Abstract
We assessed the association between metabolic health and markers of inflammation and of endothelial dysfunction using data from the Ewha Birth and Growth Cohort Study. The data of 195 subjects aged 13–15 years were analyzed. To assess metabolic syndrome, continuous metabolic syndrome (cMets) scores were calculated. We measured the levels of high-sensitivity C-reactive protein (hs-CRP), intercellular adhesion molecule 1 (ICAM-1), and vascular cell adhesion molecule 1 (VCAM-1) as markers of inflammation and endothelial dysfunction. An increase of one SD in the cMets score resulted in a 1.25-fold (95% CI 1.10–1.42) increase in the risk of acute inflammatory status and a 1.26-fold (95% CI 1.11–1.43) increase in the risk of endothelial dysfunction as defined by ICAM-1, while VCAM-1 showed a meaningless trend. Of the metabolic components, body mass index (BMI) was positively associated with elevated hs-CRP levels and high-density lipoprotein cholesterol (HDL-c) levels were negatively associated with elevated ICAM-1 levels. Additionally, a mediation analysis showed that a high BMI was directly related to elevated hs-CRP levels and indirectly related to elevated ICAM-1 levels via HDL-c. Our findings show that poor metabolic health was related to an unfavorable inflammatory status and endothelial dysfunction in adolescents.
Introduction
Metabolic syndrome is a clustering of obesity, high blood pressure, poor glucose tolerance, and dyslipidemia, and is a risk factor for cardiovascular disease (CVD). Longitudinal studies have suggested that metabolic health in later life can be traced back to childhood [1–3]. However, it is difficult to assess disease susceptibility in growing children, who vary physically and metabolically. Moreover, the prevalence of metabolic syndrome is < 5% in children and adolescents [4] and so a study requires a large sample size. The continuous metabolic syndrome (cMets) score has been proposed as an index of metabolic syndrome in children or adolescents [5] and has been evaluated extensively [2,6,7].
Regarding the effect of metabolic health on CVD development, abnormal metabolic components contribute to endothelial dysfunction accompanied by inflammation of the vessel wall, leading to the development of atherosclerosis and CVD [8]. Based on these assumptions, the associations between metabolic components and inflammatory markers (e.g., high-sensitivity C-reactive protein [hs-CRP], interleukin-6 [IL]-6) [6,9–11], and markers of endothelial dysfunction (e.g., intercellular adhesion molecule [ICAM-1] and vascular cell adhesion molecule [VCAM-1]) [6,11,12] have been evaluated. However, most studies examined adults [10,11] or had case–control designs [12,13]. Although a previous study evaluated the relationships among hs-CRP, ICAM-1, VCAM-1, and cMets in adolescents [6], evidence for children or adolescents in general is lacking.
Therefore, to determine whether a poor metabolic status is linked to levels of preclinical markers of CVD in adolescents, we assessed the cross-sectional association between metabolic components and markers of inflammation and endothelial dysfunction using data from the Ewha Birth and Growth Cohort Study. Furthermore, to identify an easily implementable and effective intervention strategy, we used mediation analysis to evaluate the direct/indirect association between BMI and an unfavorable inflammatory status and endothelial dysfunction.
Materials and methods
Subjects
This study was part of the Ewha Birth and Growth Cohort Study. This cohort was established in 2001–2006 (baseline n = 940) at the Ewha Woman’s University Mokdong Hospital (Seoul, South Korea) and was designed to investigate risk and preventive factors related to growth and disease susceptibility. Detailed information on the cohort composition and methodology has been provided elsewhere [14,15]. In 2015, a follow-up program with subjects 13 years of age was begun that involved anthropometric measurements, questionnaires, dietary surveys, and blood and urine sampling. Blood sampling was conducted after an overnight fast. During the follow-up at 13–15 years of age, blood levels of hs-CRP, ICAM-1, and VCAM-1 were measured as preclinical markers of CVD. From 2015 to 2019, 217 subjects aged 13–15 years participated in follow-up; all and their parents or guardians provided written informed consent for participation. All data was completely anonymous before author access and analysis.
For this study, subjects who met any of the following criteria were excluded: missing data for hs-CRP, ICAM-1, and VCAM-1 (n = 22), or missing data for metabolic components (n = 8). Accordingly, complete data were available for 195 subjects (93 boys and 102 girls; 175, 16, and 4 aged 13, 14, and 15 years, respectively). The study protocol was approved by the Institutional Review Board of Ewha Womans University Hospital (no. SEUMC 2019-04-034).
Indicators of metabolic health
The cMets scores were calculated based on body mass index (BMI); levels of high-density lipoprotein cholesterol (HDL-c), triglyceride (TG), and fasting glucose; and the mean arterial blood pressure (MAP). BMI (kg/m2) was calculated from the height and weight measured with the subjects wearing no shoes and light clothing using a stadiometer and a calibrated scale (GL-150, G-Tech International Co., Ltd., Uijeongbu, South Korea). The HDL-c, TG, and fasting glucose levels were measured using an automatic analyzer (Olympus AU2700; Beckman Coulter Inc., Fullerton, CA, USA). Blood pressure (BP) was measured by a trained nurse using an automatic device (BPBIO320, InBody Co., Ltd., Seoul, South Korea) with the subject in a stable position. MAP was estimated using the following formula: [(systolic BP − diastolic BP) ÷ 3] + diastolic BP.
