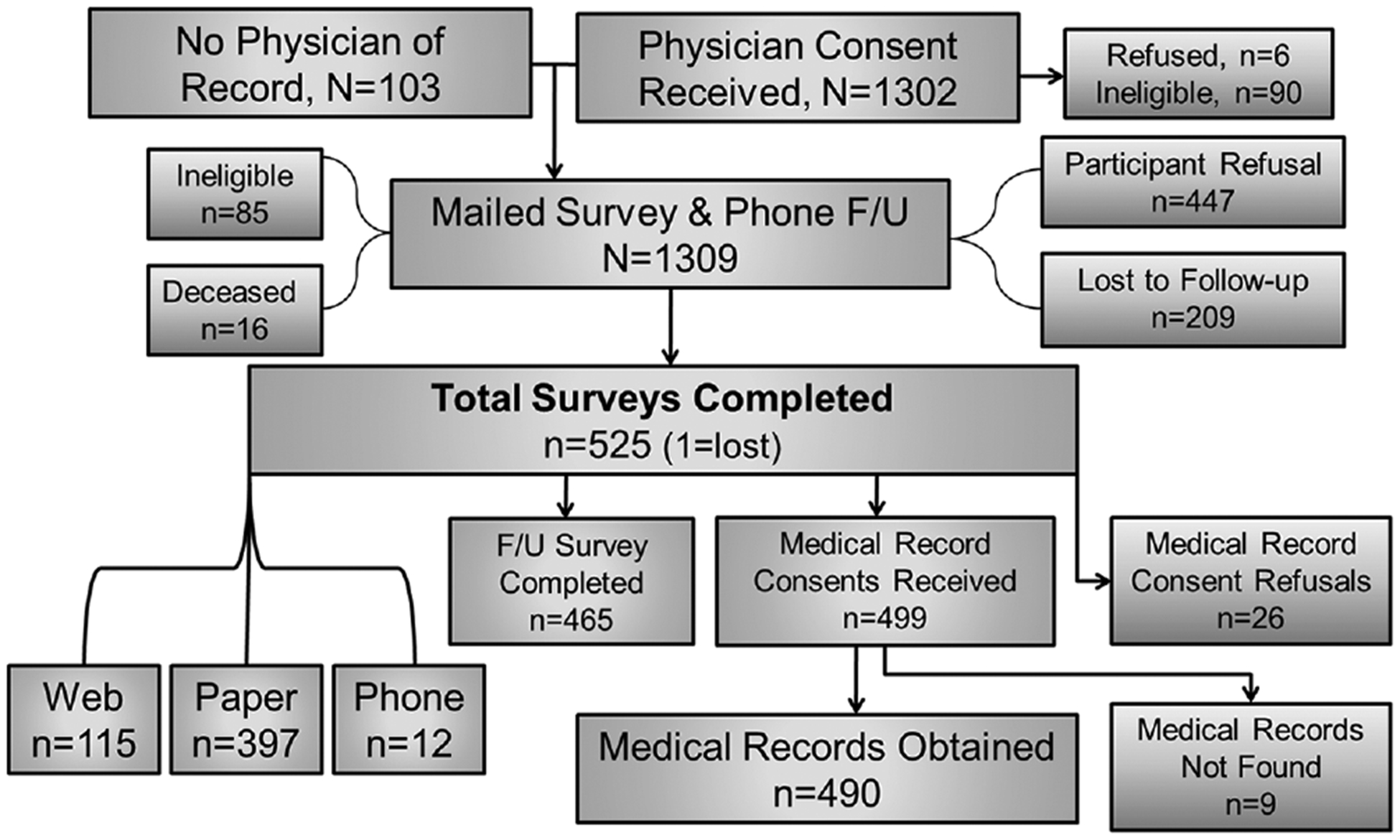
Recruitment flow diagram of AYA HOPE. Reprinted with permission from Journal of Cancer Survivorship.5
3 |. TREATMENT AND CLINICAL TRIAL ENROLLMENT
Given concerns that AYAs may be at risk for poorer care particularly because in the US, there is no specific medical “home” for this age group,1,7 a priority of AYA HOPE was to determine whether AYAs were getting appropriate treatment and enrolling in clinical trials. Survey and medical record data indicated that 95% of the cohort had received medical care in the year prior to the first survey, and 17% were receiving cancer treatment at that time.8 In an evaluation of initial treatment based on criteria developed by clinical specialists in AYA oncology, 75% of the cohort was determined to have received appropriate treatment. After excluding stage I male germ cell patients who all received appropriate treatment, the rate was reduced to 68%. Other research indicates that AYAs receive less aggressive therapies than children9 and more aggressive therapies than older adults.10 Although AYA HOPE used clinical advisors to determine appropriate treatment, one limitation the study faced was the lack of guidelines or national consensus about a definition of appropriate therapy for this population. AYA HOPE medical records indicated that 13% of study participants were treated on a clinical trial. Cancer type (P < 0.01) and clinical trial participation (P < 0.05) were associated with receiving appropriate treatment. Appropriate treatment was highest among sarcoma patients (79%) and lowest among ALL patients (56%).
