Abstract
Adverse local tissue reactions (ALTRs) were first associated with patients with failed metal-on-metal (MOM) surface replacements and total hip arthroplasty (THA). However, an increasing number of cases of ALTR in metal-on-polyethylene (MOP) THA patients are being reported. Clinically, ALTR appears as benign, aseptic masses or bursae in the periprosthetic tissues. Histopathologically, ALTRs are distinguished by an intense lymphocyte infiltrate, destruction of the synovial surfaces, widespread necrosis, and fibrin exudate. Tribocorrosion of modular junctions appears to be the cause of ALTR in MOP patients. The various tribocorrosion damage modes occurring at modular junctions produce metal ions and a diversity of particulates in relation to size, chemical composition and structure. The mechanisms by which these various products of tribocorrosion lead to ALTR are still a matter of considerable research. This review clarifies what constitutes ALTR, its relationship to implant factors, and highlights current methods for diagnosis and management of patients with ALTR in the setting of MOP THA.
Keywords: adverse local tissue reactions, taper corrosion, tribocorrosion, MOP, lymphocyte-dominated, metal ion levels
Over the last decade, the issues of tribocorrosion of modular junctions and associated tissue reactions have been among the leading concerns of orthopedic surgeons. Mechanically assisted crevice corrosion (MACC) is the all-encompassing term used to describe tribocorrosion processes occurring in the confined space between modular junction interfaces such as the head/neck junction of femoral hip prostheses [1–5]. Although the contemporary drivers of MACC are not fully understood, the process is certainly multifactorial involving implant material/design, surgical technique, and patient-related factors [5–8]. However, it has been well-established that tribocorrosion of modular junctions releases ionic and particulate corrosion products which often can trigger adverse local tissue reactions (ALTR). Such tissue reactions can cause pain, swelling, bone loss, and extensive tissue necrosis leading to complicated revision surgeries and considerable patient morbidity.
Historically, ALTR was first associated with patients with failed metal-on-metal (MOM) bearings [9–12]. More recently, as the usage of MOM total hip arthroplasty (THA) has waned, increasing numbers of ALTRs have been reported in metal-on-polyethylene bearings (MOP) associated with tribocorrosion at modular junctions [13–16]. In 2015, the prevalence of ALTR due to MACC at the head/neck junction was reported as 1.1% [17]. However in 2017, Hussey and McGrory reported a higher prevalence of 3.2% in a cross-sectional analysis of 1352 patients with surgeries performed between 2003 and 2012 [18]. It is the purpose of this review to help clarify what constitutes ALTR, its relationship to implant factors, and to highlight current methods for diagnosis and management of patients with ALTR in the setting of MOP THA.
What Constitutes an Adverse Local Tissue Reaction?
Soft tissue reactions around THA components with MOP bearings were recorded as early as 1988 [19]. Subsequently, lesions associated with MACC and severe implant wear have been described using various terms. Pseudotumor, aseptic lymphocyte-dominated vasculitis-associated lesions (ALVAL), trunnionosis, and metallosis are among the names used interchangeably in the literature as a descriptor and/or diagnosis leading to confusion and imprecision in the literature. Pseudotumor is a clinical and imaging descriptor referring to benign, aseptic masses and bursae associated with THA. ALVAL is a histologic description based on a scoring method for cell and tissue types present within the tissues [11] and was not intended to be a clinical diagnosis. Both pseudotumor and ALVAL were terms used extensively in association with failed MOM components [9,11,12]. Trunnionosis and metallosis are descriptive terms derived from gross observations at revision surgery. Trunnionosis refers to tribocorrosion damage at the femoral head-neck junction [20], whereas metallosis describes the stained appearance of the joint capsule and periprosthetic tissues due to large amounts of metal debris. However, it should be mentioned that the cellular response to this type of debris can vary widely. In our view, an ALTR is best defined as a variable combination of benign aseptic masses, ALVAL, soft and hard tissue necrosis and osteolysis in association with a joint replacement. Adverse reaction to metal debris (ARMD) is also used by some authors to describe cellular and tissue reactions in the periprosthetic tissue and in remote tissues. Nevertheless, there is no set convention for the usage of this terminology and care should therefore be exercised to use such terminology in a precise fashion.