To calculate cMets scores, the standardized z-score for the mean and standard deviation of each of five metabolic components was calculated stratified for sex but not age because the number of 14- or 15-year-old subjects was small (n = 20). Because the HDL-c level is inversely related to the cMetS score, the standardized HDL-c level was multiplied by −1. To calculate individual cMets scores, the standardized z-scores for the five components were summed. A relatively high cMets score indicates an unfavorable metabolic syndrome status.
Outcomes
We considered hs-CRP, ICAM-1, and VCAM-1 levels as the outcome variables. The hs-CRP level in fasting blood was measured by particle-enhanced immune turbidimetric assay (Cobas 8000 C702 analyzer, Roche, Mannheim, Germany). The limit of detection (LOD) for hs-CRP was 0.15 mg/dL, and values below the LOD were imputed using the equation: LOD / √2. The ICAM-1 (DCD540, R&D Systems, Minneapolis, MN, USA) and VCAM-1 (ECM340, Millipore, Billerica, MA, USA) levels were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits. Measurements of hs-CRP, ICAM-1, and VCAM-1 levels were conducted at Seegene Medical Foundation (Seoul, South Korea). In terms of quality assurance/quality control, the coefficient of variance was < 10% for all measurements. The outcome variables were evaluated continuously. Additionally, we used alternative definitions of an unfavorable inflammatory status and endothelial dysfunction because of the lack of a clinical cutoff value for children and adolescents. Endothelial dysfunction was defined as a level of ICAM-1 or VCAM-1 ≥ 75th percentile. An acute inflammatory status was defined as an hs-CRP level of > 0.3 mg/dL [10,16], which is typically used for adults.
Covariates
As demographic factors, sex, age, and monthly household income (< 3 million, 3–5 million, and ≥ 5 million KRW) were evaluated. Using a questionnaire, we collected data on the parental history of disease, physical activity, and food intake. Total energy intake for the past year was obtained from a semi-quantitative food-frequency questionnaire (FFQ) and consisted of 92 food items. The FFQ instrument was developed by expert consensus by adding beverage items (e.g., coffee intake) to the existing validated FFQ instrument [17,18]. Depending on the nature of the cohort study, the same investigative tools were used, with appropriate modifications for the age of the subjects. Individual dietary data were collected by trained dieticians during face-to-face interviews. Eating breakfast was related to a healthy dietary pattern and dietary quality [19,20], so eating breakfast daily was included as a covariate. The daily amount of time spent sedentary (e.g., watching TV, gaming) was divided into < 2 h and ≥ 2 h based on the distribution of data. The frequency of weekly vigorous-intensity physical activity (e.g., jogging, soccer, basketball, swimming) was categorized as never, 1–2 times/week, 3–4 times/week, and ≥ 5 times/week for > 20 min at a time. Exposure to secondhand smoke in households was investigated using the questionnaire.
Statistical analysis
Summary statistics are presented as means ± standard deviation (SD) for normally distributed variables, medians with interquartile range (IQR) for non-normally distributed variables, and frequencies with percentage for categorical variables. Comparison of basic characteristics according to sex was performed by Student’s t-test, Mann–Whitney U-test, and chi-squared test.
To assess the linear associations of metabolic syndrome score and metabolic components with the outcome variables, we used the Pearson correlation for ICAM-1 and the Spearman correlation for hs-CRP and VCAM-1 based on the presence or absence of a normal distribution. The effects of basic characteristics on cMets scores were estimated as a coefficient with standard error (SE) by linear regression analysis.
The association of metabolic health with inflammation and endothelial dysfunction was assessed by multiple linear regression and multiple logistic regression. Because VCAM-1 levels were not normally distributed, the values were log-transformed. Of the subjects, 50.8% had an hs-CRP level lower than LOD, so it was evaluated by multiple logistic regression. We included sex, age at participation in follow-up, monthly household income, parental history of hypertension, parental history of diabetes, weekly vigorous-intensity physical activity, TV viewing, secondhand smoking, eating breakfast, and total energy intake as covariates. Multicollinearity was assessed by variance inflation factor (VIF), which was satisfied (VIF < 2 in all models).
Furthermore, we evaluated the mediating effects of biochemical metabolic factors on the association between BMI and an unfavorable inflammatory status and endothelial dysfunction. Log-transformed TG values were used in the analysis. The covariates included were as mentioned above. All statistical analyses were conducted using SAS software (ver. 9.4; SAS Institute, Cary, NC, USA). Statistical significance was determined as a value of p < 0.05 in a two-tailed test.
Results
Of the 195 children, 47.7% (n = 93) were boys; the mean age of the subjects was 13.1 (± 0.4) years. Of the subjects, 23.1% and 14.4% had a parental history of hypertension and diabetes, respectively. Regarding weekly vigorous-intensity physical activity, 19.7% of the subjects responded “never” and 9.8% responded “> 5 times per week”. Of the subjects, 35.1% watched TV for more than 2 h a day, and 61.9% stated that they ate breakfast every day. Other than physical activity, there was no difference in basic characteristics according to sex (Table 1). Also, the basic characteristics were not associated with cMets scores (Table 2).