Survey responses indicated that only 17% of AYAs were aware that there were clinical trials available for their stage or type of cancer.11 Among those who knew a trial was available, 68% were enrolled. For respondents who chose not to participate in a trial, the primary reason was concern about involvement in research, including experimental treatments and side effects. Additionally, 21% indicated problems accessing trials. Alongside the AYA HOPE study, the NCI conducted another study of treatment patterns in a larger cohort of AYAs (n = 1358) identified via SEER registries during the same timeframe as AYA HOPE.12 That study reviewed medical records and queried physicians. Results showed that only 14% of AYAs had enrolled on a clinical trial and were more likely to have insurance, be younger, and be treated by pediatric oncologists. Together, these data suggested that lower availability and concerns with involvement in clinical trials might be important factors in AYAs not receiving appropriate care.
4 |. FINANCIAL IMPACT, INSURANCE, AND CARE
The financial impact of cancer is substantial at any time in life.13 However, young adults are particularly vulnerable because they are early in their professional development and face increasing financial independence. Additionally, with transitions from school to full-time work, sources of health insurance change. Approximately two thirds of respondents 21 to 39 years (and >50% of those 15–20 years) reported a negative impact of cancer on their financial situation.14 Financial advice was the most common supportive service reported as unmet by AYAs,15 and more than half of all respondents indicated an unmet need for financial advice or information.16 At the time of the AYA HOPE study, which predated the Affordable Care Act,17 young adults were a group with one of the highest uninsured rates.18 Given the potential financial vulnerability of AYAs with cancer, AYA HOPE also examined financial and insurance factors associated with medical care utilization.
At the follow-up survey, most AYA HOPE study participants (88%) had received cancer-related medical care in the past 12 months and 17% were undergoing cancer treatment. Not surprisingly, receipt of cancer-related care was associated with having current or prior-year health insurance.8 Survey responses showed that most AYAs were insured during initial treatment but the percentage of insured patients decreased over time, with more than a quarter of the cohort experiencing some period without insurance.19 Additionally, 11% of the whole cohort and 25% of those who did not receive medical care in the prior year had lost health insurance.8 Having coverage did not always correspond to the receipt of care. More than 20% of AYA HOPE respondents indicated there were tests/treatments not covered by insurance; however, most of those patients (81%) received this care regardless of insurance (Figure 219). Consistent with AYA research highlighting socioeconomic impacts on HRQOL,20 AYA HOPE respondents without health insurance reported worse HRQOL, including worse overall physical and mental health, emotional functioning, and fatigue.21 In an open-ended question where participants could describe anything about their medical care or experience with cancer, they highlighted financial problems, including challenges with insurance coverage.22 Overall, these data suggest that AYAs with cancer in the US experience adverse impacts of their care and outcomes when health insurance is lacking.
FIGURE 2.