In periprosthetic tissues, the cellular responses to particulates from wear and corrosion are driven by either the innate (nonspecific) or adaptive (specific) immune system. Chronic inflammation linked to the innate immunological response is characterized by a cellular infiltrate dominated by macrophages and foreign body giant cells (groups of fused macrophages) which can form particle-induced granulomas. In reaction to implant debris, macrophages increase pro-inflammatory factors and secrete chemokines and cytokines. Conversely, chronic inflammation driven by the adaptive response is controlled by T and B lymphocytes. Among the CD3+ T lymphocyte subpopulation are CD4+ helper T cells and CD8+ cytotoxic T cells. It is the T-helper cells that dominate implant-debris associated responses and have been described as Type IV delayed type hypersensitivity [21].
The most distinguishing feature of the histopathological appearance of ALTR is a marked chronic inflammation consisting of an intense lymphocytic infiltrate [11,14,22](Figure 1). Destruction of the synovial surface, inflammatory fibrin exudate and wide-spread necrosis are also prominent features of the periprosthetic soft tissues (Figure 2). Immunohistochemical staining has shown that the lymphocytic infiltrate is dominated by CD3+ T lymphocytes with a perivascular and diffuse distribution, while CD20+ B cells were mostly limited to perivascular sites [14](Figure 3). Plasmacytes and/or eosinophils can also be seen scattered within lymphocytic infiltrate in many cases. Unique to ALTR caused by MACC, numerous large particles of translucent, pale green chromium phosphate corrosion products may be present in the tissues, surrounded by giant cells, or within abundant fibrin exudate covering the surface of the joint capsule (Figure 4). Often, mild infiltrates of particle-laden macrophages containing metal and fine particles of corrosion products are present as well. However, it is important to note that the prominent histologic features of ALTR are the lymphocytic infiltrate along with widespread necrosis. At times, the extent of necrosis of the periprosthetic tissue is such that few areas of viable cells will be present. The remaining viable cells are most often infiltrates of lymphocytes. The primary histological and immunohistochemical nature of this inflammatory response to MACC of CoCrMo modular junctions has been shown to be similar to the ALTR reported with MOM surface replacements with no modular junctions [14], as well as with MOM THA with MACC at the head-neck and/or neck-stem junctions [23].
Figure 1.

The histopathological appearance of ALTR due to MACC is characterized by a chronic inflammation consisting of an intense infiltrate of perivascular and diffuse lymphocytes with destruction of the synovial surface. (Hematoxylin and eosin stain, x40)
Figure 2.

Widespread necrosis is also a distinguishing feature of ALTR. Perivascular and diffuse lymphocytes can be seen at the lower third of this photomicrograph. (Hematoxylin and eosin stain, x20)
Figure 3.
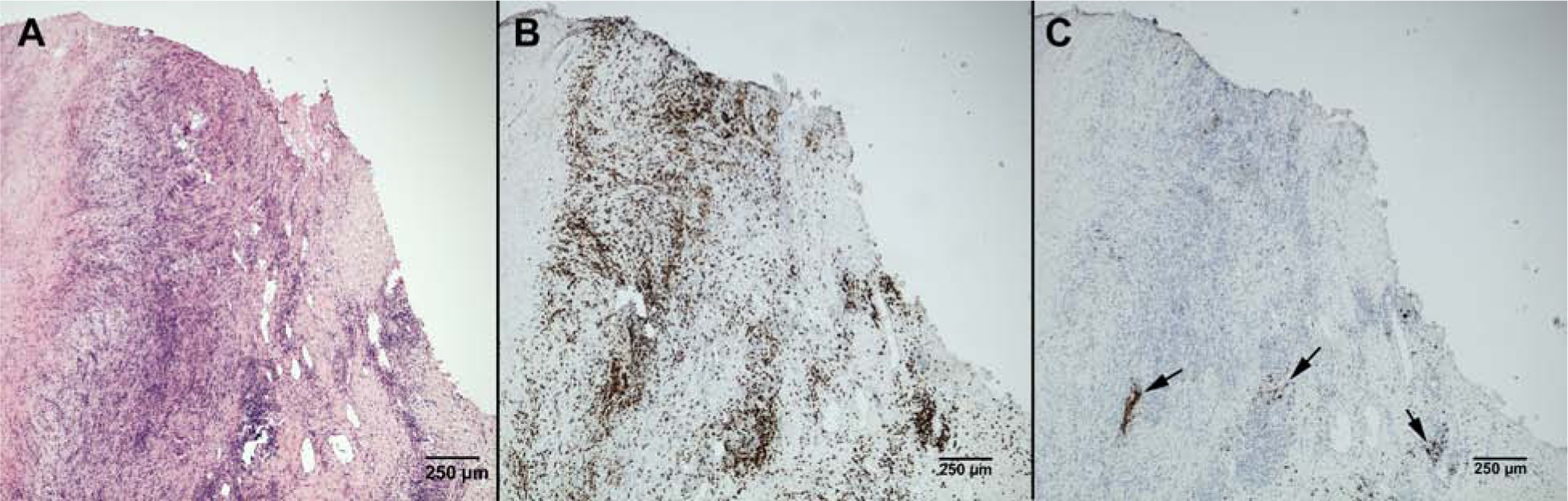
Serial sections of pseudocapsule obtained during revision of a corroded CoCrMo modular head in situ for 5 years. A: Hematoxylin and eosin staining shows an intense lymphocytic infiltrate. B: Immunohistochemical staining reveals this infiltrate to be dominated by CD3+ T lymphocytes with a perivascular and diffuse distribution. C: CD20+ B lymphocytes are few and limited to perivascular sites (arrows). (A-C: x40).
