Abstract
Tai-Chi (TC) practice has been increasingly used to prevent falls in older adults. However, the biomechanical mechanisms underlying the effects of TC practice on fall risk among older adults remain unanswered. The objective of this pilot study was to examine how TC gait biomechanically impacts the human body in terms of dynamic gait stability and lower limb muscle strength in comparison with regular walking gait. Ten healthy adults performed five trials of TC gait following three to five trials of regular walking. Full body kinematics and kinetics were collected, and then dynamic gait stability and lower limb joint moments were determined. During TC gait, individuals were less stable, moved more slowly and experienced a larger mediolateral movement in comparison with regular walking gait. The peak moment at the ankle joint on the sagittal and transverse planes, at the knee joint on all three planes, and at the hip joint on the frontal plane was significantly different when performing TC gait than during regular gait. The results indicate that TC gait challenges body balance and requires more muscle strength of the lower limb joints compared to regular walking gait. To cope with these challenges, the body could develop neuromuscular control strategies to maintain body balance and thus reduce the risk of falls. The findings and methodology in this study could provide preliminary guidance for identifying optimal TC forms in order to maximize the effects of TC-based fall prevention interventions among various populations with elevated risk of falls.
Keywords: Tai-Chi practice, Dynamic gait stability, Limb support, Feasible Stability Region, Joint moment
INTRODUCTION
Falls are a serious public health concern among older adults. Approximately one third of older adults fall at least once annually (Tinetti, 2003). Falls can result in serious injuries such as fractures and head trauma, often cause a fear of falling, and lead to heavy economic burden to the healthcare system (McCarthy, 2016). Tremendous efforts have been devoted in developing fall prevention programs (Guirguis-Blake et al., 2018).
Tai-Chi (TC) practice has been widely used as a non-pharmacological approach to improve body balance and prevent falls in older adults (Li et al., 2019; Lomas-Vega et al., 2017; Wolf et al., 2003; Wu et al., 2016). Tai-Chi is a more than 1,200-year old traditional Chinese exercise. It is based on gentle and slow movements that represent many variations and changes such as emptiness and fullness, movement and stillness, expressed strength and softness, and forward and backward movements. Despite the positive TC-induced health benefits, such as increasing lower limb strength (Penn et al., 2019), improving flexibility (Lan et al., 1996), and enhancing balance (Hosseini et al., 2018), the underlying biomechanical mechanisms of TC practice that contributes to reducing the risk of falls among older adults are still unclear. Previous TC-based clinical trials adopted certain selected TC forms. However, the scientific reasoning of such a selection is lacking (Li et al., 2019; Li et al., 2018). Without a thorough understanding of such mechanisms, it is difficult to accurately identify and effectively implement optimal TC forms into interventions for preventing falls among older adults. The diversity in TC forms among studies could have contributed to the inconclusive findings as indicated by a recent review article that the efficacy of TC practice reducing falls in older adults is uncertain (Sherrington et al., 2019).
Dynamic gait stability (Yang et al., 2009) and limb support (Ding and Yang, 2016) have been identified as key risk factors of falls in older adults. Dynamic gait stability describes the kinematic relationship between the body’s center of mass (COM) and base of support (BOS) in the horizontal direction within the novel Feasible Stability Region theory (Pai and Patton, 1997; Yang et al., 2007). FSR is comprised of two limits: the limits against backward and forward falling (Fig. 1a). The two limits encompass all possible COM motion states which allow one to keep a balanced upright posture during gait without reestablishing the BOS. An adequate dynamic stability ensures the appropriate relationship between the body’s COM and BOS to maintain its balance in the horizontal direction. Ample leg strength, on the other hand, provides vital limb support to avoid the body collapsing vertically after an unexpected perturbation.
Fig. 1.