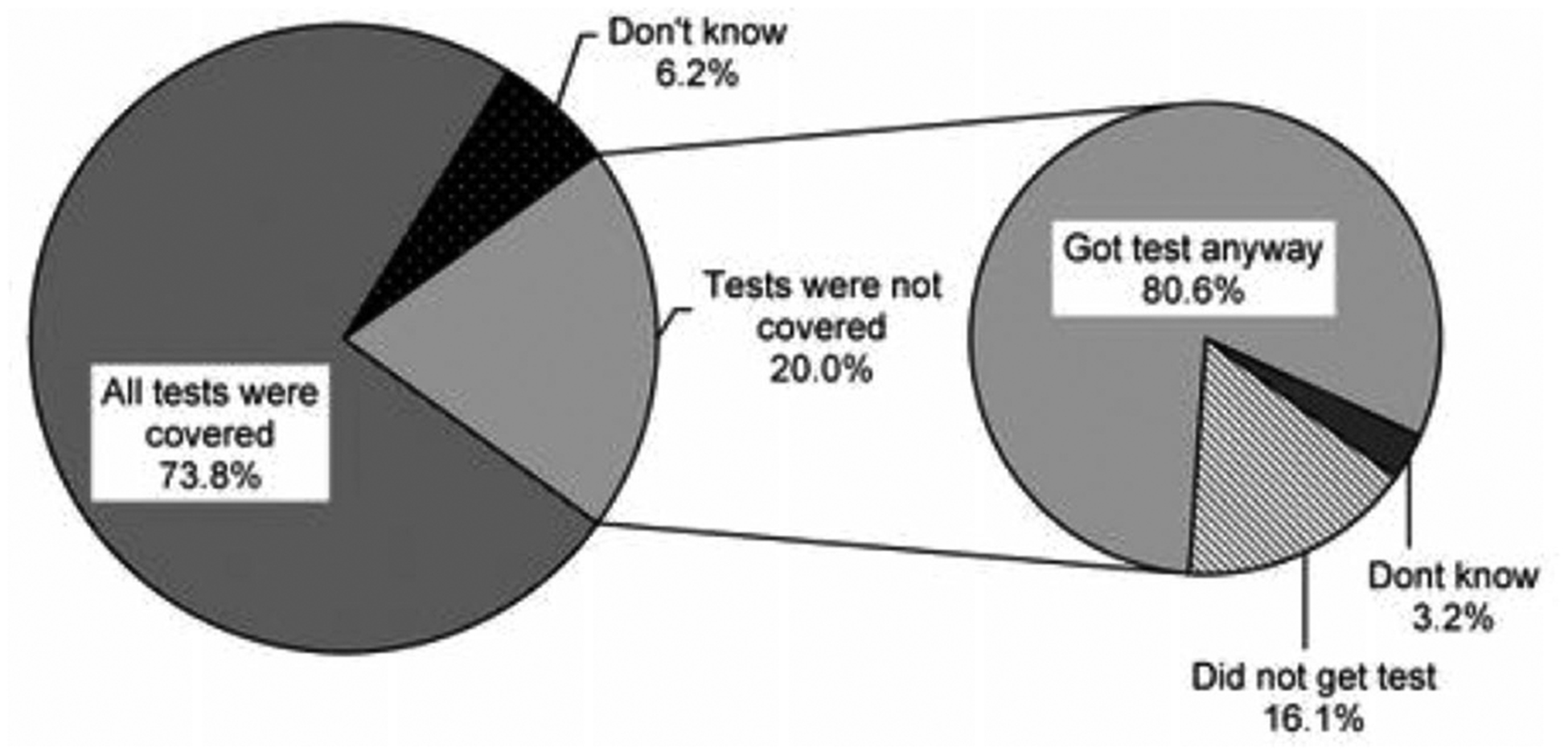
Coverage of doctor-recommended cancer tests/treatment (n = 465). The percentage of participants who indicated that there were doctor-recommended tests or treatments not covered by their insurance in the baseline survey as well as whether they received the test/treatments regardless of insurance coverage. Reprinted with permission from Cancer19
5 |. CARE EXPERIENCES AND UNMET NEEDS
From the survey, we learned that more than half of the AYA HOPE cohort reported excellent overall quality of care.16 Qualitative responses indicated that participants attributed satisfaction with care to various healthcare services. These included the availability and communication of healthcare information to support decision-making, coordination of care, appropriate management of side effects, and the speed and flexibility of treatments.22 Those who reported being dissatisfied with care described concerns about lacking information regarding medical protocols and side effects, alternative treatment options, and follow-up care. Several respondents also felt dissatisfied based on a belief that their initial cancer diagnosis was delayed. Unfortunately, survey methodology is inadequate for determining whether actual delays occurred, as our preliminary testing of survey items suggested the potential for recall bias. However, given that patients do perceive delays, this topic should be investigated in future studies with pre–post-diagnosis medical data.
One challenge in understanding cancer care received by AYAs is determining their treatment facilities and providers. AYAs can be treated at pediatric or adult-focused cancer centers, depending on their age and type of cancer. We found that the majority of AYA patients in the cohort were treated in cancer centers (66%), with one third of those treated in NCI-designated centers.23 Additionally, 8% of the institutions were academic and only 2% of the cohort was identified as treated in a pediatric hospital, with the remaining patients treated at community hospitals.21 Physicians treating AYA HOPE patients were predominately trained in nonpediatric specialties, with fewer than 5% treated by pediatric specialists.23 With so few patients being treated in pediatric facilities or by pediatricians, comparisons could not be made between the type of care received by pediatric specialization. However, these data were consistent with the age of the respondent and the type of cancer being treated. In the AYA HOPE study, 13% of the cohort were adolescents (under age 20) with an additional 18% were 20 to 25 years. The cancer type most likely treated by pediatric specialists was ALL, but only 4% of the cohort was being treated for that cancer.