Table 1. Basic characteristics of the subjects.
| Total | Boys | Girls | p | |
|---|---|---|---|---|
| (n = 195) | (n = 93, 47.69%) | (n = 102, 52.31%) | ||
| Age, years | 13.12 ± 0.39 | 13.14 ± 0.41 | 13.11 ± 0.37 | 0.57 |
| Menarche | NA | NA | 88 (86.3%) | - |
| Monthly household income, KRW | ||||
| < 3 million KRW | 12 (6.35%) | 6 (6.52%) | 6 (6.19%) | 0.96 |
| 3–5 million KRW | 56 (29.63%) | 28 (30.43%) | 28 (28.87%) | |
| ≥ 5 million KRW | 121 (64.02%) | 58 (63.04%) | 63 (64.95%) | |
| Maternal education level | ||||
| Graduated from high school | 37 (19.68%) | 17 (18.68%) | 20 (20.62%) | 0.88 |
| Some college or higher | 151 (80.32%) | 74 (81.32%) | 77 (79.38%) | |
| Parental disease history | ||||
| HTN | 45 (23.08%) | 17 (18.28%) | 28 (27.45%) | 0.18 |
| DM | 28 (14.36%) | 13 (13.98%) | 15 (14.71%) | > 0.99 |
| Weekly vigorous-intensity physical activity | ||||
| Never | 38 (19.69%) | 12 (12.90%) | 26 (26.00%) | 0.02 |
| 1–2 times/week | 73 (37.82%) | 32 (34.41%) | 41 (41.00%) | |
| 3–4 times/week | 63 (32.64%) | 36 (38.71%) | 27 (27.00%) | |
| ≥ 5 times/week | 19 (9.84%) | 13 (13.98%) | 6 (6.00%) | |
| TV viewing | ||||
| ≥ 2 h/day | 67 (35.08%) | 30 (32.61%) | 37 (37.37%) | 0.59 |
| Secondhand smoking | ||||
| Yes | 17 (8.90%) | 5 (5.43%) | 12 (12.12%) | 0.17 |
| Total energy intake, kcal/d | 2160.00 ± 594.22 | 2197.59 ± 523.46 | 2125.83 ± 652.72 | 0.40 |
| Eating breakfast | ||||
| Everyday | 117 (61.90%) | 59 (65.56%) | 58 (58.59%) | 0.40 |
Abbreviations: KRW, Korean Won; HTN, hypertension; DM, diabetes mellitus; NA, not applicable.
Table 2. Effect of subjects’ characteristics on cMetS scores.
| Coefficient (SE) | p | |
|---|---|---|
| Age, years | 0.27 (0.53) | 0.60 |
| Sex | ||
| Boys | ref | |
| Girls | 0.00 (0.41) | > 0.99 |
| Monthly household income, KRW | ||
| <3 million KRW | ref | |
| 3-<5 million KRW | 1.23 (0.91) | 0.18 |
| 5≥ million KRW | 0.74 (0.86) | 0.40 |
| Maternal education level | ||
| Graduated from high school | ref | |
| Some college or higher | -0.52 (0.52) | 0.32 |
| Parental disease history, HTN | ||
| No | ref | |
| Yes | 0.11 (0.48) | 0.82 |
| Parental disease history, DM | ||
| No | ref | |
| Yes | 0.53 (0.58) | 0.36 |
| Weekly vigorous-intensity physical activity | ||
| never | ref | |
| 1–2 times/week | 0.54 (0.57) | 0.34 |
| 3–4 times/week | -0.54 (0.58) | 0.35 |
| ≥5 times/week | 0.69 (0.79) | 0.39 |
| TV viewing | ||
| < 2 hours/day | ref | |
| ≥ 2 hours/day | -0.06 (0.43) | 0.89 |
| Secondhand smoking | ||
| No | ref | |
| Yes | -0.13 (0.73) | 0.85 |
| Total energy intake, per 100kcal | 0.03 (0.04) | 0.47 |
| Eating breakfast | ||
| Others | ref | |
| Everyday | -0.34 (0.43) | 0.42 |
Abbreviation: S.E, standard error; KRW, Korean Won; HTN, hypertension; DM, diabetes mellitus.
Summary statistics of metabolic components and markers of inflammation and endothelial dysfunction, including cMets scores, are listed in Table 3. The mean cMets score was comparable in boys and girls. Among metabolic components, the average TG level was significantly higher in girls than in boys, but other components did not differ significantly. Of the subjects, 8.7% (n = 17) had a BMI of ≥ 25.0 kg/m2. Mean hs-CRP, ICAM-1, and VCAM-1 levels were 0.1 mg/dL, 203.9 ng/mL, and 878.2 ng/mL, respectively, and were higher in boys than in girls. The mean differences by sex were significant for hs-CRP (p = 0.03) and VCAM-1 (p < 0.001). cMets scores were positively correlated with hs-CRP and ICAM-1 levels but negatively correlated with VCAM-1 levels. In addition, the correlation between BMI and hs-CRP was moderate (rs = 0.43, p < 0.001) and that between HDL-c and hs-CRP (rs = −0.20, p < 0.01) and ICAM-1 (r = −0.26, p < 0.01) was weak (Table 3).