Figure 4.

Chromium phosphate corrosion products can often be found in the periprosthetic tissues revised for ALTR due to MACC. Here, a large (50 μm), translucent, pale green particle of chromium phosphate is seen surrounded by a giant cell. In the upper half of this image, a mild infiltrate of particle-laden macrophages containing fine particles of chromium phosphate is present. A giant cell containing fine particles of metal and chromium phosphate is seen in the left lower corner. Particle composition was confirmed using energy dispersive x-ray spectroscopy. (Hematoxylin and eosin stain, x400)
Research is ongoing, with no clear understanding to date as to the factors which influence patients to react in a variable fashion with either a macrophage- or lymphocyte-dominated tissue response to seemingly similar types and doses of wear and corrosion debris. The presence of extra-cellular and intra-cellular corrosion products within the periprosthetic tissue have been linked with the presence of perivascular and diffuse lymphocytic infiltrates, suggesting that macrophages laden with corrosion particles may be involved in the formation of these lymphocytic infiltrates [23]. Results of in vitro studies looking at the effects of cobalt and chromium ions on macrophages and the migration of lymphocytes showed that Co2+ and Cr3+ were capable of stimulating the migration of T, but not B, lymphocytes in the absence of cytokines/chemokines [24]. These results may help to explain the T cell/B cell ratio seen in ALTR periprosthetic tissues. Further, a recent study has shown that the responses to metal implant debris are largely dependent on activation of danger signaling (the inflammasome/caspase-1) with subsequent production of pro-inflammatory cytokines (IL-17A/F) by CD4+ T cells as a possible pathway for the in vivo transition from metal-delayed type hypersensitivity resistance to susceptibility [25].
The Relationship between the Implant and ALTR
It is the process of MACC at modular junctions that appears to be the common denominator for the occurrence of ALTR associated with MOP THA. MACC is not limited to the head-neck junction; it can also occur at the neck-stem tapers of dual modularity implants [13–16]. In the absence of a CoCrMo component in the THA reconstruction, ALTR is rarely reported. The onset of micromotion between the trunnion and head leads to fretting and fretting corrosion (i.e., MACC). Additionally, distinct damage modes have been identified at the interfaces between CoCrMo or Ti6Al4V femoral stems mated with CoCrMo heads [6]. These damage modes were categorized as mechanically dominated, chemically dominated, or a combination of both. Among the mechanically dominated damage modes are plastic deformation, fretting, and material transfer. Pitting corrosion, etching, intergranular corrosion, phase boundary corrosion, and column damage are examples of chemically-dominated damage modes. Fretting corrosion, formation of thick oxide films, and imprinting are the result of both mechanical and chemical processes [6,26,27]. The occurrence and extent of damage caused by the different modes is dependent on implant material on both sides of the head/neck couple. Recent studies have shown that even a fine local inhomogeneity in the implant alloy microstructure and chemical composition can cause an increased risk of corrosion and higher metal ion release rate [26,27]. Considerable variability in CoCrMo alloy microstructure has been observed in retrieved hip implants, even though the alloy conforms to ASTM standards. These microstructural features appear to dictate corrosion modes [26].