Concerning supportive care services, we found that more than half of respondents had unmet information needs relating to their cancer returning and cancer treatments, long-term side effects of treatment, obtaining financial support for medical care and having children in the future.16 Adults 30 years or older, males, those of non-white race/ethnicity, and those who reported less than excellent general health or fair/poor quality of care were more likely to report unmet information needs. However, social information needs were higher among younger adults (those diagnosed in their 20s), as well as those with greater symptom burden and those not in social support groups.24 Greater unmet information need was also associated with lower overall mental and physical HRQOL.25 Additionally, 56% to 75% of AYA HOPE respondents who needed a support group, a pain management expert, physical or occupational therapist, mental health worker, or financial advice on paying for health care did not receive these services. Recent European research has also shown a dearth of available AYA-focused supportive care.4 In AYA HOPE, factors associated with unmet services included having two or more comorbidities26 and reporting any physical symptoms.16 Unmet service needs were also associated with worse mental, physical, and overall HRQOL.15 Needing mental health services had the strongest associations with worse HRQOL outcomes, and needing physical/occupational therapy was most consistently associated with poorer functioning across health outcomes. These data suggest that there may be vulnerable subgroups of AYAs who should be targeted to ensure that their information and service needs are met, particularly as those needs were associated with worse outcomes.
6 |. IMPACT OF CANCER ON SOCIAL, PSYCHOLOGICAL, AND FUNCTIONAL OUTCOMES
When cancer occurs in late adolescence or early adulthood, one of the major concerns is how it might affect educational attainment and professional goals. In the AYA HOPE cohort, approximately 30% of teens and 40% of young adults reported negative impacts of cancer on plans for employment,14 and both intensive treatment and quitting school or work were associated with negative plans for education or employment.27 In open-ended responses, AYAs described job or education loss,22 similar to prior European research.28 In AYA HOPE, more than half of full-time workers/students reported problems with work/studies after diagnosis even though most AYAs (72%) in full-time work or school reported returning to these activities.27 Those least likely to return to work were those who lacked health insurance or those who quit working right after being diagnosed with cancer. In open-ended responses, AYAs described an inability to integrate cancer care and day-to-day life activities, including work and school.22 Overall, these data suggested substantial impacts of cancer on work and school for AYAs.
To identify needs for future studies and inform interventions related to the psychosocial impacts of cancer on AYAs, the survey queried participants about positive, negative, and neutral impacts of cancer on friend and family relationships, dating, marriage and family planning, sexual intimacy, and body image. AYAs reported both negative and positive impacts of cancer on their relationships with friends and family, and more reported positive impacts.14 A review of the social impacts of cancer on AYAs29 described negative effects, though in general studies were not designed to examine positive relationship impacts. In AYA HOPE, more respondents reported negative impacts on dating, sexual intimacy, body image, and control over life, as has been shown in qualitative research.30 Negative impacts of cancer on sexual intimacy were persistent; 49% reported negative effects on sexual function 1-year post-cancer diagnosis and 70% of those persisted in their negative perceptions 2 years after diagnosis.31 More than half of AYAs reported negative impacts of cancer on their plans for having children.14 These concerns are well-founded, as national and international studies have shown that AYAs with cancer are more likely to have adverse reproductive outcomes.32–35 In AYA HOPE, when we explored more details about the extent to which providers discussed fertility preservation with AYAs in the cohort, we found substantial gender differences, with males more likely to have had fertility preservation options discussed and recommended by providers.36 Furthermore, those without insurance or those already raising children were less likely to discuss fertility preservation with providers. Together, these data suggest that while some relationships may improve, the negative effects of cancer on dating, sexuality, fertility, and family planning can be substantial.