Table 3. Descriptive statistics and correlation coefficients between metabolic syndrome components, scores, and markers of inflammation and endothelial dysfunction.
| Descriptive summary | Correlation coefficient | ||||||
|---|---|---|---|---|---|---|---|
| Total | Boys | Girls | p | hs-CRPa | ICAM-1 | VCAM-1a | |
| (n = 195) | (n = 93, 47.69%) | (n = 102, 52.31%) | |||||
| Metabolic components | |||||||
| BMI, kg/m2 | 20.39 ± 3.14 | 20.50 ± 3.37 | 20.29 ± 2.93 | 0.64 | 0.43 (p<0.001) | 0.11 (p = 0.13) | -0.16 (p = 0.02) |
| MAP, mmHg | 81.17 ± 8.47 | 81.83 ± 8.97 | 80.56 ± 7.98 | 0.30 | 0.09 (p = 0.21) | 0.15 (p = 0.04) | 0.09 (p = 0.23) |
| Fasting glucose, mg/dL | 93.05 ± 6.53 | 93.19 ± 5.85 | 92.92 ± 7.12 | 0.77 | -0.14 (p = 0.06) | 0.11 (p = 0.11) | 0.08 (p = 0.25) |
| TG, mg/dL | 62.00 | 56.00 | 66.50 | 0.02 | 0.01 (p = 0.88) | 0.08 (p = 0.28) | -0.16 (p = 0.02) |
| (49.00–84.00) | (44.00–78.00) | (54.00–88.00) | |||||
| HDL-c, mg/dL | 52.10 ± 9.77 | 52.25 ± 8.64 | 51.96 ± 10.73 | 0.84 | -0.20 (p<0.01) | -0.26 (p<0.01) | 0.02 (p = 0.84) |
| cMets score | 0.00 ± 2.83 | 0.00 ± 2.85 | 0.00 ± 2.83 | > 0.99 | 0.20 (p<0.01) | 0.26 (p<0.01) | -0.06 (p = 0.45) |
| hs-CRP, mg/dL | 0.11 (0.11–0.38) | 0.19 (0.11–0.45) | 0.11 (0.11–0.33) | 0.03 | - | - | - |
| ICAM-1, ng/mL | 203.88 ± 65.24 | 211.51 ± 63.44 | 196.92 ± 66.38 | 0.12 | - | - | - |
| VCAM-1, ng/mL | 878.20 | 945.99 | 802.26 | <0.001 | - | - | - |
| (760.53–1039.26) | (852.51–1109.51) | (716.39–939.63) | |||||
Abbreviations: BMI, body mass index; MAP, mean arterial pressure; TG, triglyceride; HDL-c, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule; VCAM-1, vascular cell adhesion molecule; cMets, continuous metabolic syndrome.
aCorrelation coefficients and p-values were obtained by the Spearman correlation method.
The associations between metabolic health and markers of endothelial dysfunction are listed in Table 4. The ICAM-1 level tended to increase by 5.6 (SE 1.6) as the cMets score increased by one SD, while the ICAM-1 level tended to decrease by 1.4 (SE 0.5) as the HDL-c level increased by 1 mg/dL. The metabolic components, including cMets scores, were not associated with log-transformed VCAM-1 levels.
Table 4. Results of multiple regression analysis of the effect of metabolic syndrome score and its components on the levels of markers of endothelial dysfunction in adolescents.
| Outcome variables | |||
|---|---|---|---|
| Independent variables | ICAM-1 | VCAM-1 b | |
| Model 1a | cMets score | 5.58 (1.64)** | 0.0003 (0.01) |
| Model 2 a | BMI, kg/m2 | 0.73 (1.71) | -0.01 (0.01) |
| MAP, mmHg | 0.41 (0.60) | 0.002 (0.002) | |
| Fasting glucose, mg/dL | 0.33 (0.74) | 0.003 (0.003) | |
| TG, mg/dL | 0.12 (0.14) | -0.0002 (0.001) | |
| HDL-c, mg/dL | -1.36 (0.53)* | -0.002 (0.002) | |
Abbreviation: BMI, body mass index; MAP, mean arterial pressure; TG, triglyceride; HDL-c, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule; VCAM-1, vascular cell adhesion molecule; cMets, continuous metabolic syndrome.
Results are coefficients with standard errors.
*p < 0.05,
**p < 0.01.
aCoefficients and p-values were obtained after adjustment for sex, age, monthly household income, parental history of hypertension, parental history of diabetes, weekly vigorous-intensity physical activity, TV viewing, secondhand smoking, eating breakfast, and total energy intake.
bVCAM-1 did not satisfy a normal distribution, and so was log transformed.
To consider inflammatory and endothelial dysfunction status, the effect of metabolic health was assessed as an odds ratio (OR) under controlling covariates (Table 5). As the cMets score increased by one SD, the risk of acute inflammatory status increased 1.25-fold (95% confidence interval [CI] 1.10–1.42) and the risk of endothelial dysfunction increased 1.26-fold (95% CI 1.11–1.43) based on ICAM-1. Among the metabolic components, BMI was positively associated with levels of markers of acute inflammation (OR = 1.35, 95% CI 1.17–1.56). In addition, the higher the HDL-c level, the greater the protective effect against endothelial dysfunction based on ICAM-1 (OR = 0.95, 95% CI 0.90–0.99). However, none of the metabolic markers, including cMets scores, was significantly associated with elevated VCAM-1 levels.