Among other factors contributing to the occurrence and magnitude of specific damage modes are surface topography, flexural rigidity, femoral offset, angular mismatch, and gross design factors (e.g., taper length, geometry, tolerances) [5,7,28–30]. In terms of taper topography, tapers with higher circumferential machining mark peaks appear to have slower taper damage progression [8,31]. Surgical assembly and patient factors (e.g., activity, BMI) may also contribute to these modes of damage [7,31]. With respect to surgical assembly, it has been shown that cleaning of the taper before assembly reduces the risk of fretting corrosion [32]. It is therefore recommended to clean the trunnion and to remove potential contaminants from the surface prior to impaction of the head. However, to date there is no consensus as to how much load should be applied during femoral head/neck assembly, or how many mallet strikes should be performed [33]. It is essential that enough load is applied to ensure stable fixation and to prevent the onset of micro-motion and subsequent fretting, but without risking a fracture of the femur during impaction. The optimal assembly load and technique is still subject of ongoing research [32,34–37].
The various damage modes produce a diversity of particulates that may directly affect cellular responses. Particulates are released mainly in the form of micro- and nano-particles, and oxides composed of cobalt and chromium. Ions of different valences are also produced [38]. Metallo-organic complexes can also be formed when metal ions interact with organic species such as proteins or blood. Also, depending on the mechanism of debris formation, different intermediate products, such as metal-protein complexes, may also be generated. The size, chemical composition and structure of particles may lead to the observed variety of cellular responses (macrophage-dominant, lymphocyte-dominant, or mixed cellular). In fact, macrophage-dominant tissue reactions are observed histologically in the resected periprosthetic tissues of many patients revised for ALTR due to MACC. Currently, there has been no link established between the different types of implant debris generated within modular junctions and the resulting type or extent of periprosthetic tissue response. This uncertainty has led to a broader definition of ALTR in the literature, viewing ALTR as a histological spectrum [23,39]. However, as stated earlier, the histologic appearance of the periprosthetic tissues of patients with MACC and aseptic masses (pseudotumors, fluid) is lymphocyte-dominated [13,16,40].
As noted above, cobalt and chromium ions are also released as CoCrMo alloys undergo tribocorrosion. It has been well established that patients hosting joint replacements have higher levels of metal in serum, synovial fluid, and whole blood compared to those without an implant [41,42]. In fact, patients with well-functioning primary MOP total hip replacements followed for 10 years postoperative had elevated serum metal levels; although the mean serum cobalt was never above 0.8 ng/mL [43]. Metal levels in well-functioning arthroplasties are also related to the bearing surface, with higher levels seen in patients with MOM bearings compared to MOP [44–46]. Under severe tribocorrosion conditions at modular head/neck junction, cobalt and chromium levels can be greatly elevated with serum cobalt elevated to a greater degree than serum chromium [40,47–49]. A caveat needs to be mentioned with this literature; metal measurements in body fluids, including whole blood, serum, and synovial fluid, are laboratory dependent due to the sensitivity and calibration of each laboratory’s equipment and the particular methodology used in specimen processing [46].
The Diagnosis of ALTR
The diagnosis of ALTR caused by MACC can be challenging as its symptoms can mimic periprosthetic joint infection, instability, or aseptic loosening [47]. Recurrent dislocation or weakness secondary to abductor muscle destruction can also be presenting complaints in patients with ALTR due to MACC. Patients should be evaluated for ALTR when presenting with postoperative pain in the presence of well-fixed implants and a negative workup for infection. Serum metal levels are a very effective screening tool. Recent studies have concluded that threshold values of serum cobalt over 1 ng/mL (1ppb) and cobalt/chromium ratios greater than 2 are reliable indicators of an ALTR [40,47–49]. It is important to note that the serum metal level threshold for this diagnosis is considerably less than for patients with MOM bearings [40,50] where serum cobalt levels typically exceed 1 ppb in patients with well-functioning implants. However, the clinician should not rely exclusively on one diagnostic test as false positives and false negatives are possible; other modalities, particularly cross-sectional imaging (ultrasound or metal artifact reduction sequence-magnetic resonance imaging (MARS-MRI)) can be confirmative and are recommended in the workup of a patient with a suspected ALTR [47]. Cross-sectional imaging findings of large fluid collections, soft tissue masses, thickened pseudocapsule, or destruction of the abductor musculature are consistent with the diagnosis of ALTR [51].