Consistent with more recent clinic-based research of AYAs with any invasive cancer,37 as well as a recent international review,38 we found that AYAs with cancer reported significantly worse physical and mental health than did similarly aged general and healthy populations in HRQOL, with largest differences reported regarding limitations to physical and emotional roles, physical and social functioning, and fatigue.21 Physical and mental health were worse for AYAs in current treatment, with current/recent symptoms, or lacking health insurance at any time since diagnosis. Worse physical health was reported by sarcoma patients, Hispanic patients, and those with lower education. Unmarried patients reported worse mental health. Other areas that influenced HRQOL outcomes included comorbidities (for which an index tailored to this age group was developed26), unmet service needs,15 and negative perceptions of control over their lives.25 Overall, our findings suggest that subgroups of AYA patients with cancer experience major decrements in several physical and mental HRQOL domains.
7 |. DISCUSSION
The AYA HOPE study demonstrated that a US population-based AYA cohort could be successfully recruited and followed short term, and it provided insights into the experiences of AYA cancer patients. This study was the first population-based cancer registry study to examine care quality, physical and mental health outcomes for AYAs; it highlighted major impacts of cancer and the many remaining research gaps in this population. Since its rollout, several other studies have been published reporting results generally consistent with or extending AYA HOPE findings; they show the persistent impact of cancer on symptom burden, HRQOL, sexuality and relationships, end-of life issues, and barriers to clinical trial enrollment (e.g.,39–45). To summarize the state of the science of AYA oncology, in 2013, a workshop was conducted including review of current research by over 60 experts in the field.46 Manuscripts summarized current trends in cancer incidence, mortality and survival,47,48 basic biological characteristics for AYA cancers,49 clinical trial enrollment, care quality and health services,46 and social functioning.29 Together, the evidence reviewed suggests that in recent years more attention has been paid to the needs of AYAs with cancer, and investigators have launched larger cross-sectional41 and prospective, longitudinal studies.44,50
Prior to AYA HOPE, though AYAs with cancer were recognized as an understudied population,1 national data examining cancer’s impact in the US were unavailable, and it was difficult to know the extent of the challenges faced by AYAs. The AYA HOPE study provided the clinical and research communities with medical and survey data about care and outcomes experienced and provided the following lessons. First, we demonstrated the feasibility of recruiting and following patients from population-based registries who were diagnosed with cancer between ages 15 and 39. Though feasible, response rates were low, and extensive effort in using multiple modes of data collection (e.g., paper, online, and telephone) was needed. Another success was our ability to obtain a high follow-up response rate and identify how our patient population differed from the underlying eligible population and compare responders and nonresponders. AYA HOPE highlighted challenges with recruiting males, blacks, and Hispanics. Recruiting from registries allowed targeting of more vulnerable subgroups not often represented in research, such as those who are uninsured or treated outside specialty centers. These findings suggest a need for targeted research in future epidemiologic and health services studies to ensure we are addressing the impact and needs among the full AYA population. Limitations to the AYA HOPE study included our US-only study, lack of age- or cancer-based comparison groups, broad (rather than in-depth) survey questions, and inclusion of a small number of cancer types, restricting the generalizability of the findings.
Future studies are still needed to compare the experience of AYAs to older and younger cancer populations and evaluate outcomes later in the survivorship period (e.g., five or more years after cancer diagnosis), as has been done for childhood cancer survivors.51 Furthermore, there is a need to examine other cancers affecting AYAs. AYA HOPE focused on five prevalent cancers, but many common cancers in AYAs were not represented in the study (e.g., breast, colon, gynecological cancers). Many research questions remain unanswered. Specifically, concern about delay in diagnosis has been reported elsewhere and explored among AYAs.52–54 Further research is also needed on care quality and clinical trial enrollment among those treated by physicians or in institutions with pediatric specialization or by type of practice (e.g., research conducted in NCI-designated cancer centers vs community settings55).
Finally, there were topic areas suggesting a need for ongoing monitoring. Extensive financial burden was evident from the results of AYA HOPE. Recent efforts have shown financial burden on AYAs with cancer56,57 and compared with adults diagnosed with cancer at older ages,58 suggesting that financial burden may be similar to that of older cancer patients, but that the source of burden (work days lost) was different for AYAs. Parental insurance coverage mandates for young adults up to age 26 did not occur until after study completion.59 Thus, assessment of the financial impact of cancer in a changing environment of health insurance coverage is needed. Other topics requiring future exploration include obtaining necessary survivorship care; identification and alleviation of barriers to care; evaluation and monitoring of symptoms, changes in comorbidities and HRQOL; identification of family planning and fertility issues; and research on cancer impact among vulnerable subgroups of AYAs, such as racial/ethnic minorities and those with low financial resources. Future studies could also investigate areas relevant to longer term survivors that were not previously examined in AYA HOPE (e.g., recurrence of the initial cancer, late effects, and health behaviors) as AYAs survive years beyond their initial diagnoses.