Table 5. Adjusted odds ratios for endothelial dysfunction and risk of acute inflammation according to the metabolic syndrome score and its components in adolescents.
| Outcome variables | ||||
|---|---|---|---|---|
| Independent variables | hs-CRPb | ICAM-1c | VCAM-1c | |
| Model 1a | cMets score | 1.25 (1.10–1.42)** | 1.26 (1.11–1.43)** | 0.98 (0.86–1.11) |
| Model 2a | BMI, kg/m2 | 1.35 (1.17–1.56)** | 1.11 (0.98–1.27) | 0.88 (0.76–1.01) |
| MAP, mmHg | 1.04 (0.99–1.09) | 1.01 (0.97–1.06) | 1.03 (0.98–1.07) | |
| Fasting glucose, mg/dL | 0.98 (0.93–1.04) | 1.01 (0.96–1.07) | 1.01 (0.94–1.07) | |
| TG, mg/dL | 0.99 (0.98–1.00) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) | |
| HDL-c, mg/dL | 0.97 (0.93–1.02) | 0.95 (0.90–0.99)* | 0.99 (0.95–1.04) | |
Abbreviation: BMI, body mass index; MAP, mean arterial pressure; TG, triglyceride; HDL-c, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule; VCAM-1, vascular cell adhesion molecule; cMets, continuous metabolic syndrome.
Results are odds ratios with 95% confidence intervals.
*p < 0.05,
**p < 0.001.
aOdds ratio and 95% confidence intervals were calculated after adjustment for sex, age, monthly household income, parental history of hypertension, parental history of diabetes, weekly vigorous-intensity physical activity, TV viewing, secondhand smoking, eating breakfast, and total energy intake.
bAcute inflammatory status was defined as a level > 0.3 mg/dL.
cEndothelial dysfunction was alternatively defined as ≥ 75th percentile.
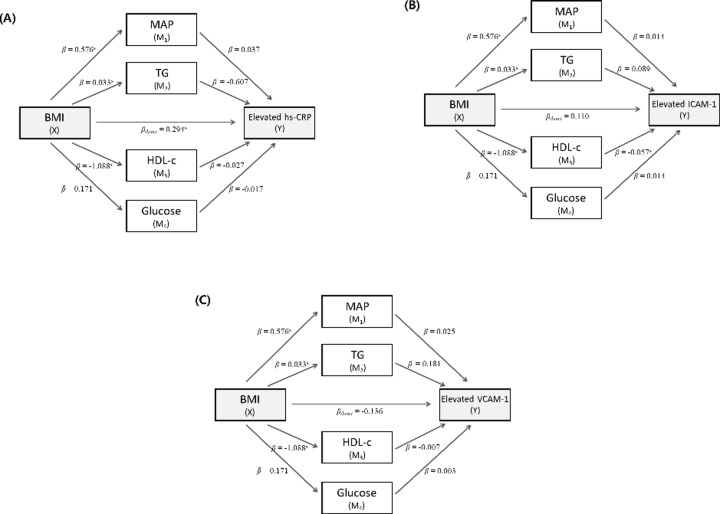
The mediating effects of biochemical metabolic factors on the association between BMI and unfavorable inflammatory status and endothelial dysfunction are shown in Fig 1. The direct effect of BMI on an elevated hs-CRP level was significant (ß = 0.29, p < 0.001), while the indirect effects of biochemical factors were not significant (Fig 1A) after adjustment for four biochemical factors. Regarding the association between BMI and an elevated ICAM-1 level, the HDL-c level showed an independent indirect effect (BMI → HDL-c, ß = −1.09, p < 0.001; HDL-c → elevated ICAM-1, ß = −0.06, p = 0.03). However, the direct effect of BMI on an elevated ICAM-1 level was not significant (Fig 1B). Neither the direct nor the indirect effect of BMI on elevated VCAM-1 levels was significant (Fig 1C).
Fig 1.
Effects of metabolic factors on the association between BMI and elevated levels of hs-CRP (A), ICAM-1 (B), and VCAM-1 (C). Abbreviation: BMI, body mass index; MAP, mean arterial pressure; TG, triglyceride; HDL-c, high-density lipoprotein cholesterol; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule; VCAM-1, vascular cell adhesion molecule. ap<0.05.
Discussion
In this study, poor metabolic health, as assessed by cMets scores, was independently associated with hs-CRP and ICAM-1 levels in adolescents. Among the metabolic components, the risk of an elevated hs-CRP level increased with increasing BMI and the risk of an elevated ICAM-1 level increased with decreasing HDL-c. Moreover, a high BMI was directly related to elevated hs-CRP levels and indirectly related to elevated ICAM-1 levels via HDL-c.
Studies have shown that ICAM-1 and VCAM-1 levels are elevated in patients with atherosclerosis, and the baseline ICAM-1 level is reportedly significantly associated with incident myocardial infarction [21] and carotid atherosclerosis [22]. ICAM-1 and VCAM-1 have been proposed as early biomarkers of changes in the artery wall [23] and to play a major role in the development of atherosclerosis; therefore, both are considered preclinical markers of endothelial dysfunction. In addition, both ICAM-1 and VCAM-1 belong to the immunoglobulin superfamily, and so are markers of inflammation and are correlated with other inflammatory markers. Briefly, as atherosclerosis progresses, increased secretion of tumor necrosis factor (TNF)-α and IL-1 induces production of IL-6 in activated monocytes and vascular smooth muscle cells, which enhances hepatic CRP synthesis. In response to TNF-α and IL-1, macrophages and endothelial cells produce ICAM-1 and VCAM-1 [24–26]. Endothelial dysfunction can be caused by metabolic syndrome, smoking, and insufficient physical activity [27], and lesions in the vessel wall can begin to grow slowly during childhood and develop in adolescence and adulthood [25].