Screening for periprosthetic joint infection (PJI) is also recommended by obtaining an erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and joint fluid aspiration. ESR and CRP are occasionally elevated in patients with ALTR; however, if both are negative, then PJI is unlikely [40,47]. Joint fluid aspirate that is cloudy, dark, or metal stained should be considered suspicious of ALTR. PJI is ruled out when synovial fluid white blood cell counts are below 3000 wbc/uL, the differential is less than 80%, and the cultures are negative [40,47]. A manual count is recommended in the setting of possible ALTR due to MACC as cellular debris may lead to falsely elevated cell counts in automated cell counting machines.
Management of Patients
Once a diagnosis of ALTR is made, surgical treatment is generally recommended. Decisions concerning when to operate and what to revise can also be challenging. Revision surgery should not be delayed to avoid involvement, or further compromise, of the abductor musculature. When the trunnion appears macroscopically intact and the implant is well-fixed, many authors have reported good clinical results by exchanging the damaged CoCrMo head with an alumina ceramic head and titanium sleeve [7,13,40]. After a CoCrMo to alumina ceramic head exchange, Plummer et al. reported postoperative metal ion levels after a mean of 2.7 years with a significant reduction in serum cobalt levels with time from 11.6 ppb to 0.33 ppb [40]. However, in a study of 40 consecutive revision surgeries for ALTR in 39 patients where ceramic heads were used in 34 hips, Kwon et al. reported 25% early complications (dislocation (15%), infection (7%), and pseudotumor recurrence (3%)) and a 10% reoperation rate [52]. Considering the low subject numbers in these studies, more data and longer term follow-up studies are warranted.
Summary
ALTR is related to the summation of debris released from bearing surfaces and modular junctions through tribocorrosion mechanisms. The prevalence of ALTR due to MACC in patients with MOP THA may be as high as, or even higher than, the prevalence of PJI in primary THA. On cross-sectional imaging, ALTR appears as a benign, aseptic mass or bursa in the periprosthetic tissues with or without osteolysis. Histopathologically, ALTR is distinguished by an intense lymphocyte infiltrate, destruction of the synovial surfaces, widespread necrosis, a fibrin exudate and possibly osteolysis. The various damage modes occurring at modular junctions produce metal ions and a diversity of particulates in relation to size, chemical composition and structure. The mechanisms by which these various products of tribocorrosion lead to ALTR are still a matter of considerable research. Patients presenting with postoperative pain in the presence of well-fixed implants and a negative infection workup should be evaluated for ALTR. While the diagnosis of ALTR due to MACC can be challenging, serum metal levels and cross-sectional imaging have proven to be effective diagnostic modalities. Timely revision surgery is recommended to avoid progressive damage to the abductor musculature and soft tissue envelop of the hip. When there is considerable soft tissue damage, revision surgery can be particularly challenging, occasionally necessitating the use of a constrained cup or other methods to mitigate the risk of instability. When femoral stems are well-fixed and the trunnion appears macroscopically intact, exchange of the damaged CoCrMo head with an alumina ceramic head and titanium sleeve has shown promising short-term results.