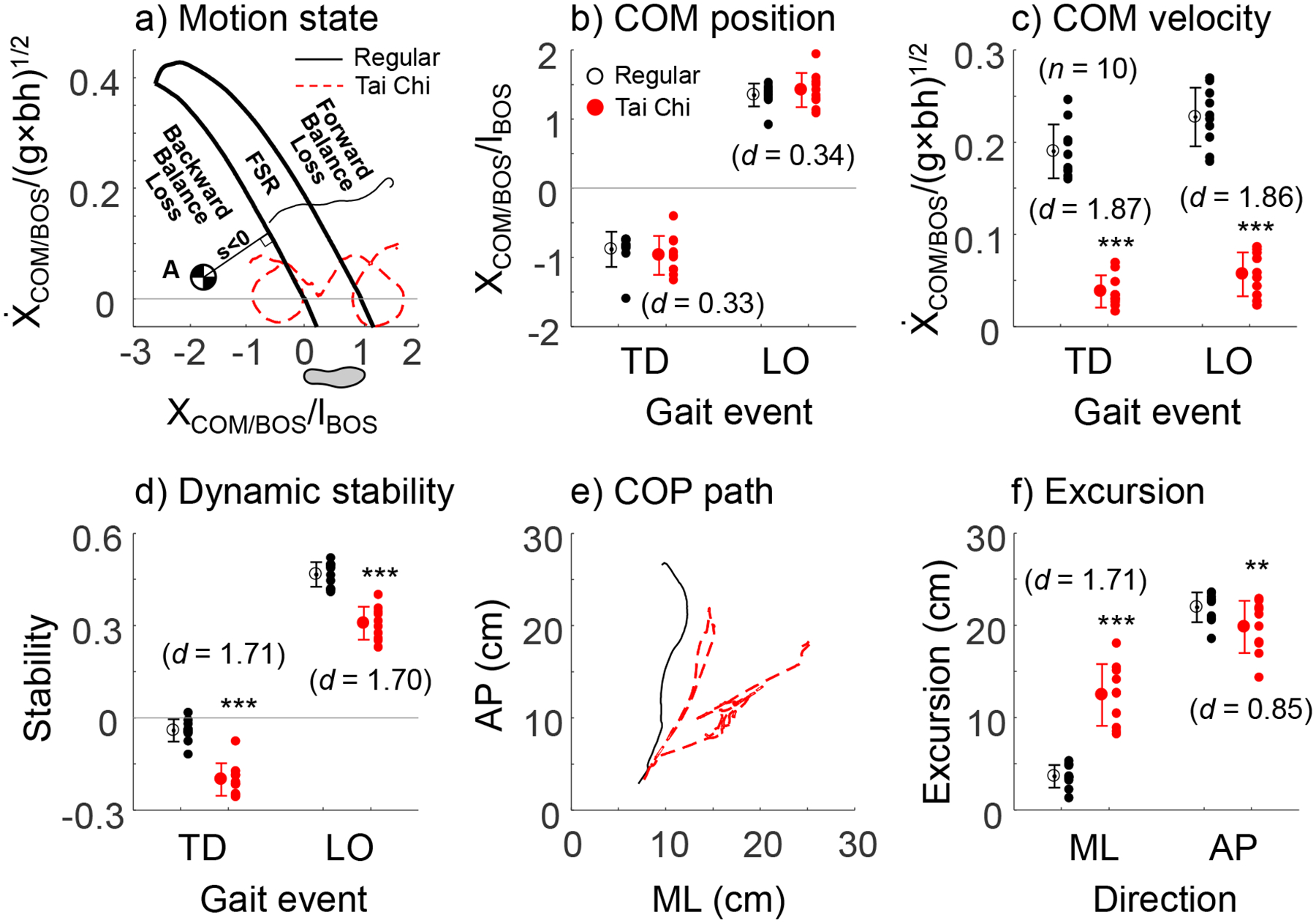
a) Demonstration of dynamic gait stability defined based on the Feasible Stability Region (FSR) theory. Unlike static stability, which only involves the relative position of the body’s center of mass (COM) to the base of support (BOS), the FSR theory considers both position and velocity of the COM with respect to its BOS. When the COM’s motion state (i.e., the combination of its position and velocity relative to the BOS) is below the lower limit of FSR (like point A), COM lacks adequate forward momentum to bring itself above the BOS. Dynamic stability is thus negative indicating an unstable state against backward falling. When a person’s COM motion state is within the FSR, the person assumes a stable upright body posture without a need to adjust the existing BOS. When the COM motion state is above the FSR, the COM has excessive forward momentum that likely leads to a forward fall. The value of dynamic stability (s) is quantified as the shortest distance from the COM motion state to FSR’s lower limit (the solid line between the motion state A and the FSR). Also shown are the COM motion state trajectories during the stance phase in Tai-Chi (TC) and regular gaits for a representative participant. Comparisons between TC and regular gaits of b) COM position, c) COM velocity, and d) dynamic gait stability at touchdown (TD) and liftoff (LO). The COM position and velocity were relative to the rear edge of the BOS and normalized by foot length (lBOS) and , respectively (where g represents the acceleration due to gravity and bh the body height). Both the COM position and velocity relative to the BOS are unitless. Therefore, dynamic gait stability is a dimensionless measurement. e) Demonstration of the center of pressure (COP) path on the transverse plane during both gaits for the participant in a). f) Comparison of the COP mediolateral (ML) and anteroposterior (AP) excursion between regular and TC gaits. COP excursion was determined as the maximal displacement of the COP path in the respective direction. Also shown is the effect size of each comparison expressed as Cohen’s d. ***: p < 0.001 vs. regular gait; **: p < 0.01 vs. regular gait.