Similar to our study, a Young Heart Project 2000 study assessed the relationships among hs-CRP, ICAM-1, VCAM-1, and cMets in adolescents [6]; the main findings were consistent with our results. However, this study involved 1:1-matched overweight and normal-weight adolescents, so its summary statistics may differ from the general population of adolescents. Our study also found that cMets scores were independently associated with levels of ICAM-1 but not of VCAM-1. This is consistent with the results of a study involving adults [11]. Regarding the association between metabolic components and markers of endothelial dysfunction, a positive association with TG [28] and insulin resistance [29], and a negative association with HDL-c [30] have been reported. We found a significant relationship between HDL-c and ICAM-1. This may be because HDL-c inhibits expression of endothelial adhesion molecules [31]. By contrast, there was no significant association between metabolic health and VCAM-1 levels. The biological responses of ICAM-1 and VCAM-1 have been reported [25,32], but the mechanisms underlying the changes in ICAM-1 and VCAM-1 levels are unclear [6,33]. In addition, it has been proposed that ICAM-1 may be predictive of cardiovascular events in adults, and VCAM-1 may be a prognostic factor in patients with atherosclerosis [25]. Therefore, caution is needed when interpreting the clinical implications of VCAM-1 levels in children and adolescents.
hs-CRP is a nonspecific marker of inflammation and evidence has implied that hs-CRP levels are associated with metabolic syndrome and are predictive of CVD development [10, 11]. Although the relationship between metabolic components and hs-CRP levels is unclear, several studies in children and adolescents [6,9,16], and in adults [10,11] have reported a significant positive association between metabolic syndrome and hs-CRP levels. In addition, hs-CRP levels are reportedly correlated with the severity of CVD. A case study in patients with angina reported that the number of metabolic syndrome components was positively associated with the severity of coronary atherosclerosis and hs-CRP levels were positively correlated with the number of metabolic syndrome components and the severity of coronary atherosclerosis [34]. A previous study also reported that BMI was independently associated with elevated CRP levels [9], in agreement with our results. Furthermore, the 2-year Preventing Overweight Using Novel Dietary Strategies (POUNDS) LOST study revealed that weight loss exerted a favorable effect on hs-CRP levels [35]. A longitudinal follow-up study also found that subjects with rapid weight gain had a higher risk of elevated CRP [36]. In this study, BMI, but not the other metabolic components, was directly associated with elevated hs-CRP levels. The association of BMI with elevated ICAM-1 levels was mediated by HDL-c. Therefore, BMI was directly or indirectly related to high hs-CRP and ICAM-1 levels, both markers of CVD. BMI was also associated with unfavorable metabolic conditions (high MAP and TG and low HDL-c). A possible mechanism underlying these associations may be that the composition and function of adipose tissue are altered in obesity, leading to the synthesis and secretion of various inflammatory mediators (e.g., adipokines, cytokines, and chemokines). Adipokines produced in adipose tissue help to regulate lipid metabolism, immunity, and inflammation processes, and are also associated with subsequent endothelial dysfunction [37]. Our results support this mechanism, and it is noteworthy that the relevance was confirmed in an observational study of adolescents rather than an experimental study. Childhood obesity can lead to obesity in adulthood [38]. Therefore, to reduce the risk of CVD, it is important that normal weight be maintained from a young age.
There is need for caution in interpreting the findings of this study. Because the subjects were not representative of the South Korean population, the generalizability of the results is limited. However, this study involved the general population rather than being a case-control design. Also, this was a cross-sectional study, so the temporal relevance is unclear. Errors in biomarker measurements can lead to non-differential bias, rendering the estimated values meaningless. We have not evaluated various indicators related to inflammation or endothelial dysfunction, such as TNF-a and IL-6. Therefore, further large-scale studies are needed to evaluate the feasibility of the study results for various indicators. Nevertheless, our findings have shown significant relevance that is consistent with previous studies. In addition, because various factors contribute to the development of CVD, we considered a number of covariates. However, the residual effects of unmeasured factors may have affected the results. Finally, the direct and indirect effects of BMI on an unfavorable inflammatory status and endothelial dysfunction were evaluated by mediation analysis, which may help further understanding.
In summary, poor metabolic health, as assessed by cMets scores, was related to an unfavorable inflammatory status and endothelial dysfunction in adolescents. Hence, maintaining metabolic health, particularly maintaining a normal weight, may prevent the development of CVD in later life.
Data Availability
All relevant data are within the manuscript.