Supplementary Material
Acknowledgements
This work was funded by NIH/NIAMS grant R01AR070181.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Collier JP, Surprenant VA, Jensen RE, Mayor MB, Surprenant HP. Corrosion between the components of modular femoral hip prostheses. J Bone Joint Surg Br 1992;74:511–7. [DOI] [PubMed] [Google Scholar]
- [2].Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations. The effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res 1993;27:1533–44. [DOI] [PubMed] [Google Scholar]
- [3].Urban RM, Jacobs JJ, Gilbert JL, Galante JO. Migration of corrosion products from modular hip prostheses. Particle microanalysis and histopathological findings. J Bone Joint Surg Am 1994;76:1345–59. [DOI] [PubMed] [Google Scholar]
- [4].Jacobs JJ, Urban RM, Gilbert JL, Skipor AK, Black J, Jasty M, et al. Local and distant products from modularity. Clin Orthop Relat Res 1995;319:94–105. [PubMed] [Google Scholar]
- [5].Pourzal R, Lundberg HJ, Hall DJ, Jacobs JJ. What Factors Drive Taper Corrosion? Journal of Arthroplasty 2018;33:2707–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hall DJ, Pourzal R, Lundberg HJ, Mathew MT, Jacobs JJ, Urban RM. Mechanical, chemical and biological damage modes within head-neck tapers of CoCrMo and Ti6Al4V contemporary hip replacements: Damage Modes In THR Modular Junctions. Journal of Biomedical Materials Research Part B: Applied Biomaterials 2018;106:1672–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Berstock JR, Whitehouse MR, Duncan CP. Trunnion corrosion: what surgeons need to know in 2018. Bone Joint J 2018;100-B:44–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pourzal R, Hall DJ, Ha NQ, Urban RM, Levine BR, Jacobs JJ, et al. Does Surface Topography Play a Role in Taper Damage in Head-neck Modular Junctions? Clin Orthop Relat Res 2016;474:2232–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Willert H-G, Buchhorn GH, Dipl-Ing, Fayyazi A, Flury R, Windler M, et al. Metal-on-Metal Bearings and Hypersensitivity in Patients with Artificial Hip Joints: A Clinical and Histomorphological Study. JBJS 2005;87:28–36. [DOI] [PubMed] [Google Scholar]
- [10].Jacobs JJ, Urban RM, Hallab NJ, Skipor AK, Wimmer MA. Metal-on-metal bearings. J AAOS 2009;17:69–76. [DOI] [PubMed] [Google Scholar]
- [11].Campbell P, Ebramzadeh E, Nelson S, Takamura K, Smet K, Amstutz HC. Histological Features of Pseudotumor-like Tissues from Metal-on-Metal Hips. Clinical Orthopaedics and Related Research® 2010;468:2321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, et al. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. Journal of Bone & Joint Surgery, British Volume 2010;92:356–361. [DOI] [PubMed] [Google Scholar]
- [13].Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am 2012;94:1655–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hall DJ, Pourzal R, Della Valle CJ, Galante JO, Jacobs JJ, Urban RM. Corrosion of Modular Junctions in Femoral and Acetabular Components for Hip Arthroplasty and Its Local and Systemic Effects. STP1591, ASTM International, West Conshohocken, PA: 2015, p. 410–27. [Google Scholar]
- [15].Cooper HJ, Urban RM, Wixson RI, Meneghini RM, Jacobs JJ. Adverse Local Tissue Reactions Arising from Corrosion at the Neck-Body Junction in a Dual Taper Stem with a CoCr Modular Neck. The Journal of Bone & Joint Surgery (AM) 2013;95:865–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cooper HJ. The local effects of metal corrosion in total hip arthroplasty. Orthop Clin North Am 2014;45:9–18. [DOI] [PubMed] [Google Scholar]
- [17].McGrory BJ, MacKenzie J, Babikian G. A High Prevalence of Corrosion at the Head–Neck Taper with Contemporary Zimmer Non-Cemented Femoral Hip Components. The Journal of Arthroplasty 2015;30:1265–8. [DOI] [PubMed] [Google Scholar]
- [18].Hussey DK, McGrory BJ. Ten-Year Cross-Sectional Study of Mechanically Assisted Crevice Corrosion in 1352 Consecutive Patients with Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty 2017;32:2546–51. [DOI] [PubMed] [Google Scholar]
- [19].Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J Bone Joint Surg Am 1988;70:1238–42. [PubMed] [Google Scholar]