TC gait is one of the 24 forms of Yang-style TC and is the basic but common leg motions in TC movements. It is a periodic motion with temporal patterns similar to regular gait. Given that the majority of outdoor falls occur during locomotion, like walking (Bergland et al., 2003), the purpose of this pilot study was to examine the influence of TC gait on dynamic gait stability and lower limb support among adults in comparison with regular walking gait. Examining the impact of TC practice on dynamic gait stability and limb support may provide valuable insight into the mechanisms employed by TC to help reduce falls.
METHODS
The detailed protocol of the data collection for this study can be found elsewhere (Jagodinsky et al., 2015; Liu et al., 2016). Briefly, ten healthy adults (five males, mean±SD age: 58.4±13.1 years; height: 1.73±0.08m; mass: 73.6±18.5kg) without known history of musculoskeletal disorders, neurological diseases, orthopedic and cardiovascular conditions were enrolled. All participants had minimum of two-year experience practicing TC and knowledge of the 24 simplified Yang-style TC forms. Prior to participation, all participants signed an informed consent document approved by the University Institutional Review Board (Record Number: 2016–050).
After three-seven trials of regular walking over a linear pathway embedded with two force plates (AMTI, MA) at self-selected speed and manner, all participants performed five trials of Yang-style TC gait. Full-body kinematics were collected from 37 reflective markers placed on the body’s bony landmarks (Liu et al., 2016) using a motion capture system (Vicon, UK) sampling at 100Hz. Ground reaction force data were recorded synchronously with the kinematic data at a sampling frequency of 1,000Hz.
The last TC gait trial was chosen as the representative one and analyzed. Marker paths were low-pass filtered with a cutoff frequency of 6Hz using a 4th order, zero-lag Butterworth filter. The body COM kinematics were then computed using gender-dependent segmental inertial parameters based on the filtered marker trajectories (de Leva, 1996). The two components of the COM motion state (i.e., its position and velocity) were calculated relative to the rear of the BOS (i.e. the leading heel) and normalized by foot length (lBOS) and , respectively, where g represents the gravitational acceleration and bh the body height. Dynamic gait stability was calculated as the shortest distance from the COM motion state to the limit against backward balance loss (Fig. 1a) (Yang and Pai, 2010). Two events: touchdown (TD) and liftoff (LO), were identified based on the vertical ground reaction force. Position and velocity of the COM relative to the BOS, and dynamic gait stability were calculated at both events.