Funding Statement
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A1B03030088). It had no role in the design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Katzmarzyk PT, Pérusse L, Malina RM, Bergeron J, Després JP, Bouchard C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: the Québec Family Study. J Clin Epidemiol. 2001;54(2): 190–195. 10.1016/s0895-4356(00)00315-2 [DOI] [PubMed] [Google Scholar]
- 2.Bao W, Srinivasan SR, Wattigney WA, Berenson GS. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart Study. Arch Intern Med. 1994;154(16): 1842–1847. [PubMed] [Google Scholar]
- 3.Hulsegge G, Spijkerman AM, van der Schouw YT, Bakker SJ, Gansevoort RT, Smit HA, et al. Trajectories of Metabolic Risk Factors and Biochemical Markers prior to the Onset of Cardiovascular Disease - The Doetinchem Cohort Study. PLoS One. 2016;11(5):e0155978 10.1371/journal.pone.0155978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee HA, Park H. Overview of noncommunicable diseases in Korean children and adolescents: Focus on obesity and its effect on metabolic syndrome. J Prev Med Public Health. 2013;46: 173–182. 10.3961/jpmph.2013.46.4.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shafiee G, Kelishadi R, Heshmat R, Qorbani M, Motlagh ME, Aminaee T, et al. First report on the validity of a continuous Metabolic syndrome score as an indicator for Metabolic syndrome in a national sample of paediatric population - the CASPIAN-III study. Endokrynol Pol. 2013;64(4): 278–284. 10.5603/ep.2013.0006 [DOI] [PubMed] [Google Scholar]
- 6.Wijnstok NJ, Twisk JW, Young IS, Woodside JV, McFarlane C, McEneny J, et al. Inflammation markers are associated with cardiovascular diseases risk in adolescents: the Young Hearts project 2000. J Adolesc Health. 2010;47(4): 346–351. 10.1016/j.jadohealth.2010.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee HA, Park SH, Hong YS, Ha EH, Park H. The Effect of Exposure to Persistent Organic Pollutants on Metabolic Health among KOREAN Children during a 1-Year Follow-Up. Int J Environ Res Public Health. 2016;13(3). pii: E270. 10.3390/ijerph13030270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koh KK, Han SH, Quon MJ. Inflammatory markers and the metabolic syndrome: insights from therapeutic interventions. J Am Coll Cardiol. 2005;46(11): 1978–1985. 10.1016/j.jacc.2005.06.082 [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Ajani UA, Mokdad AH. National Health and Nutrition Examination. The metabolic syndrome and concentrations of C-reactive protein among U.S. youth. Diabetes Care. 2005;28(4): 878–881. 10.2337/diacare.28.4.878 [DOI] [PubMed] [Google Scholar]
- 10.Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation. 2003;107(3): 391–397. 10.1161/01.cir.0000055014.62083.05 [DOI] [PubMed] [Google Scholar]
- 11.Pischon T, Hu FB, Rexrode KM, Girman CJ, Manson JE, Rimm EB. Inflammation, the metabolic syndrome, and risk of coronary heart disease in women and men. Atherosclerosis. 2008;197(1): 392–399. 10.1016/j.atherosclerosis.2007.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Shorman A, Al-Domi H, Faqih A. Markers of subclinical atherosclerosis in schoolchildren with obesity and metabolic syndrome. Swiss Med Wkly. 2017;147:w14446 10.4414/smw.2017.14446 [DOI] [PubMed] [Google Scholar]
- 13.Glowinska B, Urban M, Peczynska J, Florys B. Soluble adhesion molecules (sICAM-1, sVCAM-1) and selectins (sE selectin, sP selectin, sL selectin) levels in children and adolescents with obesity, hypertension, and diabetes. Metabolism. 2005;54(8): 1020–1026. 10.1016/j.metabol.2005.03.004 [DOI] [PubMed] [Google Scholar]
- 14.Lee HA, Park EA, Cho SJ, Kim HS, Kim YJ, Lee H, et al. Mendelian randomization analysis of the effect of maternal homocysteine during pregnancy, as represented by maternal MTHFR C677T genotype, on birth weight. J. Epidemiol. 2013; 23: 371–375. 10.2188/jea.JE20120219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee HA, Kim YJ, Lee H, Gwak HS, Hong YS, Kim HS, et al. The preventive effect of breast-feeding for longer than 6 months on early pubertal development among children aged 7–9 years in Korea. Public Health Nutr. 2015; 18: 3300–3307. 10.1017/S1368980015000518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim YH, Park HA, Kang JH, Lee SH, Kim SH, Kim MJ, et al. C-reactive Protein, Obesity, and Cardiovascular Risk Factors in 7 Years-old Korean Children. J Korean Acad Fam Med 2007;28: 509–514. [Google Scholar]
- 17.Oh SY, Chung J, Kim M, Kwon SO, Cho BH. Antioxidant nutrient intakes and corresponding biomarkers associated with the risk of atopic dermatitis in young children. Eur J Clin Nutr. 2010; 64: 245–252. 10.1038/ejcn.2009.148 [DOI] [PubMed] [Google Scholar]