In summary, the AYA HOPE study provided evidence to the AYA oncology research community that population-based research on medical care and outcomes in AYAs with cancer in the US is feasible and sets the stage for additional research to understand and address the needs of this young, vulnerable, resilient population. As one AYA HOPE study participant explained, “Having cancer was a surreal experience. I learned that I am stronger than I thought. I am not a cancer survivor, but a cancer defeater.”
ACKNOWLEDGMENTS
The authors wish to acknowledge the AYA HOPE study team who contributed meaningfully to the design, implementation, and interpretation of the study. We also acknowledge the many AYA patients, survivors, and caregivers who participated in the survey development and in the final study. We also thank Dr. Erin Kent for her thoughtful editorial suggestions and logistic support of the manuscript.
Funding information
National Cancer Institute, Grant/Award Numbers: N01PC-2010-00029, N01PC-2010-00028, N01PC-2010-00030, N01PC-2010-00032, N01PC-2010-00034, N01PC-2010-00035, N01PC-2010-00140
Abbreviations:
- ALL
acute lymphoblastic leukemia
- AYA
adolescent and young adult
- AYA HOPE
Adolescent and Young Adult Health Outcomes and Patient Experiences Study
- HRQOL
health-related quality of life
- NCI
National Cancer Institute
- SEER
Surveillance Epidemiology and End Results
- US
United States (of America)
Footnotes
CONFLICTS OF INTEREST
The authors have no conflict of interest to report. The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the National Cancer Institute, the National Institutes of Health, or the US Department of Health and Human Services.
REFERENCES
- 1.Adolescent and Young Adult Oncology Progress Review Group. Closing the gap: research and care imperatives for adolescents and young adults with cancer (NIH Publication No. 06–6067). Bethesda, MD: 2006. August Report nr NIH Publication No. 06–6067. 108 p. [Google Scholar]
- 2.National Cancer Institute. 2015 January 24, 2018. Adolescents and young adults with cancer. <https://www.cancer.gov/types/aya>. Accessed 2018 January 24, 2018.
- 3.National Cancer Institute. 2018 January 24. Healthcare delivery research program. https://healthcaredelivery.cancer.gov/. Accessed 2018 January 24.
- 4.Saloustros E, Stark DP, Michailidou K, et al. The care of adolescents and young adults with cancer: results of the ESMO/SIOPE survey. ESMO Open. 2017; 2: e000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harlan LC, Lynch CF, Keegan TH, et al. Recruitment and follow-up of adolescent and young adult cancer survivors: the AYA HOPE study. J Cancer Surviv. 2011;5:305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richards J, Wiese C, Katon W, et al. Surveying adolescents enrolled in a regional health care delivery organization: mail and phone follow-up—what works at what cost. J Am Board Fam Med. 2010;23:534–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stock W, La M, Sanford B, et al. What determines the outcomes for adolescents and young adults with acute lymphoblastic leukemia treated on cooperative group protocols? A comparison of children’s cancer group and cancer and leukemia group B studies. Blood. 2008;112:1646–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keegan TH, Tao L, DeRouen MC, et al. Medical care in adolescents and young adult cancer survivors: what are the biggest access-related barriers. J Cancer Surviv. 2014;8:282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta AA, Pappo A, Saunders N, et al. Clinical outcome of children and adults with localized Ewing sarcoma: impact of chemotherapy dose and timing of local therapy. Cancer. 2010;116:3189–3194. [DOI] [PubMed] [Google Scholar]
- 10.Alvarado R, Lari SA, Roses RE, et al. Biology, treatment, and outcome in very young and older women with DCIS. Ann Surg Oncol. 2012;19:3777–3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shnorhavorian M, Doody DR, Chen VW, et al. Knowledge of clinical trial availability and reasons for nonparticipation among adolescent and young adult cancer patients: a population-based study. Am J Clin Oncol. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parsons HM, Harlan LC, Seibel NL, et al. Clinical trial participation and time to treatment among adolescents and young adults with cancer: does age at diagnosis or insurance make a difference. J Clin Oncol. 2011;29:4045–4053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Altice CK, Banegas MP, Tucker-Seeley RD, et al. Financial hardships experienced by cancer survivors: a systematic review. J Natl Cancer Inst. 2017;109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bellizzi KM, Smith A, Schmidt S, et al. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer. 2012;118:5155–5162. [DOI] [PubMed] [Google Scholar]
- 15.Smith AW, Parsons HM, Kent EE, et al. Unmet support service needs and health-related quality of life among adolescents and young adults with cancer: the AYA HOPE study. Front Oncol. 2013;3:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: a population-based cancer registry study. J Cancer Surviv. 2012;6:239–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patient Protection and Affordable Care Act. 42 USC § 180012010.