- [20].Mistry JB, Chughtai M, Elmallah RK, Diedrich A, Le S, Thomas M, et al. Trunnionosis in total hip arthroplasty: a review. Journal of Orthopaedics and Traumatology 2016;17:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hallab NJ, Jacobs JJ. Chemokines Associated with Pathologic Responses to Orthopedic Implant Debris. Front Endocrinol (Lausanne) 2017;8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Krenn V, Perino G. Histological diagnosis of implant-associated pathologies. Berlin: Springer-Verlag GmbH Germany; 2017. [Google Scholar]
- [23].Perino G, Ricciardi BF, Jerabek SA, Martignoni G, Wilner G, Maass D, et al. Implant based differences in adverse local tissue reaction in failed total hip arthroplasties: a morphological and immunohistochemical study. BMC Clin Pathol 2014;14:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Baskey SJ, Lehoux EA, Catelas I. Effects of cobalt and chromium ions on lymphocyte migration. J Orthop Res 2017;35:916–24. [DOI] [PubMed] [Google Scholar]
- [25].Samelko L, Caicedo MS, Jacobs J, Hallab NJ. Transition from metal-DTH resistance to susceptibility is facilitated by NLRP3 inflammasome signaling induced Th17 reactivity: Implications for orthopedic implants. PLoS ONE 2019;14(1):e0210336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Pourzal R, Hall DJ, Ehrich J, McCarthy SM, Mathew MT, Jacobs JJ, et al. Alloy Microstructure Dictates Corrosion Modes in THR Modular Junctions. Clinical Orthopaedics & Related Research 2017;475:3026–30–3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hall DJ, McCarthy SM, Ehrich J, Urban RM, Fischer A, Lundberg HJ, et al. Imprinting and Column Damage on CoCrMo Head Taper Surfaces in Total Hip Replacements In: Mihalko WM, Lemons JE, Greenwald AS, Kurtz SM, editors. Symposium on Beyond the Implant: Retrieval Analysis Methods for Implant Surveillance, West Conshohocken, Pa. 19428–2959: ASTM International; 2018, p. 131–55. [Google Scholar]
- [28].Kocagöz SB, Underwood RJ, Sivan S, Gilbert JL, MacDonald DW, Day JS, et al. Does taper angle clearance influence fretting and corrosion damage at the head–stem interface? A matched cohort retrieval study. Seminars in Arthroplasty 2013;24:246–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Porter DA, Urban RM, Jacobs JJ, Gilbert JL, Rodriguez JA, Cooper HJ. Modern Trunnions Are More Flexible: A Mechanical Analysis of THA Taper Designs. Clin Orthop Relat Res 2014;472:3963–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pennock AT, Schmidt AH, Bourgeault CA. Morse-type tapers: factors that may influence taper strength during total hip arthroplasty. J Arthroplasty 2002;17:773–8. [DOI] [PubMed] [Google Scholar]
- [31].Lundberg HJ, Ha NQ, Hall DJ, Urban RM, Levine BR, Pourzal R. Contact Mechanics and Plastic Deformation at the Local Surface Topography Level After Assembly of Modular Head-Neck Junctions in Modern Total Hip Replacement Devices In: Greenwald AS, Kurtz SM, Lemons JE, Mihalko WM, editors. Modularity and Tapers in Total Joint Replacement Devices, West Conshohocken, PA: ASTM International; 2015, p. 59–82. [Google Scholar]
- [32].Krull A, Morlock MM, Bishop NE. The Influence of Contamination and Cleaning on the Strength of Modular Head Taper Fixation in Total Hip Arthroplasty. The Journal of Arthroplasty 2017;32:3200–5. [DOI] [PubMed] [Google Scholar]
- [33].Marinier M, Edmiston TA, Kearns S, Hannon CP, Levine BR. A Survey of the Prevalence of and Techniques to Prevent Trunnionosis. Orthopedics 2018;41:e557–62. 10.3928/01477447-20180524-03. [DOI] [PubMed] [Google Scholar]
- [34].Rehmer A, Bishop NE, Morlock MM. Influence of assembly procedure and material combination on the strength of the taper connection at the head-neck junction of modular hip endoprostheses. Clin Biomech (Bristol, Avon) 2012;27:77–83. [DOI] [PubMed] [Google Scholar]
- [35].Heiney JP, Battula S, Vrabec GA, Parikh A, Blice R, Schoenfeld AJ, et al. Impact magnitudes applied by surgeons and their importance when applying the femoral head onto the Morse taper for total hip arthroplasty. Arch Orthop Trauma Surg 2009;129:793–6. [DOI] [PubMed] [Google Scholar]
- [36].Noble P, Foley E, Simpson J, Gold J, Choi J, Ismaily S, et al. Inter-surgeon variability in the assembly of modular head-neck tapers in THA via the posterior approach. Orthopaedic Proceedings 2017;99-B:59–59. 10.1302/1358-992X.99BSUPP_5.ISTA2016-059. [DOI] [Google Scholar]