The center of pressure (COP) trace during stance phase (from TD to LO at the same side) was determined from the ground reaction force. The excursion of COP trajectory in the anteroposterior (AP) and mediolateral (ML) directions were determined as the maximal COP displacement in the respective direction. An individualized seven-segment human model that included the head-arms-trunk, bilateral thighs, legs, and feet, was developed for each participant (Pai et al., 2006; Winter, 2009). Resultant moments at the ankle, knee, and hip joints were calculated using an inverse dynamics approach based on the collected ground reaction forces and COP data. The peak value of joint moment during the stance phase was identified for all joints in all three planes and was normalized to body mass (in Nm/kg). Considering the symmetry between sides, we calculated COP and joint moments at the right limb.
All dependent variables, including COM position and velocity, dynamic gait stability, the COP excursion in AP and ML directions, and moments of three lower limb joints in all three planes, were tested for skewness using the Shapiro-Wilk test. If data violated the normal distribution, a logarithm transform would be executed. All variables were compared between TC gait and regular gait using paired t-tests with SPSS 24 (IBM) and a significance level of 0.05 was applied. The Cohen’s d was calculated as the effect size for each comparison between gait. To reduce Type I error due to the multiple t-test comparisons, the Bonferroni step-down (Holm) correction was made to the significance level.
RESULTS
At TD, the COM position relative to the BOS was comparable between gaits (−0.967±0.281 for TC gait vs. −0.880±0.257 for regular gait, p=0.523, Fig. 1b). The relative COM velocity to the BOS was significantly lower during TC gait than in regular gait (0.038±0.018 vs. 0.190±0.029, p <0.001, Fig. 1c). Individuals were less stable during TC gait in comparison with regular gait at the same event (−0.201±0.053 vs. −0.041±0.037, p<0.001, Fig. 1d). Similar results were observed with COM position, velocity, and dynamic gait stability at LO: 1.421±0.249 vs. 1.350±0.166 and p=0.434 for position; 0.0057±0.024 vs. 0.228±0.032 and p<0.001 for velocity; and 0.308±0.054 vs. 0.466±0.040 and p<0.001 for dynamic gait stability (Fig. 1b–d). During stance phase, the COM motion trajectory was lower for TC gait than the regular gait (Fig. 1a). Both types of gait covered a similar range of COM position but COM velocity was lower during TC gait than the regular gait. Notably, COM during the regular gait continuously travelled forward relative to the BOS while it reversed the moving direction four times in TC gait. Overall, participants were less stable when practicing TC gait than in normal gait.
The COP displacement during TC gait was smaller in the anteroposterior direction (0.198±0.028 vs. 0.220±0.016cm, p=0.008, Fig. 1e–f) but greater in the mediolateral direction (0.125±0.033 vs. 0.037±0.013cm, p<0.001) comparing with the regular gait.
TC gait showed a significantly smaller peak moment on the sagittal plane (0.904±0.166 vs. 1.397±0.123Nm/kg, p<0.001) but larger moment on the transverse plane (0.188±0.100 vs. 0.097±0.039Nm/kg, p=0.047) at the ankle joint than the regular gait (Fig. 2a & c). The moment on all three planes was significantly larger during TC gait than in normal gait at the knee joint (1.388±0.342 vs. 0.657±0.134Nm/kg, p<0.001 for sagittal plane; 0.504±0.254 vs. 0.379±0.119Nm/kg, p=0.048 for frontal plane; and 0.474±0.104 vs. 0.207±0.063Nm/kg, p <0.001 for transverse plane, Fig. 2d–f). The hip joint on the frontal plane was higher during TC gait than the regular gait (1.561±0.404 vs. 1.389±0.337, p=0.049, Fig. 2h). Moment was comparable between the two distinct gaits at the ankle joint in the frontal plane and the hip joint in the sagittal and transverse planes (p>0.05 for all, Fig. 2b, g, &i).
Fig. 2.