- 18.Chung J, Kwon SO, Ahn H, Hwang H, Hong SJ, Oh SY. Association between dietary patterns and atopic dermatitis in relation to GSTM1 and GSTT1 polymorphisms in young children nutrients. Nutrients. 2015:7: 9440–9452. 10.3390/nu7115473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee HA, Hwang HJ, Oh SY, Park EA, Cho SJ, Kim HS, et al. Which Diet-Related Behaviors in Childhood Influence a Healthier Dietary Pattern? From the Ewha Birth and Growth Cohort. Nutrients. 2017; 9(1): 4 10.3390/nu9010004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee HA, Park H. The mediation effect of individual eating behaviours on the relationship between socioeconomic status and dietary quality in children: the Korean National Health and Nutrition Examination Survey. Eur J Nutr. 2017;56(3): 1339–1346. 10.1007/s00394-016-1184-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ridker PM, Hennekens CH, Roitman-Johnson B, Stampfer MJ, Allen J. Plasma concentration of soluble intercellular adhesion molecule 1 and risks of future myocardial infarction in apparently healthy men. Lancet. 1998; 351: 88–92. 10.1016/S0140-6736(97)09032-6 [DOI] [PubMed] [Google Scholar]
- 22.Hwang SJ, Ballantyne CM, Sharrett AR, Smith LC, Davis CE, Gotto AM Jr, et al. Circulating adhesion molecules VCAM-1, ICAM-1, and E-selectin in carotid atherosclerosis and incident coronary heart disease cases: the Atherosclerosis Risk In Communities (ARIC) study. Circulation. 1997; 96: 4219–4225. 10.1161/01.cir.96.12.4219 [DOI] [PubMed] [Google Scholar]
- 23.Gross MD, Bielinski SJ, Suarez-Lopez JR, Reiner AP, Bailey K, Thyagarajan B, et al. Circulating soluble intercellular adhesion molecule 1 and subclinical atherosclerosis: the Coronary Artery Risk Development in Young Adults Study. Clin Chem. 2012;58(2):411–420. 10.1373/clinchem.2011.168559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blake GJ, Ridker PM. Novel clinical markers of vascular wall inflammation. Circ Res. 2001;89(9): 763–771. 10.1161/hh2101.099270 [DOI] [PubMed] [Google Scholar]
- 25.Fotis L, Giannakopoulos D, Stamogiannou L, Xatzipsalti M. Intercellular cell adhesion molecule-1 and vascular cell adhesion molecule-1 in children. Do they play a role in the progression of atherosclerosis? Hormones (Athens). 2012;11(2): 140–146. [DOI] [PubMed] [Google Scholar]
- 26.Kim SK. Inflammatory Markers in Coronary Artery Disease. Korean Circulation J 2001;31(7): 617–619. [Google Scholar]
- 27.Rajendran P, Rengarajan T, Thangavel J, Nishigaki Y, Sakthisekaran D, Sethi G, et al. The Vascular Endothelium and Human Diseases. Int J Biol Sci. 2013; 9(10): 1057–1069. 10.7150/ijbs.7502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kavazarakis E, Moustaki M, Gourgiotis D, Zeis PM, Bossios A, Mavri A, et al. The impact of serum lipid levels on circulating soluble adhesion molecules in childhood. Pediatr Res. 2002;52(3): 454–458. 10.1203/00006450-200209000-00025 [DOI] [PubMed] [Google Scholar]
- 29.Valle Jiménez M, Estepa RM, Camacho RM, Estrada RC, Luna FG, Guitarte FB. Endothelial dysfunction is related to insulin resistance and inflammatory biomarker levels in obese prepubertal children. Eur J Endocrinol. 2007;156(4): 497–502. 10.1530/EJE-06-0662 [DOI] [PubMed] [Google Scholar]
- 30.Ohta T, Saku K, Takata K, Adachi N. Soluble vascular cell-adhesion molecule-1 and soluble intercellular adhesion molecule-1 correlate with lipid and apolipoprotein risk factors for coronary artery disease in children. Eur J Pediatr. 1999;158: 592–598. 10.1007/s004310051154 [DOI] [PubMed] [Google Scholar]
- 31.Cockerill GW, Rye KA, Gamble JR, Vadas MA, Barter PJ. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arterioscler Thromb Vasc Biol. 1995;15(11): 1987–1994. 10.1161/01.atv.15.11.1987 [DOI] [PubMed] [Google Scholar]
- 32.Bosanská L, Michalský D, Lacinová Z, Dostálová I, Bártlová M, Haluzíková D, et al. The influence of obesity and different fat depots on adipose tissue gene expression and protein levels of cell adhesion molecules. Physiol Res. 2010;59(1): 79–88. [DOI] [PubMed] [Google Scholar]
- 33.Isoppo de Souza C, Rosa DD, Ettrich B, Cibeira GH, Giacomazzi J, Tusset P, et al. Association of adipokines and adhesion molecules with indicators of obesity in women undergoing mammography screening. Nutr Metab (Lond). 2012;9(1): 97 10.1186/1743-7075-9-97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noh HJ, Kwon NH, Joo SB. Severity of Coronary Atherosclerosis; Influence of Metabolic Syndrome Risk Factor Clustering and hs-CRP. Korean Circulation J. 2006;36: 802–808. [Google Scholar]
- 35.Nicklas JM, Sacks FM, Smith SR, LeBoff MS, Rood JC, Bray GA, et al. Effect of dietary composition of weight loss diets on high-sensitivity c-reactive protein: the Randomized POUNDS LOST trial. Obesity (Silver Spring). 2013;21(4): 681–689. 10.1002/oby.20072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thompson AL, Koehler E, Herring AH, Paynter L, Du S, Zhang B, et al. Weight Gain Trajectories Associated With Elevated C-Reactive Protein Levels in Chinese Adults. J Am Heart Assoc. 2016;5(9). pii: e003262. 10.1161/JAHA.116.003262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwaifa IK, Bahari H, Yong YK, Noor SM. Endothelial Dysfunction in Obesity-Induced Inflammation: Molecular Mechanisms and Clinical Implications. Biomolecules. 2020;10(2). pii: E291. 10.3390/biom10020291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2): 95–107. 10.1111/obr.12334 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript.