Introduction
Web-Objective Structured Clinical Examination (OSCEs) were piloted for the Clinical Skills Assessment (CSA) exams in the USA two decades ago and were shown to be an acceptable way to conduct OSCEs remotely. The learners valued the process yet expressed numerous limitations. 1 In response to the COVID-19 outbreak in Qatar, medical schools stopped in-person teaching creating a hiatus in clinical instruction. The Clinical Skills and Simulation Lab (CSSL) team devised and piloted a Web-OSCE to determine its feasibility in this setting, and to evaluate stakeholders’ experiences.
We describe the steps taken to create a Web-OSCE built on women’s reproductive and sexual health which is part of the third year Obstetrics and Gynecology Clerkship curriculum, using Zoom teleconferencing. It mirrored the steps taken when conducting this activity in person; however, all communication relied on emails before the event, Zoom during the event with WhatsApp as a backup for connectivity between learners, Zoom hosts and faculty.
Methods
Pre-Web-OSCE steps
Preparing students
CSSL provided by email a step-by-step instruction guide plus a pre-OSCE task for students to complete to ensure that they could access the OSCE on the day of the activity. A live Zoom session led by faculty reviewed the learning objectives, expectations and assessment and served as an open forum for students to ask questions in order to mitigate any anxiety surrounding the new modality.
Preparing simulated patients
Simulated patients (SP) were surveyed to assess their interest and technology capabilities to participate in Zoom activities. Interested SPs joined a Zoom meeting with staff members, who ensured they had adequate technical capability. SPs were selected and confirmed according to requirements of the case. Training notes and checklists were sent in advance to all. Observers helped capture the details of the encounter for SP checklist completion, as encounters were not recorded. Case training was done as normal, only in Zoom.
Pilot OSCE
A dry run pilot OSCE was conducted with SPs, faculty and staff to ensure all stakeholders had the opportunity to become familiar with the Zoom technology and processes required to conduct the Web-OSCE. It highlighted potential challenges and tested the achievability of the desired learning objectives in the new medium.
Web-OSCE steps
Figure 1 illustrates the journey of a learner and SP, from prebrief to debrief. All participants interact via Zoom teleconferencing using their own devices with audio/video capability and access to high-speed internet.
Figure 1.
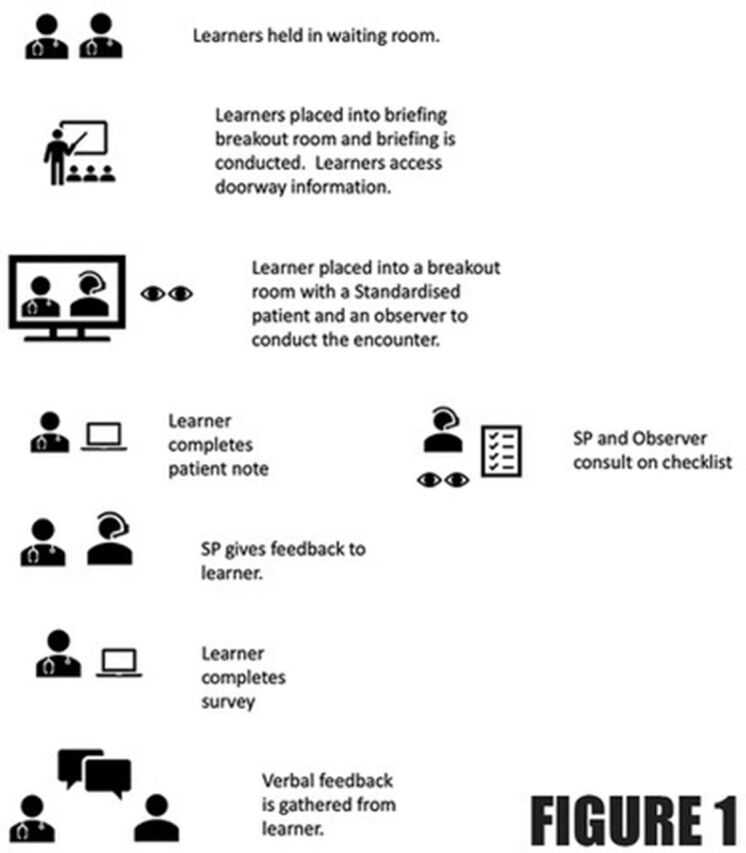
The figure was illustrated by JV using Microsoft Office icons. These icons are free to use and there is no royalty nor copyright. SP, simulated patient.