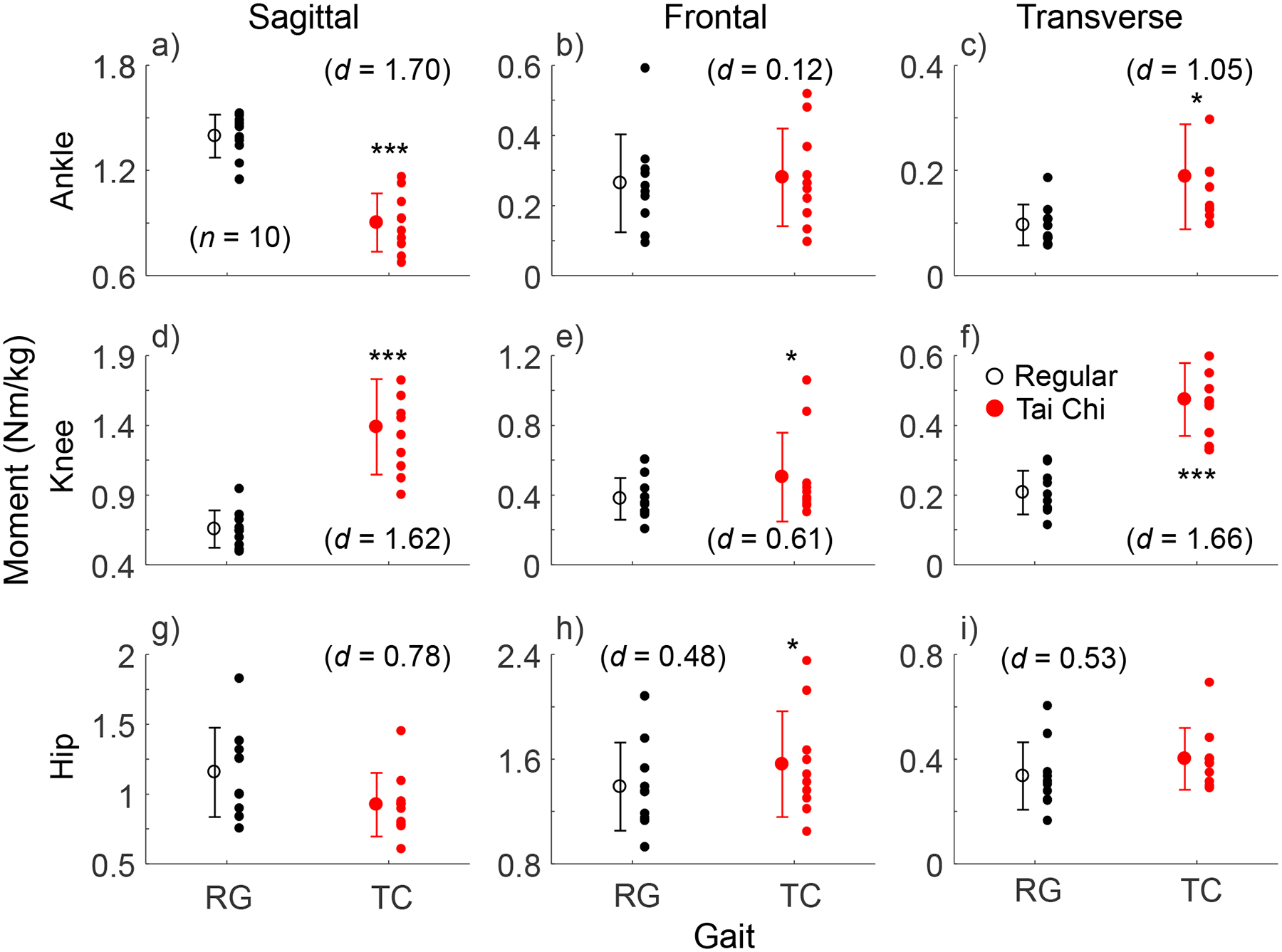
Comparisons of the magnitude of the peak joint moment at the ankle (a, b, and c), knee (d, e, and f), and hip (g, h, and i) on three planes (sagittal: first column; frontal: second column, and transverse: third column) between Tai-Chi gait (TC) and regular walking gait (RG). All moments were calculated using inverse dynamics based on an individualized biomechanical human model (Winter, 2009) and normalized to body mass (in Nm/kg). Both the group mean (± SD, the circle with error bars) and individual values (the scatter circles) are shown. The effect size of each comparison between gaits is displayed as Cohen’s d. ***: p < 0.001 vs. RG; *: p < 0.05 vs. RG.
DISCUSSION
Like any intervention, TC practice for falls prevention should be based on its soundly understood mechanisms. This study directly tackled the possible biomechanical mechanisms of TC practice reducing the risk of falls by improving body balance and leg muscle strength.
A few previous studies quantified TC gait in terms of the ground reaction force pattern, gait parameters, and COP trajectory during TC gait (Wu et al., 2004; Wu and Millon, 2008). Alike the present study, they reported slower gait speed, greater mediolateral COP displacement, and larger lateral shift of the body associated with TC gait (Wu et al., 2004). A unique contribution of the current study was the application of dynamic gait stability in TC gait. Our results revealed that individuals are less stable during TC gait than regular gait. A low stability could represent a challenge to the body’s postural control system and increase the risk of falling during TC gait. To respond to the challenge, the body must adaptively develop neuromuscular control strategies to maintain and improve body balance. Improvements in body balance could signify a reduced fall risk. From this perspective, TC practice reflects the overload practice principle (i.e., to increase the difficulty of tasks during practice). This could in part account for the observed TC-induced balance improvements among older adults in previous clinical trials (Lomas-Vega et al., 2017).
Consistent with previous studies (Wu and Millon, 2008), our study shows that the hip joint moment in the frontal plane was greater in TC gait than in the regular gait. Lateral stability has been associated with falls in older people (Rogers et al., 2001). The frontal-plane joint moment at the hip is significantly increased during TC gait compared with regular gait (Fig. 2h). This stimulation over a long-term training course likely strengthens hip abductors/adductors, which in turn improves the lateral stability and thus the fall risk. TC gait also requires larger moment in all three planes at the knee joint (Fig. 2d–f). As the knee joint plays a vital role in preventing falls, an increased knee joint moment capacity would reduce the risk of falls. Collectively, the increased moment at the lower limb joints provides sufficient limb support to prevent the body from collapsing should a perturbation occur. This may serve as another explanation of the mechanism of TC practice mitigating the risk of falls.
Our study has limitations. First, the sample size was small, possibly resulting in large variabilities in the outcome measures and affecting our findings. Second, not all our participants aged 65 or older and all of them are experienced TC practitioners. This may reduce the generalizability of the study among older adults and those with less TC experience. Despite the limitations, the results from this study will furnish preliminary evidence to justify further studies examining the biomechanical impact of individual TC forms on the human body.
Our study represents the first attempt to elucidate the biomechanical impact of TC practice on fall risk. A clear understanding of how each TC form affects body biomechanics will lay a solid scientific foundation for future efforts to optimize the effectiveness of TC practice on preventing falls.
Supplementary Material
ACKNOWLEDGEMENTS
This work was funded in part by grant K23AT009568 from the National Institutes of Health. The authors thank Caroline Simpkins for editing.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
The authors have no conflicts.
REFERENCES
- Bergland A, Jarnlo GB, Laake K, 2003. Predictors of falls in the elderly by location. Aging Clin Exp Res 15, 43–50. [DOI] [PubMed] [Google Scholar]
- de Leva P, 1996. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J. Biomech 29, 1223–1230. [DOI] [PubMed] [Google Scholar]
- Ding L, Yang F, 2016. Muscle weakness is related to slip-initiated falls among community-dwelling older adults. J. Biomech 49, 238–243. [DOI] [PubMed] [Google Scholar]
- Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL, 2018. Interventions to prevent falls in older adults: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 319, 1705–1716. [DOI] [PubMed] [Google Scholar]