- [37].Scholl L, Schmidig G, Faizan A, TenHuisen K, Nevelos J. Evaluation of surgical impaction technique and how it affects locking strength of the head-stem taper junction. Proc Inst Mech Eng H 2016;230:661–7. [DOI] [PubMed] [Google Scholar]
- [38].Bijukumar DR, Segu A, Souza JCM, Li X, Barba M, Mercuri LG, et al. Systemic and local toxicity of metal debris released from hip prostheses: A review of experimental approaches. Nanomedicine 2018;14:951–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ricciardi BF, Nocon AA, Jerabek SA, Wilner G, Kaplowitz E, Goldring SR, et al. Histopathological characterization of corrosion product associated adverse local tissue reaction in hip implants: a study of 285 cases. BMC Clin Pathol 2016;16:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Plummer DR, Berger RA, Paprosky WG, Sporer SM, Jacobs JJ, Della Valle CJ. Diagnosis and Management of Adverse Local Tissue Reactions Secondary to Corrosion at the Head-Neck Junction in Patients with Metal on Polyethylene Bearings. The Journal of Arthroplasty 2016;31:264–8. [DOI] [PubMed] [Google Scholar]
- [41].Skipor AK, Campbell PA, Patterson LM, Amstutz HC, Schmalzried TP, Jacobs JJ. Serum and urine metal levels in patients with metal-on-metal surface arthroplasty. J Mater Sci Mater Med 2002;13:1227–34. [DOI] [PubMed] [Google Scholar]
- [42].Hartmann A, Hannemann F, Lützner J, Seidler A, Drexler H, Günther K-P, et al. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearing–systematic review of clinical and epidemiological studies. PLoS ONE 2013;8:e70359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Levine BR, Hsu AR, Skipor AK, Hallab NJ, Paprosky WG, Galante JO, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am 2013;95:512–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Rasquinha VJ, Ranawat CS, Weiskopf J, Rodriguez JA, Skipor AK, Jacobs JJ. Serum metal levels and bearing surfaces in total hip arthroplasty. J Arthroplasty 2006;21:47–52. [DOI] [PubMed] [Google Scholar]
- [45].Dahlstrand H, Stark A, Wick MC, Anissian L, Hailer NP, Weiss RJ. Comparison of metal ion concentrations and implant survival after total hip arthroplasty with metal-on-metal versus metal-on-polyethylene articulations. Acta Orthop 2017;88:490–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Barlow BT, Ortiz PA, Boles JW, Lee Y-Y, Padgett DE, Westrich GH. What Are Normal Metal Ion Levels After Total Hip Arthroplasty? A Serologic Analysis of Four Bearing Surfaces. J Arthroplasty 2017;32:1535–42. [DOI] [PubMed] [Google Scholar]
- [47].Della Valle CJ, Calkins TE, Jacobs JJ. Diagnosing Taper Corrosion: When Is It the Taper and When Is It Something Else? J Arthroplasty 2018;33:2712–5. [DOI] [PubMed] [Google Scholar]
- [48].Kwon Y-M, MacAuliffe J, Arauz PG, Peng Y. Sensitivity and Specificity of Metal Ion Level in Predicting Adverse Local Tissue Reactions Due to Head-Neck Taper Corrosion in Primary Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty 2018;33:3025–9. [DOI] [PubMed] [Google Scholar]
- [49].Fillingham YA, Della Valle CJ, Bohl DD, Kelly MP, Hall DJ, Pourzal R, et al. Serum Metal Levels for Diagnosis of Adverse Local Tissue Reactions Secondary to Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty 2017;32:S272–7. [DOI] [PubMed] [Google Scholar]
- [50].Chalmers BP, Perry KI, Taunton MJ, Mabry TM, Abdel MP. Diagnosis of adverse local tissue reactions following metal-on-metal hip arthroplasty. Curr Rev Musculoskelet Med 2016;9:67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Morozov PP, Sana M, McGrory BJ, Farraher SW, Abrahams TG. Comparison of Pre-Revision Magnetic Resonance Imaging and Operative Findings in Mechanically Assisted Crevice Corrosion in Symptomatic Metal-on-Polyethylene Total Hip Arthroplasties. J Arthroplasty 2017;32:2535–45. [DOI] [PubMed] [Google Scholar]
- [52].Kwon Y-M, Rossi D, MacAuliffe J, Peng Y, Arauz P. Risk Factors Associated With Early Complications of Revision Surgery for Head-Neck Taper Corrosion in Metal-on-Polyethylene Total Hip Arthroplasty. J Arthroplasty 2018;33:3231–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