SPs and observers arrive before learners and are admitted by cohost 1. Cohost 2 renames them (SP1…Obs1…) while host ensures sufficient audio/video quality, conducts SP briefing and assigns them to their breakout rooms. Observers mute audio and turn off video while the student is in the breakout room.
Students are admitted by host into the main session to join and be briefed in briefing breakout room. Cohost 3 instructs students to log into the Learning Management System (LMS).
Cohost 2 confirms that SPs are ready and host moves students to breakout rooms (student 1 to SP1, and so on). The 30 min encounter begins. Cohost 2 keeps time following an activity operational plan (online supplementary appendix 1). Host broadcasts a 10 and 5 min warning via a written banner message into the breakout rooms while cohost 2 verbally announces into each breakout room. Host broadcasts a written message at the end of the encounter and joins each breakout room to move students to the postencounter area. SPs and observers turn on audio/video to discuss the encounter and prepare for the SP to give feedback.
Cohost 3 instructs students to log into the LMS to complete a subjective, objective, assessment and plan (SOAP) note which automatically submits to the faculty.
Cohost 2 confirms that breakout rooms are ready and host moves students back to the breakout rooms for 10 min face-to-face feedback. Host announces end of feedback and moves all back to the main room for debriefing. SPs and observers have 40 min to complete the checklist and take a break before the next encounter.
Cohost 3 instructs students to complete a feedback survey. Cohost 4 conducts a debrief with all students, before they leave the meeting.
After concluding all encounters, SPs and observers are moved to the main session room to reflect on their experience with cohost 4 and complete an online survey.
Observing SPs submit completed student checklists. Cohost 1 enters responses and comments. Each checklist is double-checked by a second party to ensure accurate entry.
Once write-ups are reviewed by faculty, scores are generated and released to students along with SP checklist and write-up feedback.
bmjstel-2020-000629supp001.pdf (44.4KB, pdf)
Results
The activity included nine students, three SPs, three observers, one host and four cohosts and took 4.5 hours to conduct. All SPs and students responded to the online survey.
All agreed that expectations were clearly communicated, staff and equipment contributed to a positive learning experience, the activity fostered a safe learning environment and, overall, it was a valuable learning activity. Eight respondents (88%) agreed/strognly agree (SA) that the objectives of the activity were met, and that feedback had been valuable. Comments included: ‘it models the clinics and can be turned into telemedicine’ and ‘… only downfall is that we cannot do a physical exam’. SPs expressed a need for role portrayal training time as much of the training had focused on using Zoom. They remarked that checklists needed to be modified for the new platform. All valued the practice sessions, Zoom tutorials, use of WhatsApp groups and time set for dry runs.
Discussions
Devising and conducting a Web-OSCE over Zoom requires a team of meeting host/cohosts; an operational plan; a trained pool of SPs; access for all participants to reliable internet connections; and personal devices with built-in audio and video capabilities. Student, SP and faculty feedback was encouraging. We identified a need to teach telemedicine, learnt that checklists needed to be modified in rating appropriateness of student eye contact, since looking at a patient on screen means looking away from the camera. All the essential goals aside from physical exam skills could be assessed in the Web-OSCE. These included accurate history taking, communication and rapport building (ie, eye contact, active listening, and so on), critical reasoning based on elicited data and provided physical exam findings.
Acknowledgments
We acknowledge Mrs Christina Bernardo (cohost 2) and Mrs Gemma Fabricante (cohost 1) for their significant contributions, in recruitment and training of SPs, in serving as cohosts during the dry runs and actual OSCE, and in supporting post-OSCE data entry.
Footnotes
Contributors: SM: substantial contribution to the conception of the work; or the analysis and interpretation of data for the work; and drafted the work and revised it critically for important intellectual content; and prepared the final approval of the version to be published. LS: substantial contributions to the design of the work; interpretation of data for the work; and revised it critically for important intellectual content. JV: substantial contributions to the conception of the work; and the acquisition, analysis and interpretation of data for the work; and drafted the figure as well as critically revised it for important intellectual content. MJ: substantial contributions to the conception and design of the case; interpretation of data for the work; and revised critically the manuscript for important intellectual content. LS, JV and MJ contributed to the final approval of the version to be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Reference
- 1. Novack DH, Cohen D, Peitzman SJ, et al. A pilot test of WebOSCE: a system for assessing trainees' clinical skills via teleconference. Med Teach 2002;24:483–7. 10.1080/0142159021000012504 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjstel-2020-000629supp001.pdf (44.4KB, pdf)