- Hosseini L, Kargozar E, Sharifi F, Negarandeh R, Memari A-H, Navab E, 2018. Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: a randomized control trial. J Exerc Rehabil 14, 1024–1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagodinsky A, Fox J, Decoux B, Weimar W, Liu W, 2015. Biomechanical comparison of frontal plane knee joint momnet arms during normal and Tai Chi walking. J Phys Ther Sci 27, 2959–2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan C, Lai J-S, Wong M-K, Yu M-L, 1996. Cardiorespiratory function, flexibility, and body composition among geriatric tai chi chuan practitioners. Arch. Phys. Med. Rehabil 77, 612–616. [DOI] [PubMed] [Google Scholar]
- Li F-Z, Harmer P, Eckstrom E, Fitzgerald K, Chou L-S, Liu Y, 2019. Effectiveness of Tai Ji Quan vs multimodal and stretching exercise interventions for reducing injurious falls in older adults at high risk of falling: Follow-up analysis of a randomized clinical trial. JAMA Netw Open 2, e188280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F-Z, Harmer P, Fitzgerald K, Eckstrom E, Akers L, Chou L-S, Pidgeon D, Voit J, Winters-Stone K, 2018. Effectiveness of a therapeutic Tai Ji Quan intervention vs a multimodal exercise intervention to prevent falls among older adults at high risk of falling. JAMA Intern Med 178, 1301–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Kovaleski JE, Kepple TM, Wolfe J, Decoux B, McCarthy JP, Singh J, Lewis CE, 2016. Does Tai Chi gait reduce external knee adduction moment? J. Altern. Complement. Med 22, 818–823. [DOI] [PubMed] [Google Scholar]
- Lomas-Vega R, Obrero-Gaitan E, Molina-Ortega FJ, Del-Pino-Casado R, 2017. Tai Chi for risk of falls. A meta-analysis. J. Am. Geriatr. Soc 65, 2037–2043. [DOI] [PubMed] [Google Scholar]
- McCarthy M, 2016. Falls are leading cause of injury deaths among older people, US study finds. BMJ 354, i5190. [Google Scholar]
- Pai Y-C, Patton JL, 1997. Center of mass velocity-position predictions for balance control. J. Biomech 30, 347–354. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Yang F, Wening JD, Pavol MJ, 2006. Mechanisms of limb collapse following a slip among young and older adults. J. Biomech 39, 2194–2204. [DOI] [PubMed] [Google Scholar]
- Penn I-W, Sung W-H, Lin C-H, Chuang E, Chuang T-Y, Lin P-H, 2019. Effects of individualized Tai-Chi on balance and lower-limb strength in older adults. BMC Geriatrics 19, 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MW, Hedman LD, Johnson ME, Cain TD, Hanke TA, 2001. Lateral stability during forward-induced stepping for dynamic balance recovery in young and older adults. J Gerontol A Biol Sci Med Sci 56, M589–M594. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Fairhall NJ, W. GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE, 2019. Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2019, CD012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, 2003. Preventing falls in elderly persons. N Engl J Med 388, 42–49. [DOI] [PubMed] [Google Scholar]
- Winter DA, 2009. Biomechanics and Motor Control of Human Movement, 4th ed Wiley, Hoboken, NJ. [Google Scholar]
- Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ, 2003. Intense Tai Chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J. Am. Geriatr. Soc 51, 1693–1701. [DOI] [PubMed] [Google Scholar]
- Wu G, Liu W, Hitt J, Millon D, 2004. Spatial, temporal and muscle action patterns of Tai Chi gait. J. Electromyogr. Kinesiol 14, 343–354. [DOI] [PubMed] [Google Scholar]
- Wu G, Millon D, 2008. Joint kinetics during Tai Chi gait and normal walking gait in young and elderly Tai Chi Chuan practitioners. Clin. Biomech 23, 787–795. [DOI] [PubMed] [Google Scholar]
- Wu Y, MacDonald HV, Pescatello LS, 2016. Evaluating exercise prescription and insturctional methods used in Tai Chi studies aimed at improving balance in older adults: A systematic review. J. Am. Geriatr. Soc 64, 2074–2080. [DOI] [PubMed] [Google Scholar]
- Yang F, Anderson FC, Pai Y-C, 2007. Predicted threshold against backward balance loss in gait. J. Biomech 40, 804–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Bhatt T, Pai Y-C, 2009. Role of stability and limb support in recovery against a fall following a novel slip induced in different daily activities. J. Biomech 42, 1903–1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Pai Y-C, 2010. Role of individual lower limb joints in reactive stability control following a novel slip in gait. J. Biomech 43, 397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