- 18.National Center for Health Statistics. Health, United States, 2008 With Chartbook. Hyattsville, MD: NCHS; 2009. [Google Scholar]
- 19.Parsons HM, Schmidt S, Harlan LC, et al. Young and uninsured: insurance patterns of recently diagnosed adolescent and young adult cancer survivors in the AYA HOPE study. Cancer. 2014;120:2352–2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kent EE, Sender LS, Morris RA, et al. Multilevel socioeconomic effects on quality of life in adolescent and young adult survivors of leukemia and lymphoma. Qual Life Res. 2013;22:1339–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith AW, Bellizzi KM, Keegan TH, et al. Health-related quality of life of adolescent and young adult patients with cancer in the United States: the adolescent and young adult health outcomes and patient experience study. J Clin Oncol. 2013;31:2136–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zebrack B, Kent EE, Keegan TH, et al. “Cancer sucks,” and other ponderings by adolescent and young adult cancer survivors. J Psychosoc Oncol. 2014;32:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsons HM, Harlan LC, Schmidt S, et al. Who treats adolescents and young adults with cancer? A report from the AYA HOPE study. J Adolesc Young Adult Oncol. 2015;4:141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kent EE, Smith AW, Keegan TH, et al. Talking about cancer and meeting peer survivors: Social information needs of adolescents and young adults diagnosed with Cancer. J Adolesc Young Adult Oncol. 2013;2:44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeRouen MC, Smith AW, Tao L, et al. Cancer-related information needs and cancer’s impact on control over life influence health-related quality of life among adolescents and young adults with cancer. Psychooncology. 2015;24:1104–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu XC, Prasad PK, Landry I, et al. Impact of the AYA HOPE comorbidity index on assessing health care service needs and health status among adolescents and young adults with cancer. Cancer Epidemiol Biomarkers Prev. 2015;24:1844–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30:2393–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grinyer A The biographical impact of teenage and adolescent cancer. Chronic Illn. 2007;3:265–277. [DOI] [PubMed] [Google Scholar]
- 29.Warner EL, Kent EE, Trevino KM, et al. Social well-being among adolescents and young adults with cancer: a systematic review. Cancer. 2016;122:1029–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carpentier MY, Fortenberry JD, Ott MA, et al. Perceptions of masculinity and self-image in adolescent and young adult testicular cancer survivors: implications for romantic and sexual relationships. Psychooncology. 2011;20:738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wettergren L, Kent EE, Mitchell SA, et al. Cancer negatively impacts on sexual function in adolescents and young adults: the AYA HOPE study. Psychooncology. 2017;26:1632–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anderson C, Engel SM, Mersereau JE, et al. Birth outcomes among adolescent and young adult cancer survivors. JAMA Oncol. 2017;3:1078–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haggar FA, Pereira G, Preen D, et al. Adverse obstetric and perinatal outcomes following treatment of adolescent and young adult cancer: a population-based cohort study. PLoS One. 2014;9:e113292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madanat-Harjuoja LM, Malila N, Lahteenmaki PM, et al. Preterm delivery among female survivors of childhood, adolescent and young adulthood cancer. Int J Cancer. 2010;127:1669–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magelssen H, Melve KK, Skjaerven R, et al. Parenthood probability and pregnancy outcome in patients with a cancer diagnosis during adolescence and young adulthood. Hum Reprod. 2008;23:178–186. [DOI] [PubMed] [Google Scholar]
- 36.Shnorhavorian M, Harlan LC, Smith AW, et al. Fertility preservation knowledge, counseling, and actions among adolescent and young adult patients with cancer: a population-based study. Cancer. 2015;121:3499–3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Husson O, Zebrack BJ, Block R, et al. Health-related quality of life in adolescent and young adult patients with cancer: a longitudinal study. J Clin Oncol. 2017;35:652–659. [DOI] [PubMed] [Google Scholar]
- 38.Sodergren SC, Husson O, Robinson J, et al. Systematic review of the health-related quality of life issues facing adolescents and young adults with cancer. Qual Life Res. 2017;26:1659–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Acquati C, Zebrack BJ, Faul AC, et al. Sexual functioning among young adult cancer patients: a 2-year longitudinal study. Cancer. 2018;124:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Champion VL, Wagner LI, Monahan PO, et al. Comparison of younger and older breast cancer survivors and age-matched controls on specific and overall quality of life domains. Cancer. 2014;120:2237–2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mack JW, Chen LH, Cannavale K, et al. End-of-Life care intensity among adolescent and young adult patients with cancer in Kaiser Permanente Southern California. JAMA Oncol. 2015;1:592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salsman JM, Garcia SF, Yanez B, et al. Physical, emotional, and social health differences between posttreatment young adults with cancer and matched healthy controls. Cancer. 2014;120:2247–2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sanford SD, Zhao F, Salsman JM, et al. Symptom burden among young adults with breast or colorectal cancer. Cancer. 2014;120:2255–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Husson O, Zebrack B, Block R, et al. Posttraumatic growth and well-being among adolescents and young adults (AYAs) with cancer: a longitudinal study. Support Care Cancer. 2017;25:2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jacob SA, Shaw PH. No improvement in clinical trial enrollment for adolescents and young adults with cancer at a children’s hospital. Pediatric Blood Cancer. 2017;64. [DOI] [PubMed] [Google Scholar]
- 46.Smith AW, Seibel NL, Lewis DR, et al. Next steps for adolescent and young adult oncology workshop: an update on progress and recommendations for the future. Cancer. 2016;122:988–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barr RD, Ries LA, Lewis DR, et al. Incidence and incidence trends of the most frequent cancers in adolescent and young adult Americans, including “nonmalignant/noninvasive” tumors. Cancer. 2016;122:1000–1008. [DOI] [PubMed] [Google Scholar]
- 48.Keegan TH, Ries LA, Barr RD, et al. Comparison of cancer survival trends in the United States of adolescents and young adults with those in children and older adults. Cancer. 2016;122:1009–1016. [DOI] [PubMed] [Google Scholar]
- 49.Tricoli JV, Blair DG, Anders CK, et al. Biologic and clinical characteristics of adolescent and young adult cancers: acute lymphoblastic leukemia, colorectal cancer, breast cancer, melanoma, and sarcoma. Cancer. 2016;122:1017–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kwak M, Zebrack BJ, Meeske KA, et al. Trajectories of psychological distress in adolescent and young adult patients with cancer: a 1-year longitudinal study. J Clin Oncol. 2013;31:2160–2166. [DOI] [PubMed] [Google Scholar]
- 51.Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA. 2003;290:1583–1592. [DOI] [PubMed] [Google Scholar]
- 52.Martin S, Ulrich C, Munsell M, et al. Delays in cancer diagnosis in under-insured young adults and older adolescents. Oncologist. 2007;12:816–824. [DOI] [PubMed] [Google Scholar]
- 53.Mou J, Bolieu EL, Amoroso PJ, et al. Treatment delay in adolescent and young adult cancer patients: what matters. Ann Epidemiol; 272017:1. [Google Scholar]
- 54.Xu Y, Stavrides-Eid M, Baig A, et al. Quantifying treatment delays in adolescents and young adults with cancer at McGill University. Current Oncol. 2015;22:e470–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Roth ME, O’Mara AM, Seibel NL, et al. Low enrollment of adolescents and young adults onto cancer trials: insights from the community clinical oncology program. J Oncol Pract. 2016;12:e388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Landwehr MS, Watson SE, Macpherson CF, et al. The cost of cancer: a retrospective analysis of the financial impact of cancer on young adults. Cancer Med. 2016;5:863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Freyer DR. Making ends meet: financial issues from the perspectives of patients and their health-care team In: Bleyer A, Barr R, Ries LA, et al. , editors. Cancer in Adolescents and Young Adults. Hamilton, Canada: Springer International Publishing; 2017. p 667–685. [Google Scholar]
- 58.Guy GP Jr, Yabroff KR, Ekwueme DU, et al. Estimating the health and economic burden of cancer among those diagnosed as adolescents and young adults. Health Aff (Millwood). 2014;33:1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cantor JC, Belloff D, Monheit AC, et al. Expanding dependent coverage for young adults: lessons from state initiatives. J Health Polit Policy Law. 2012;37:99–128. [DOI] [PubMed] [Google Scholar]


